(Yes - as an intern I didn't know how to forward the pagers)
#FOAMed #MedTwitter #July1st
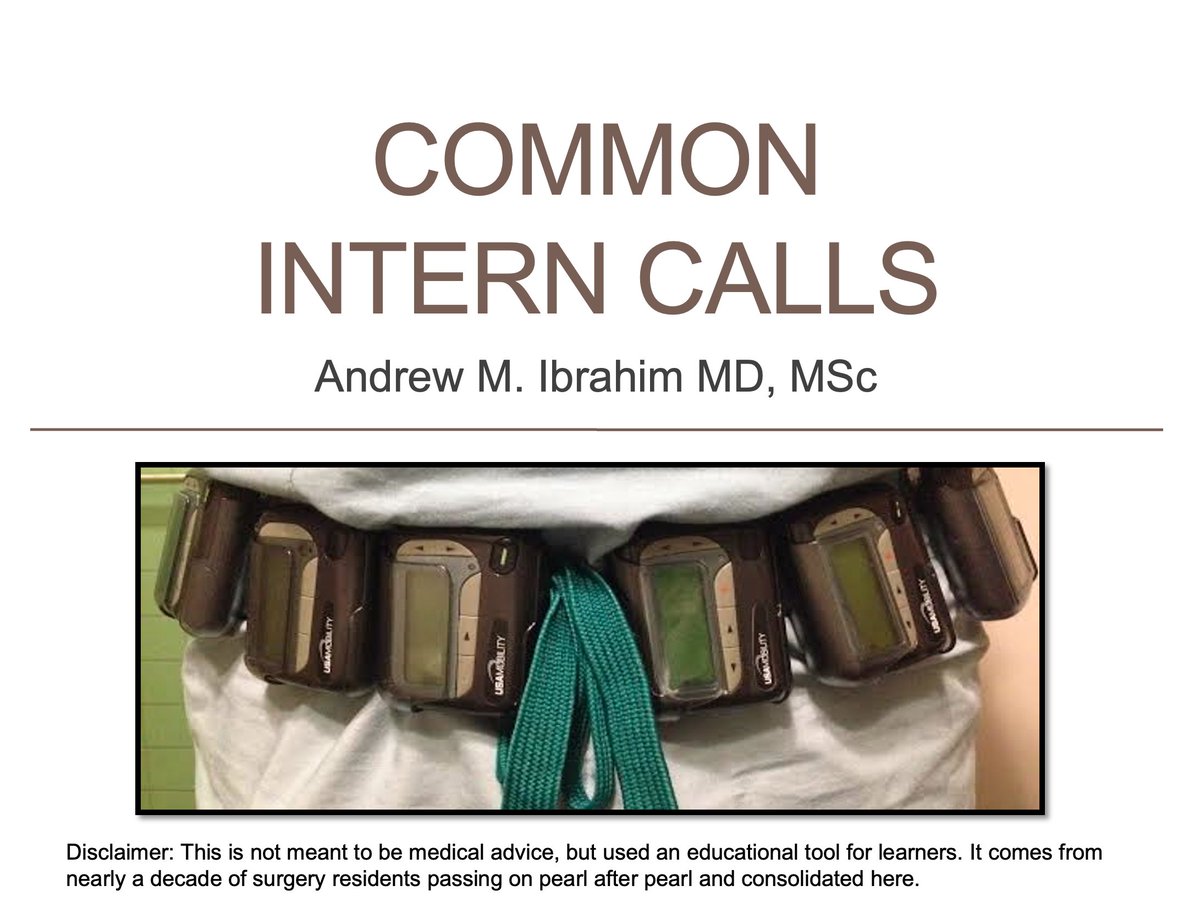
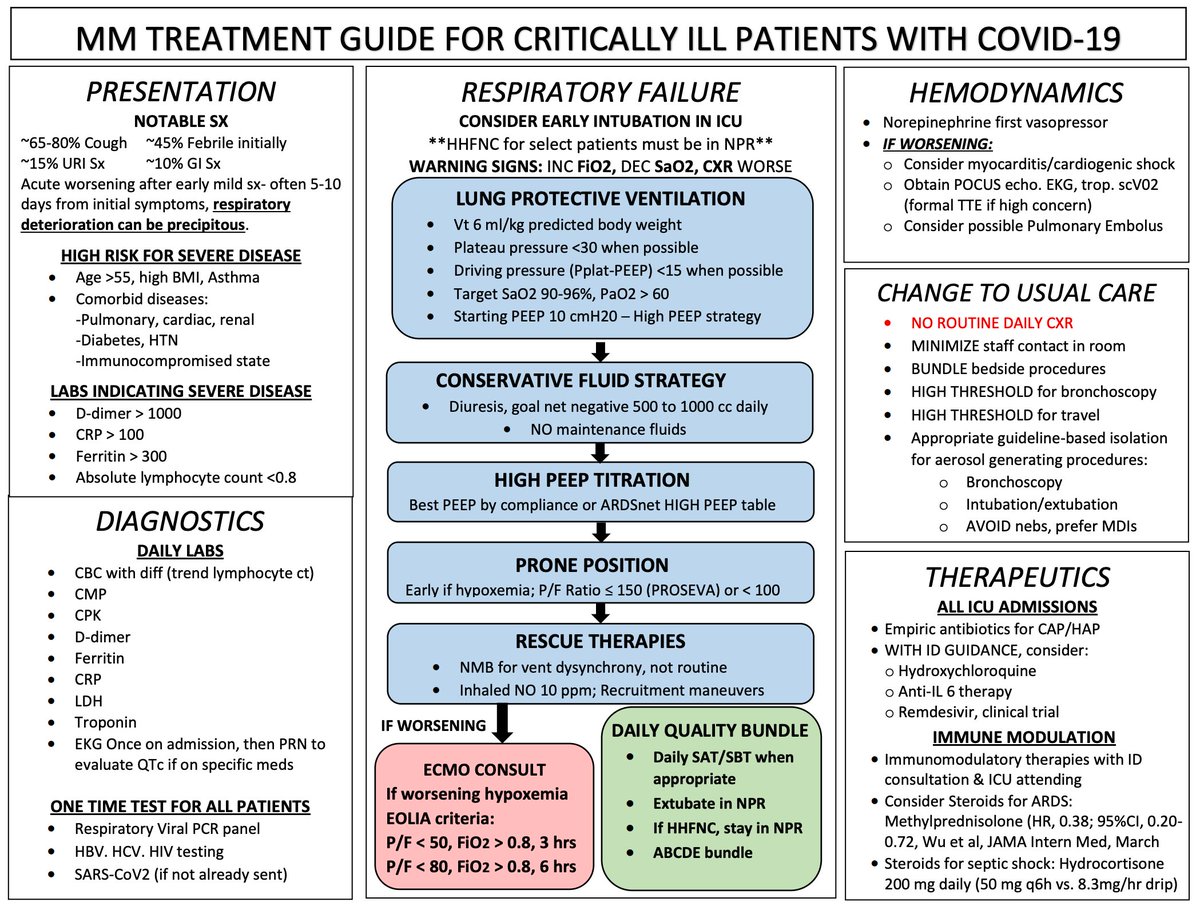
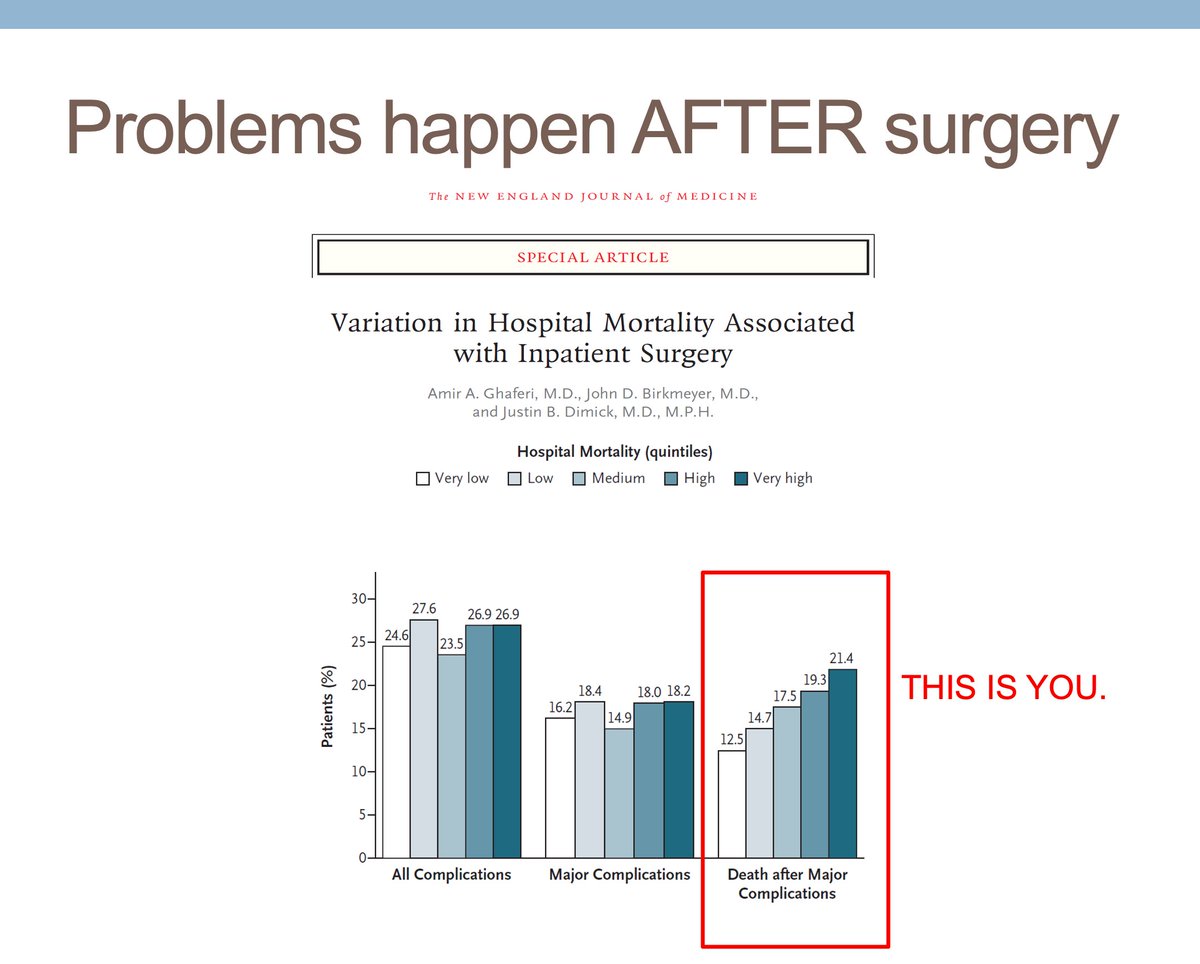
nejm.org/doi/full/10.10…
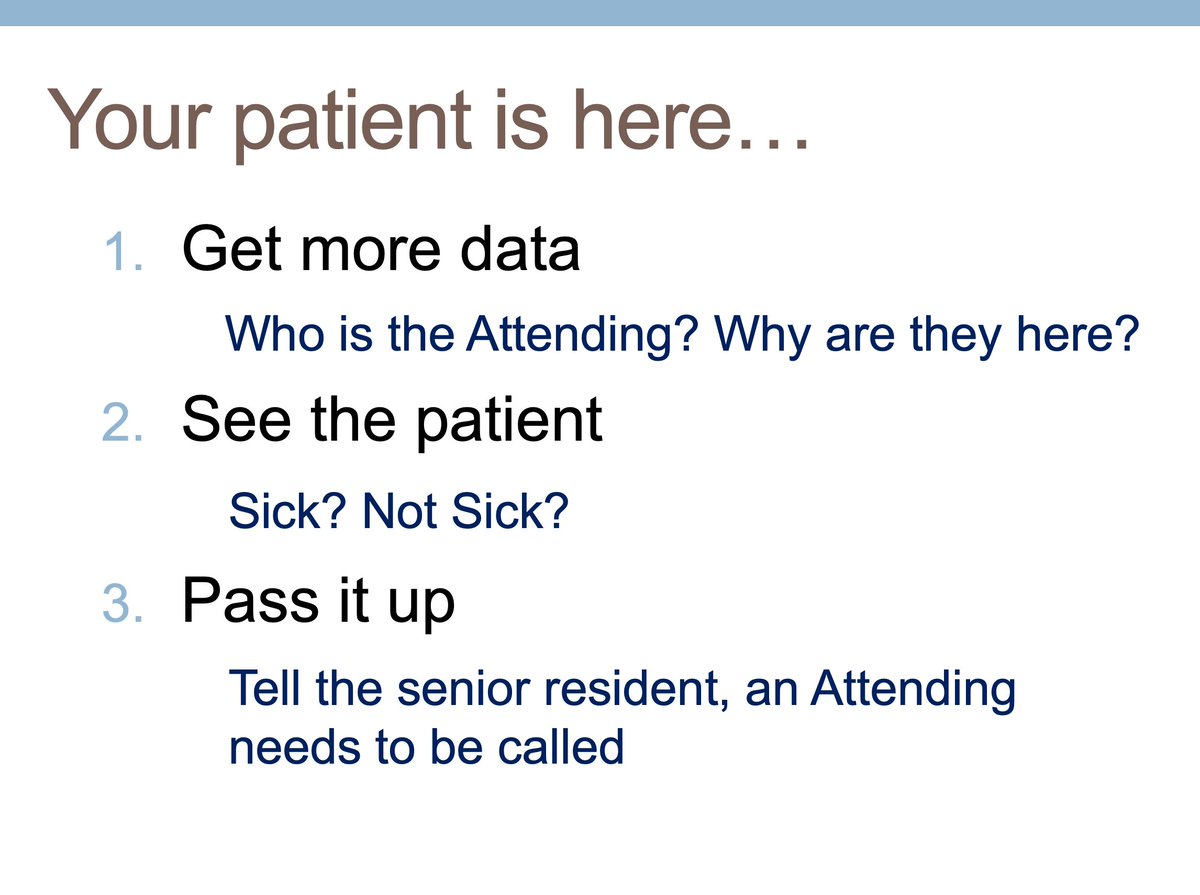
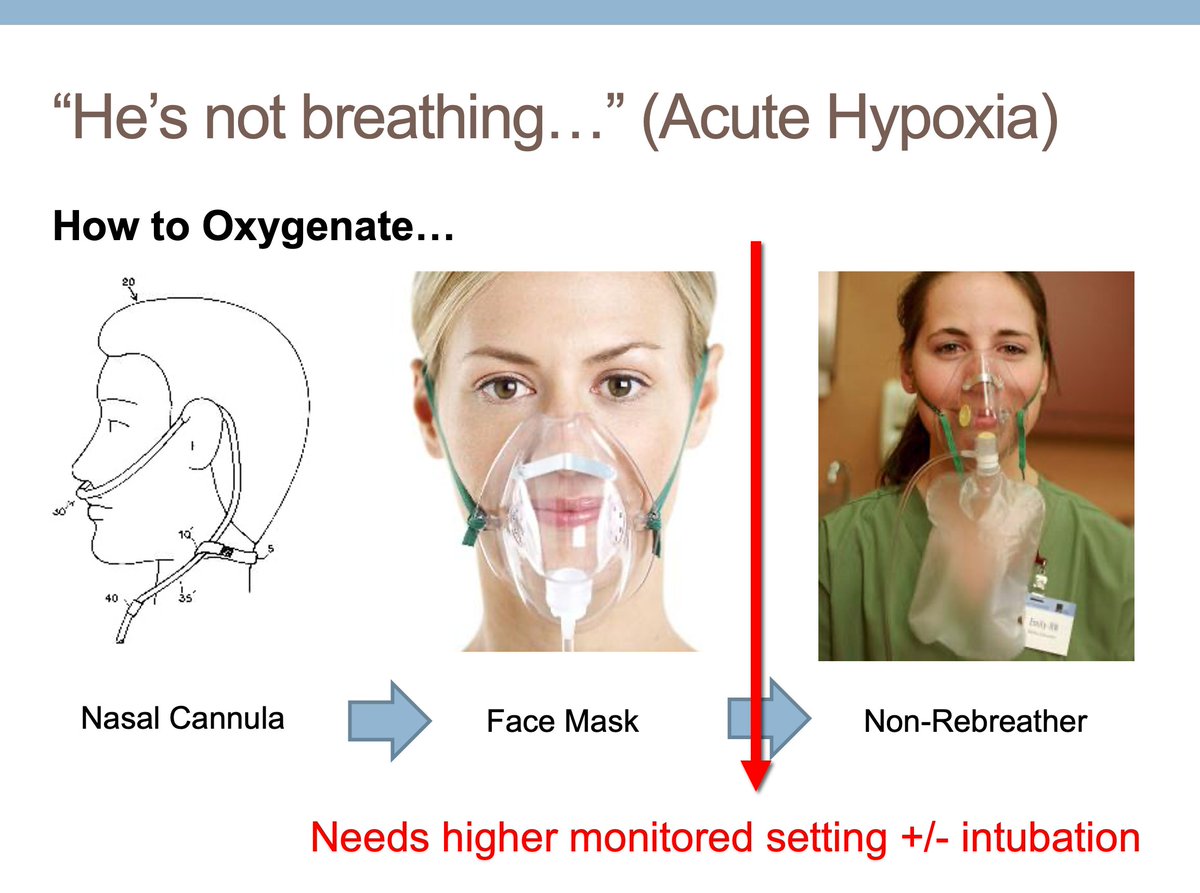
1. Get more Data
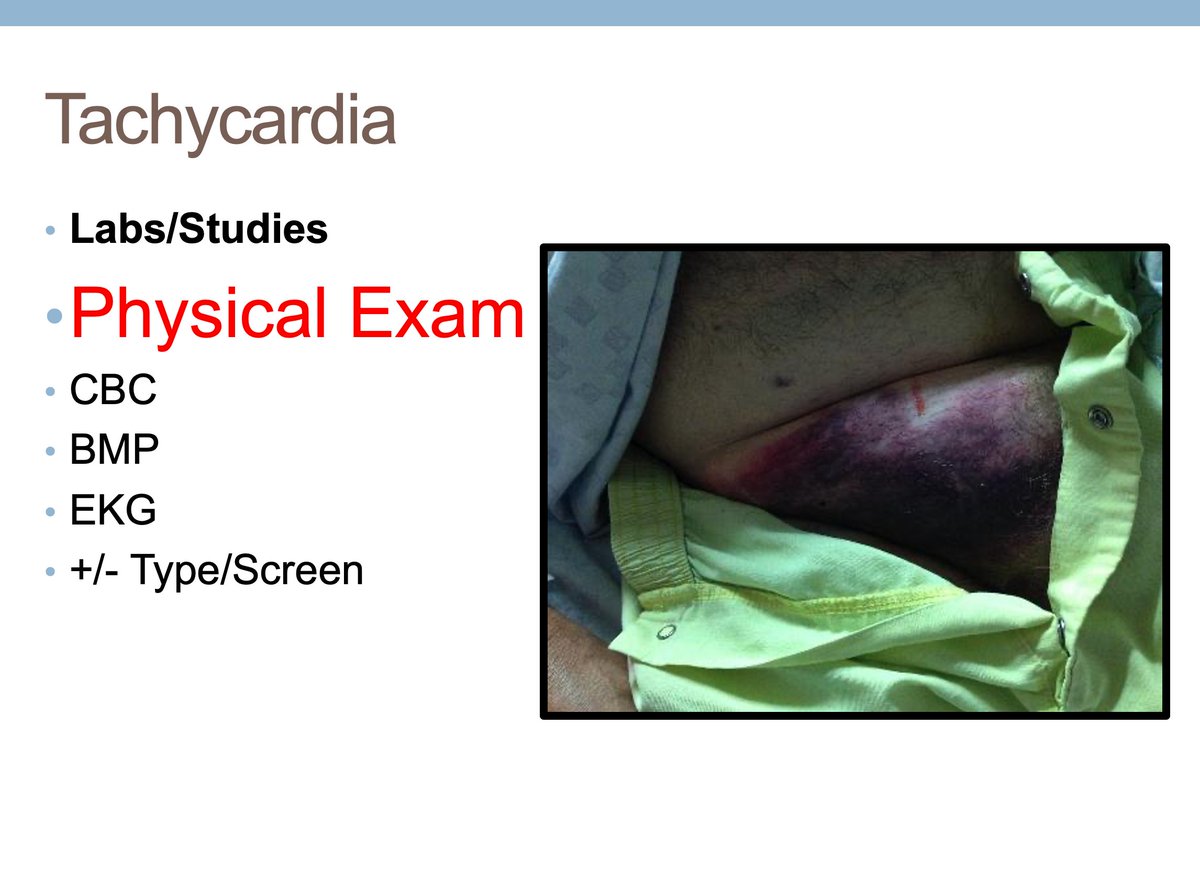
2. See the Patient
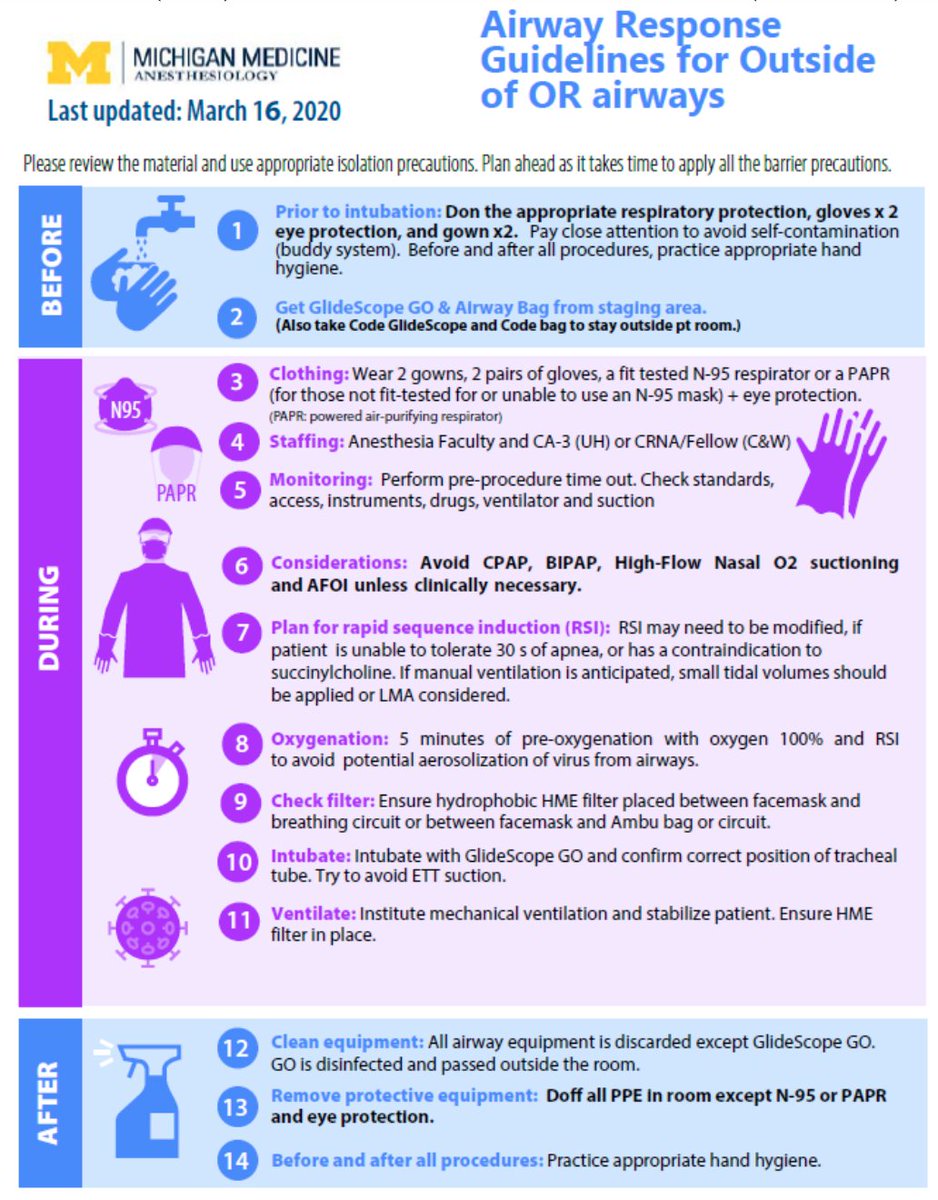
3. Pass it up
#FOAMED #MedTwitter