Interesting thread on possible reasons for resurgence of cases in NY & Madrid.
Some useful observations but several key flaws.
Quick thread.
Some useful observations but several key flaws.
Quick thread.
https://twitter.com/_MiguelHernan/status/1304424019450630144
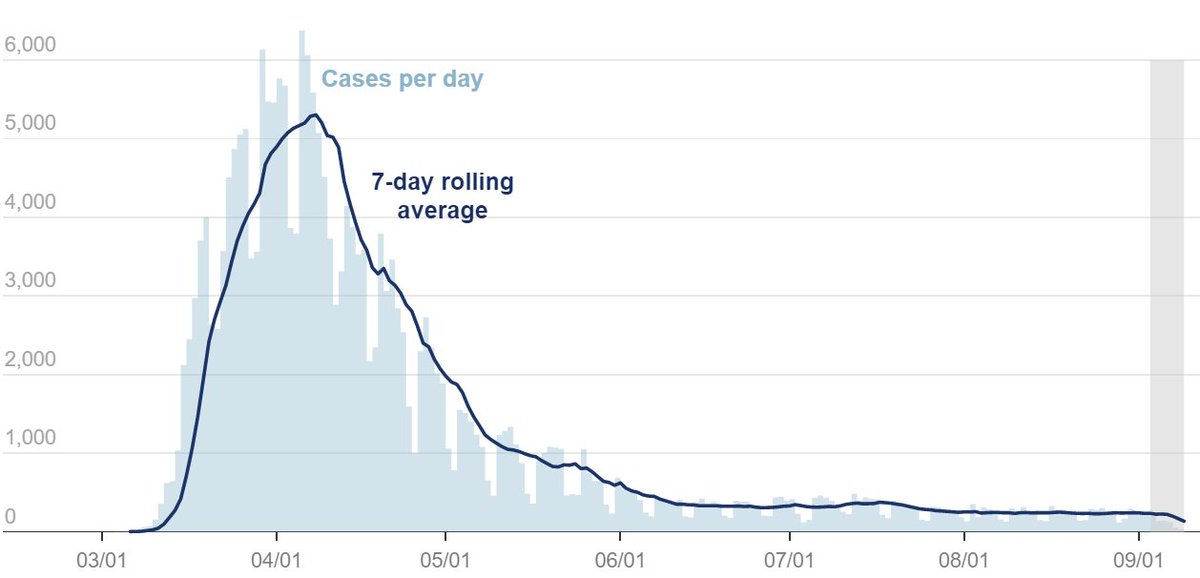
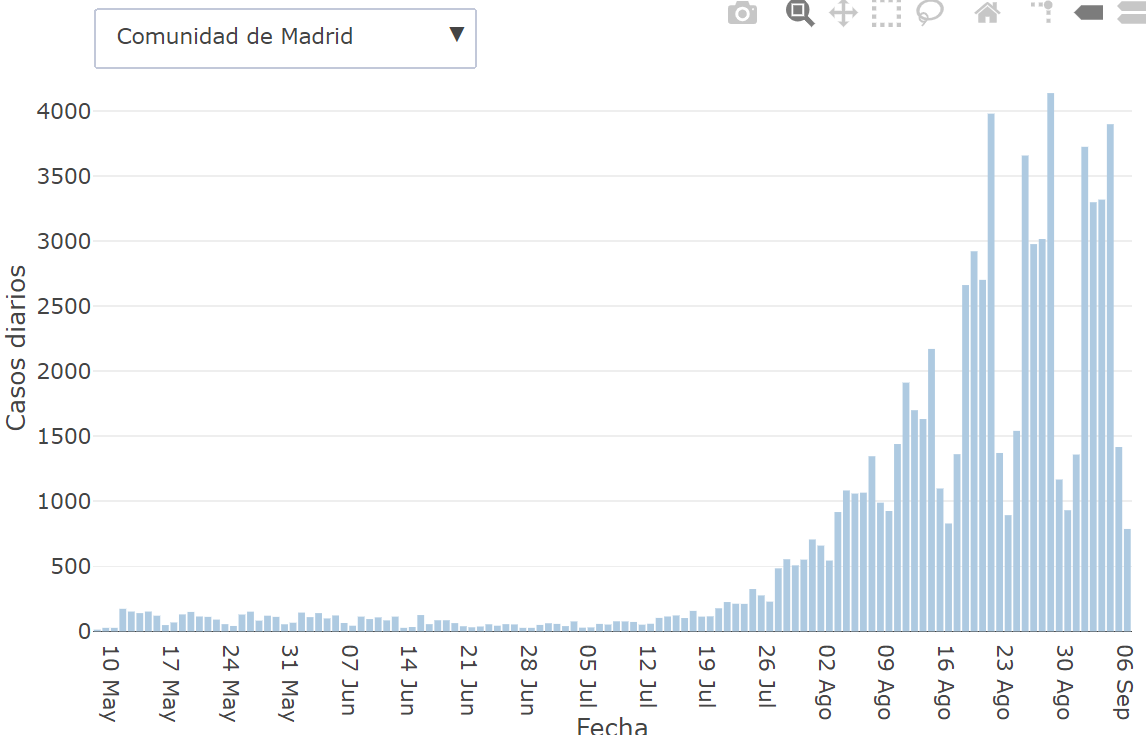
-Comparison would have been better for NYC & Madrid. Not sure why data from a whole state is being compared to a city. Maybe b/c @_MiguelHernan wants to claim seroprev is similar b/w 2 locations which is NOT true about NYC (25%) & Madrid (15%) but is for NYS & Madrid?
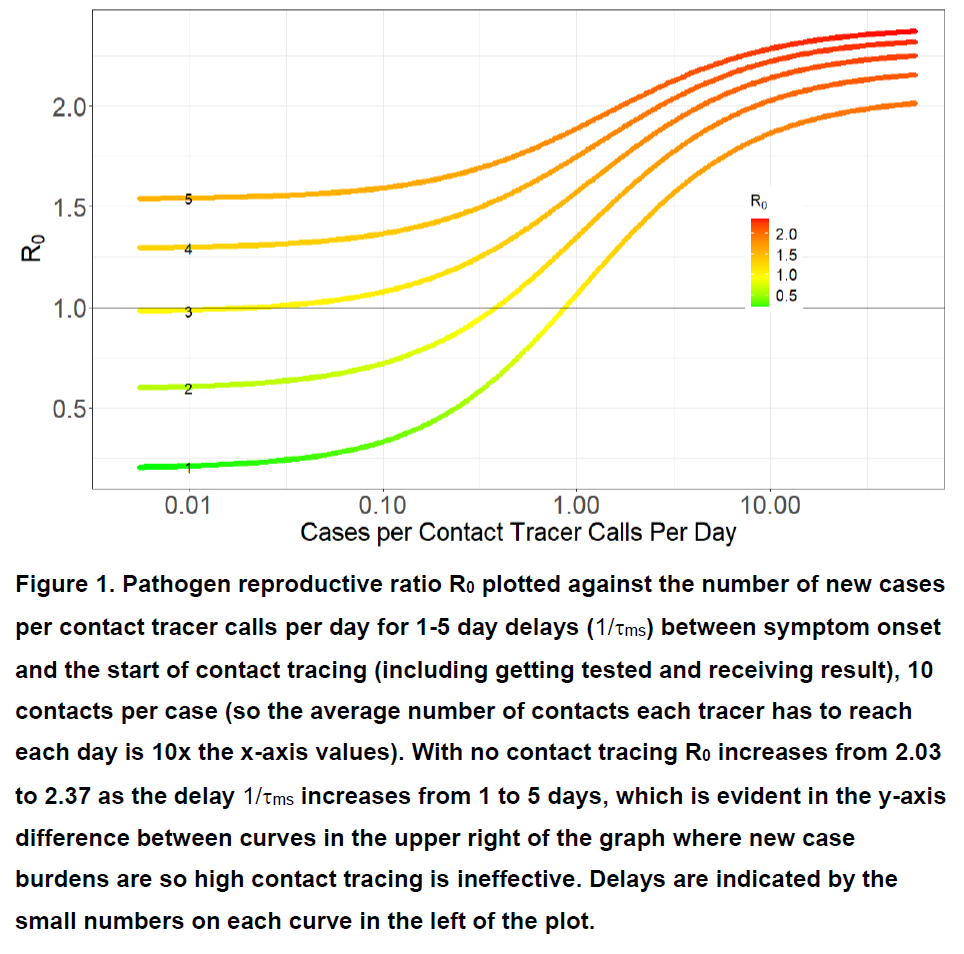
-@_MiguelHernan claims diff #s of contact tracers made a difference but our recent paper (
https://twitter.com/DiseaseEcology/status/1304486025599660032) shows this is unlikely to be true. If they had 200 tracers in early July this would be plenty to trace the <100 cases they had in July (cnecovid.isciii.es/covid19/#ccaa).
@_MiguelHernan also suggests that opening restaurants played key role. It's quite possible that open restaurants led people to have close contact/dinner w/ people from other households, but evidence for b/w table transmission is anecdotal & likely makes up tiny frac/<1% of cases.
If anyone has seen study with % of cases in a city/county/state that are traced back to b/w table transmission at restaurants please link here. Similarly, if anyone has seen data for % of cases that arise from work activities (not social), please link here. Outbreaks #s aren't %s
There is far too much hand-waving and policy being made about the importance of indoor dining or work-related transmission w/ no actual quantitative evidence on its relative importance. I am not aware of ANY study or quantitative data on this critical topic.
My own speculation on key diffs b/w NYC & Madrid are:
- Differences in behavior (possibly driven by open indoor dining @ restaurants, but not directly resulting from b/w table transmission)
(cont)
- Differences in behavior (possibly driven by open indoor dining @ restaurants, but not directly resulting from b/w table transmission)
(cont)
- Different levels of immunity (~2x in NYC vs Madrid) both below herd immunity threshold:
https://twitter.com/DiseaseEcology/status/1275595167936868352
https://twitter.com/DiseaseEcology/status/1283868410363777024
- Now that cases have risen to much higher levels, insufficient contact tracing capacity (
(Note that due to diffs in testing, case counts in Feb & Aug not really comparable),
https://twitter.com/DiseaseEcology/status/1304486025599660032).
(Note that due to diffs in testing, case counts in Feb & Aug not really comparable),
Finally, while re-opening businesses has repeatedly led to increases in cases, as it did in Spain, it doesn't have to be this way. Lockdowns are not the only way:
https://twitter.com/DiseaseEcology/status/1272271134696673281
• • •
Missing some Tweet in this thread? You can try to
force a refresh