1/ Thread -- Let's Get the Data
Many medical professionals (like my good friend and colleague, @DrNadolsky) feel strongly that #LowCarb-ers may be acting very recklessly by allowing their #LDL #Cholesterol to be much higher than the guidelines allow.
citizensciencefoundation.org/concerned-for-…
Many medical professionals (like my good friend and colleague, @DrNadolsky) feel strongly that #LowCarb-ers may be acting very recklessly by allowing their #LDL #Cholesterol to be much higher than the guidelines allow.
citizensciencefoundation.org/concerned-for-…
2/ And this may well be the case.
Certainly if "diet induced" high LDL is the equivalent to genetically high LDL, such as those with #FamilialHypercholesterolemia (FH), then there should be likewise rapidly progressing #atherosclerosis.
Certainly if "diet induced" high LDL is the equivalent to genetically high LDL, such as those with #FamilialHypercholesterolemia (FH), then there should be likewise rapidly progressing #atherosclerosis.
3/ "The sine qua non of FH is severe elevation of total and LDL cholesterol levels." jaoa.org/article.aspx?a…
Often heterozygous FH is considered where LDL is 190 to 500 mg/dL, with homozygous being above 500.
Often heterozygous FH is considered where LDL is 190 to 500 mg/dL, with homozygous being above 500.
4/ Indeed, there are key symptoms they may arise in the low carb community related to high cholesterol-- the most relevant being "tendon xanthomas"
"Tendon xanthomas are a classic pathognomonic physical examination finding, detected in approximately 20% to 40% of those with FH."
"Tendon xanthomas are a classic pathognomonic physical examination finding, detected in approximately 20% to 40% of those with FH."
5/ I won't link a picture here, but you can google "tendon xanthomas" for examples.
(Note these are different than xanthelasmas which can occur around the eyes/eyelids, but are less specific to FH -- where tendon xanthomas are very specific)
(Note these are different than xanthelasmas which can occur around the eyes/eyelids, but are less specific to FH -- where tendon xanthomas are very specific)
6/ Given children with homozygous FH can get tendon xanthomas at age 2 or 3, and given the lipid hypothesis considers "LDL burden" to be dose dependent and log linear over lifetime exposure- these symptoms should be showing up at very high rates for low carb hyper-responders soon
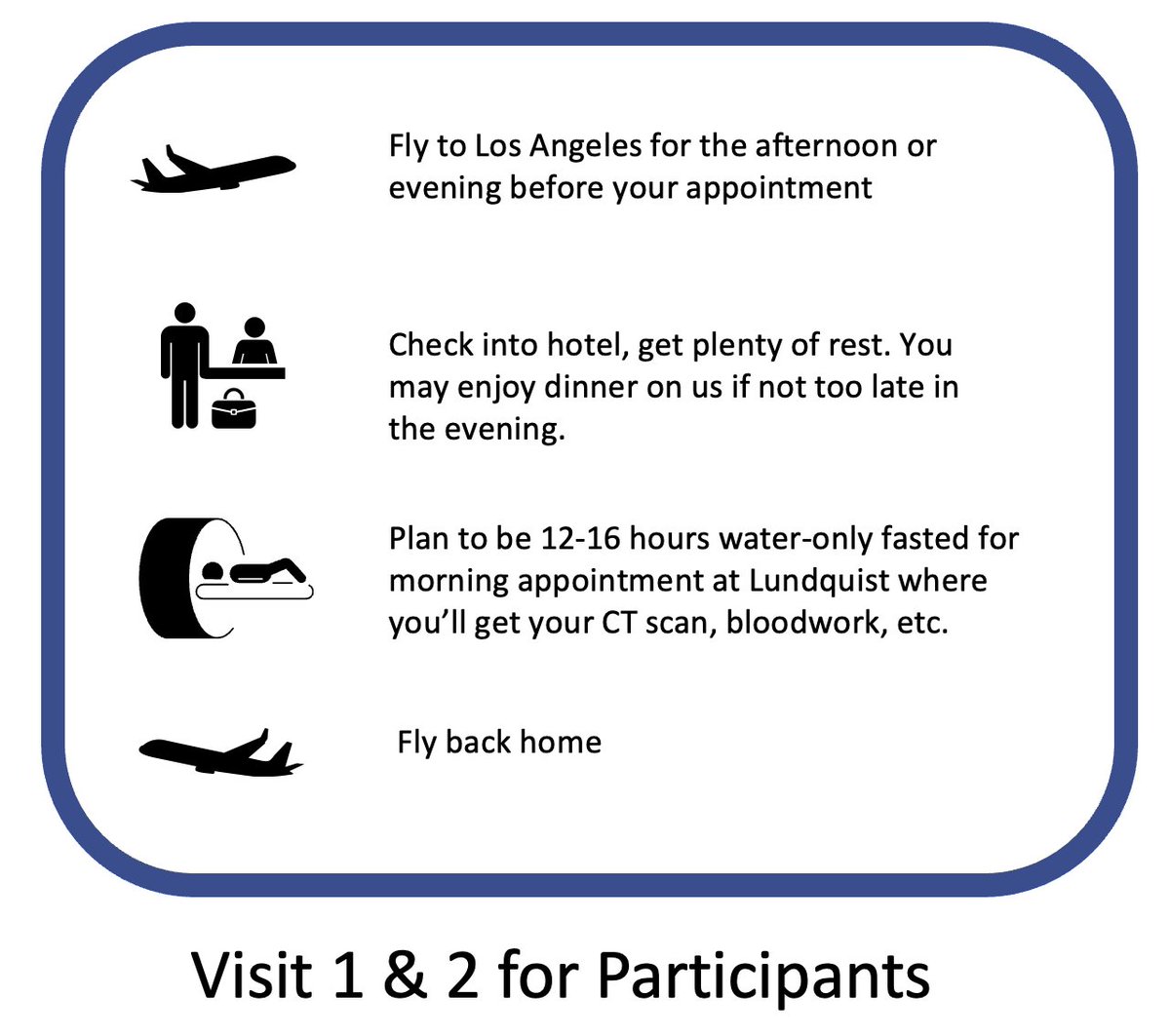
7/ Which is all the more reason to take Computed Tomography Angiography (CTA) scans in a clinical trial as soon as possible -- which is our central measurement for the study.
CTAs can display powerful, high resolution geography of the cardiovascular system.
CTAs can display powerful, high resolution geography of the cardiovascular system.
8/ And given the effect size of "Lean Mass Hyper-responders" (LMHRs) where LDL is often well above the guidelines (>190 mg/dL -- with many in the 300s, 400s, 500s or more), we should be able to observe the same rapid progression of atherosclerosis we see with FH in just 1 year.
9/ To emphasize -- if you believe low carbers are being too cavalier with their high cholesterol -- help fund this study to bring this data back to them ASAP.
This study could potentially give notice to everyone on low carb who might need to take steps to lower their lipids.
This study could potentially give notice to everyone on low carb who might need to take steps to lower their lipids.
10/ Conversely, if you yourself are low carb with high cholesterol and believe the data will show low to no risk, you should be just as motivated to get the evidence specific to this context.
In short -- help us get the data that's relevant to you.
citizensciencefoundation.org/concerned-for-…
In short -- help us get the data that's relevant to you.
citizensciencefoundation.org/concerned-for-…
11/ As of this thread, our funding sits at $86,472.00 on our way to $100,000 -- where we have an anonymous donor set to match with an additional $100,000 when we reach the goal. 🚨
Which is to say -- we're very, very close to having our goal of $200k to meet our base funding.
Which is to say -- we're very, very close to having our goal of $200k to meet our base funding.
12/ There's been more than enough debate around this topic without the clinical data to its context. If many low carbers are going to maintain higher LDL regardless of the guidelines, we should capture this data ASAP to confirm its efficacy.
citizensciencefoundation.org/campaigns/lean…
citizensciencefoundation.org/campaigns/lean…
13/ And as a last reminder,
(1) 100% of donations to the Citizen Science Foundation go to this study (save CC transaction/fees) -- no CSF admin %, etc
(2) Neither myself, @DrNadolsky, nor @DrRagnar are being paid or taking any compensation from the study.
And lastly...
(1) 100% of donations to the Citizen Science Foundation go to this study (save CC transaction/fees) -- no CSF admin %, etc
(2) Neither myself, @DrNadolsky, nor @DrRagnar are being paid or taking any compensation from the study.
And lastly...
14/
(3) the Citizen Science Foundation is a fully qualified 501(c)(3) for tax deductible donations. (Please speak to your preparer for details)
So for data's sake -- let's get this crucial question answered -- show your support today!
citizensciencefoundation.org/campaigns/lean…
(3) the Citizen Science Foundation is a fully qualified 501(c)(3) for tax deductible donations. (Please speak to your preparer for details)
So for data's sake -- let's get this crucial question answered -- show your support today!
citizensciencefoundation.org/campaigns/lean…
• • •
Missing some Tweet in this thread? You can try to
force a refresh