I am living with #LongCOVID. I am experiencing multi-dimensional and episodic disability, across all dimensions of disability. My primary symptom is fatigue & post-exertion malaise. Along with other symptoms. I want to describe the nature & extent of disability I experience. 

I have used the @WHO International Classification of Functioning Disability and Health (#ICF) to describe the nature of my disability living with #LongCOVID who.int/classification… 
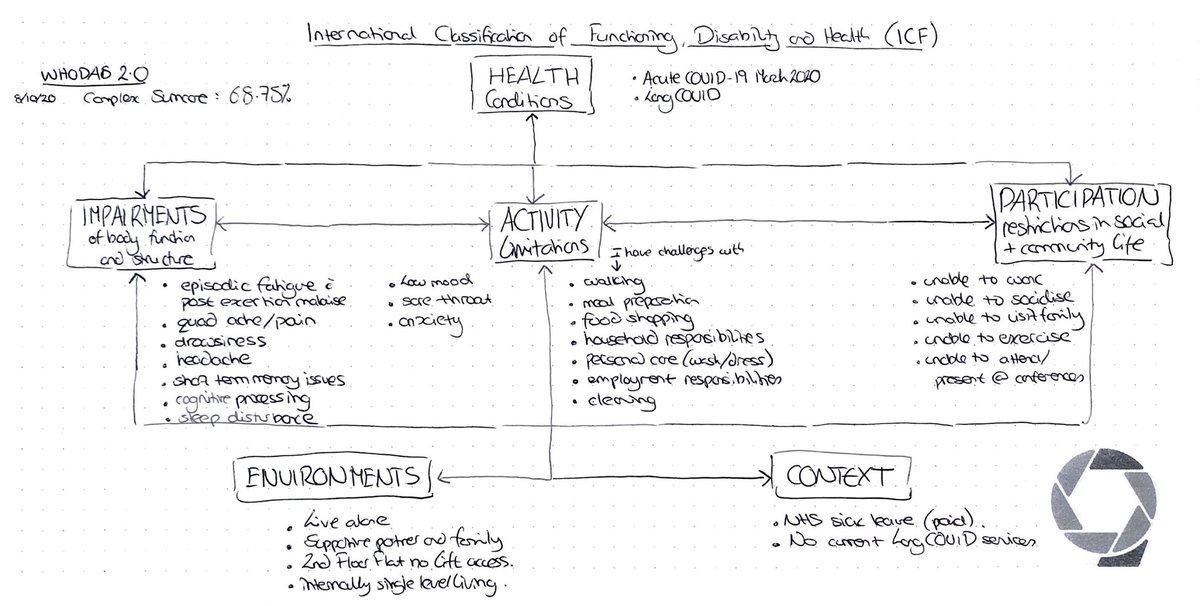
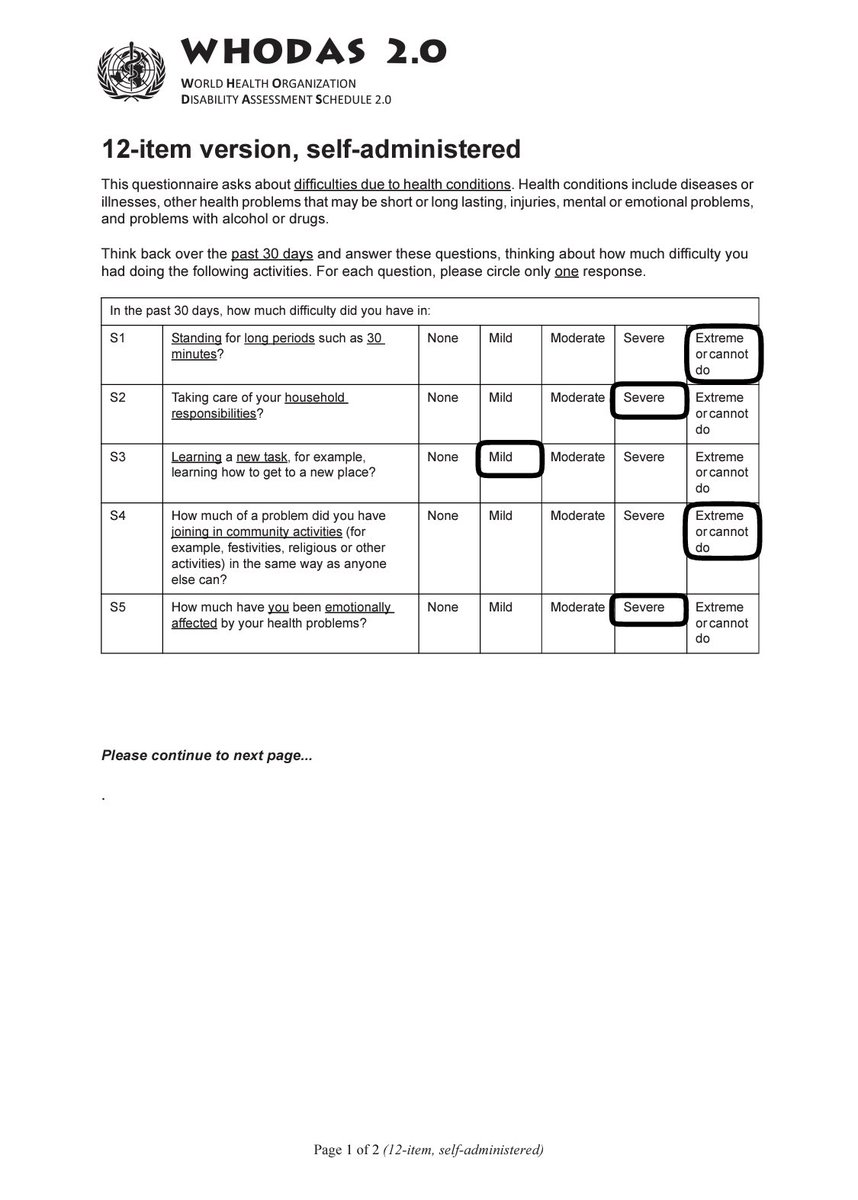
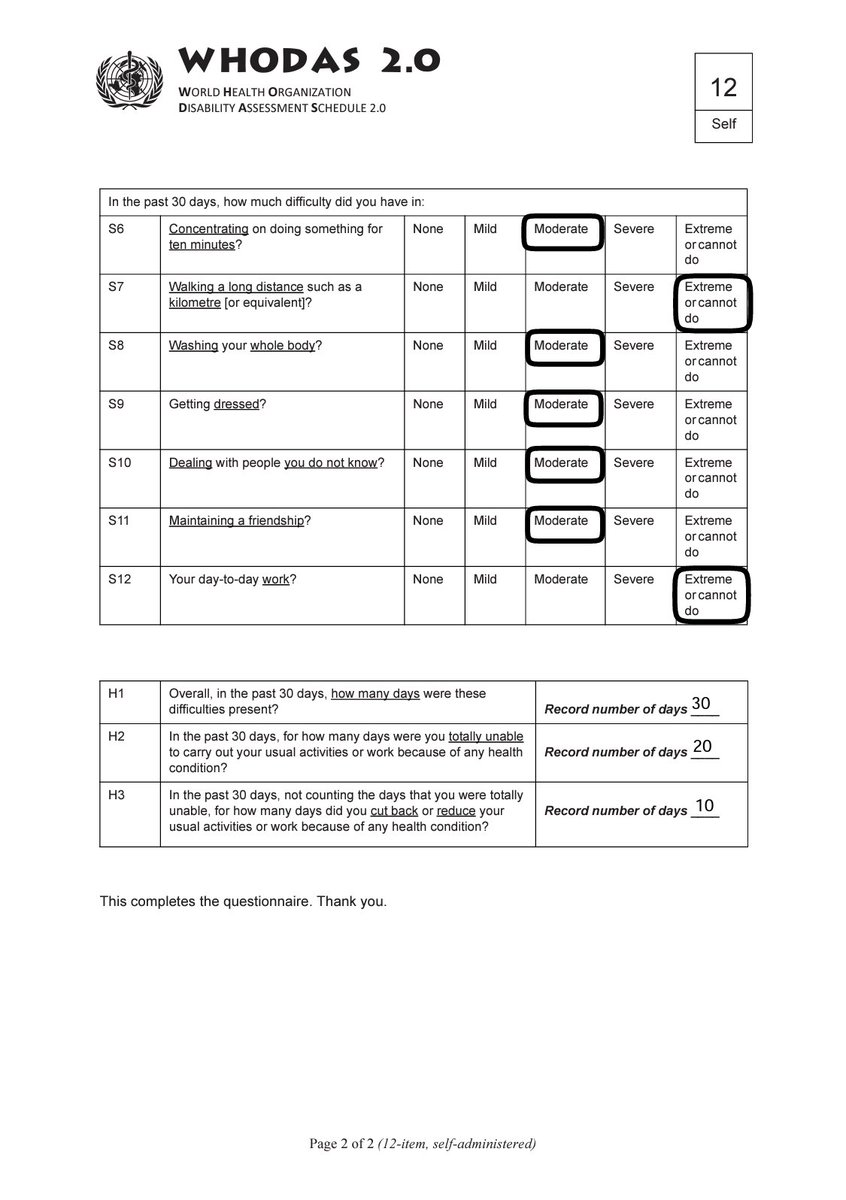
Yesterday I measured the extent of disability I experience living with #LongCOVID over the past 30 days, using @WHO World Health Organization Disability Assessment Schedule (#WHODAS). My complex sum score = 68.75% (0=no disability, 100=full disability) who.int/classification… 

I was sick with acute #COVID19 in March 2020 with fingerprick and blood tests confirming immune response in June. After 2 weeks off sick in March, I returned to work and was redeployed, including intensive care.
I returned to work for 6 months. I had ongoing symptoms including fatigue, shortness of breath and difficulty with coordination on stairs. The fatigue was unpredictable, episodic, self limiting, 24hrs in duration every 1-2 weeks. I was able to exercise at that time.
5 weeks ago I had did too much. A long walk, a cycle, and a busy day at work. I crashed. I couldn’t function. And I’ve now been signed off work for 1 month with #LongCOVID.
In the last 4 weeks I’ve been bed bound and housebound with #LongCOVID fatigue and post exertion malaise. I’ve started to improve, but much slower than I expected or hoped. I remain dependent on help for cooking & food shopping. My GP has signed me off for longer.
The post exertion malaise is brought on by physical, cognitive and emotional exertion. If I do too much, 24-48hrs later I won’t be able to do much more than go from bed to sofa for a few days. I wish I had known and had precautions of this risk with #LongCOVID
The information from @PhysiosForME has helped me so much to cope and manage more living with #LongCOVID. Particularly pacing, rest, heart rate monitoring, and symptom recording. physiosforme.com
I have also found that Heart Rate monitoring has helped reduce the physically induced post exertion malaise (PEM) #LongCOVID ... but not with cognitively induced #PEM ... I’m still learning to navigate that part physiosforme.com/heart-rate-mon…
Pacing has been the most useful technique to manage the fatigue living with #LongCOVID ... the Three Ps (Pacing, Planning, Prioritising) is useful. I’ve added my own 4th P (Precauation) because of post-exertion malaise
rcot.co.uk/conserving-ene…
rcot.co.uk/conserving-ene…
My new essential living with #LongCOVID is @FlipstickInt height adjustable folding stick with a seat (and carry bag 😊). It helps me pace. With social distancing, everywhere has a queue now eg. The shop opposite my flat & the toilet in the supermarket.
I am using @BearableApp and it’s been so useful to monitor my #LongCOVID symptoms, mood, diet, contributing factors & more bearable.app
I wanted to share this info about living with #LongCOVID, as part of my own rehabilitation. I’m proud I’ve been able to do it. I hope it’s useful. This last month, I wouldn’t have coped without my partner & family. I hope they know how grateful I am and how much I love them 🥰.
For anybody interested in the #WHODAS you can find out more on the following links:
👉 who.int/classification…
👉 sciencedirect.com/science/articl…
👉 nhivna.org/file/5f6201c20…
👉 who.int/classification…
👉 sciencedirect.com/science/articl…
👉 nhivna.org/file/5f6201c20…
• • •
Missing some Tweet in this thread? You can try to
force a refresh










