This article raises some interesting points. Have death rates from COVID-19 gone done since March?
npr.org/sections/healt…
npr.org/sections/healt…
Now, I think it's reasonable to assume that the proportion of people who die after being infected by COVID-19 will fall over time. It's probably true that being infected today is less deadly than earlier this year
That being said, I'm quite skeptical of the evidence presented. This story seems to claim that death rates have dropped ENORMOUSLY, while I would expect something more in the range of a relative 10-20% drop (say from 25% to 20%) 

The study that's linked to to verify the statement above is this one, and it's an interesting piece of research looking at some hospitals in NYC and the people they admitted for COVID-19 over time medrxiv.org/content/10.110…
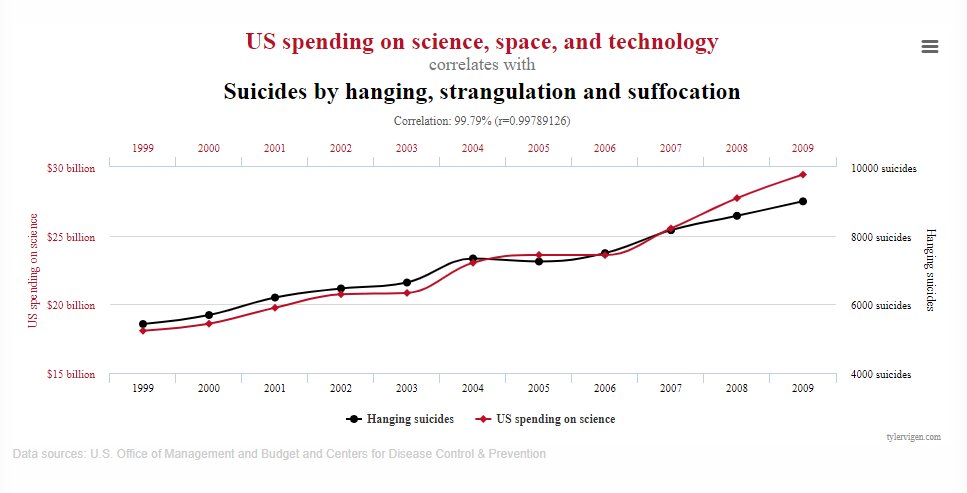
Looking at the results table, something immediately springs out. The denominator here - the number of patients being admitted by week - has changed DRAMATICALLY over time 

Perhaps more worryingly, that precipitous drop from 25% death rate to 7.6% cited in the news article appears to be based on...a single week of data. If you move back two weeks, there's no drop in death rates at all! 
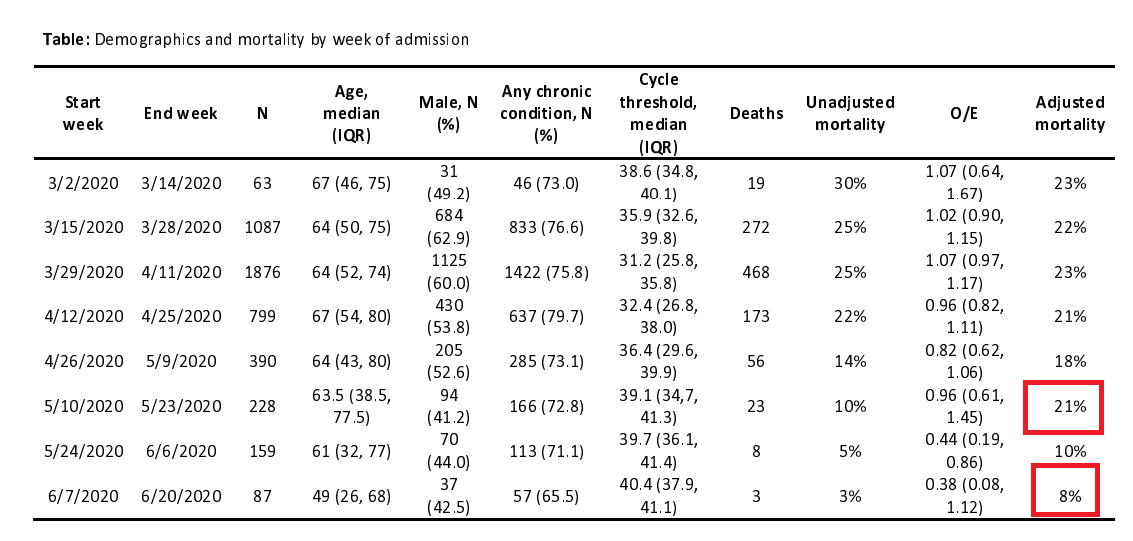
There also isn't really any trend here - a nonsignificant drop from 23% to 21% over two months, and then a sudden halving of the death rate in just one week, which corresponds to a sudden decrease in the average age
Moving on, we have the second paper cited in the NPR article, which looks at a very large sample of people who were admitted to ICU in English hospitals for COVID-19
medrxiv.org/content/10.110…
medrxiv.org/content/10.110…
This study found that if you take the average death rate of these patients from the 'peak', it decreased in a linear fashion each week, and thus COVID-19 is getting less lethal 
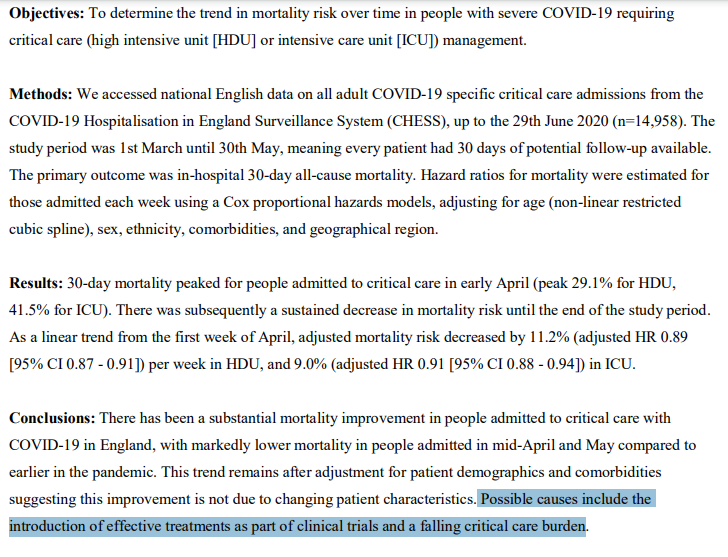
But why did they choose the 'peak' week? It wasn't the first week of data collection, and it's a bit arbitrary to only start counting from the worst week in the whole dataset
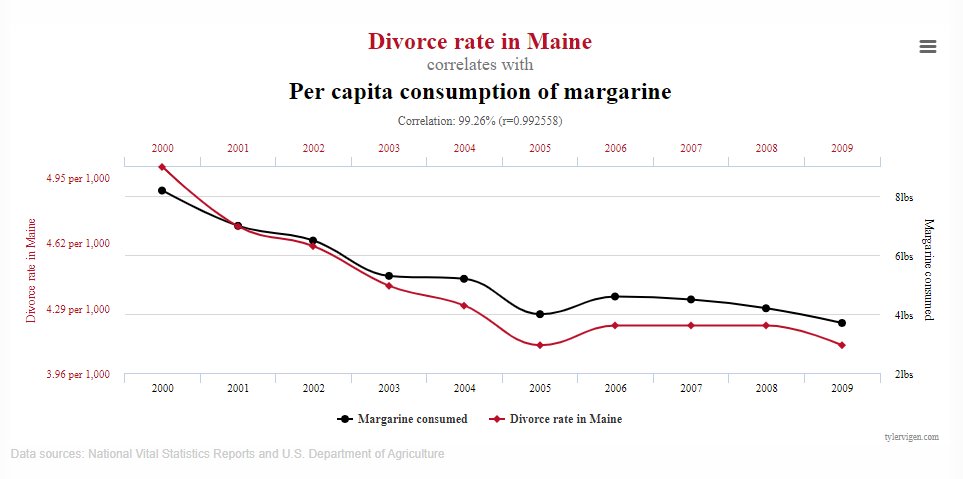
Indeed, if we extend the analysis back even just 3 weeks, the relationship disappears almost entirely and suddenly there's been very little difference since March! 
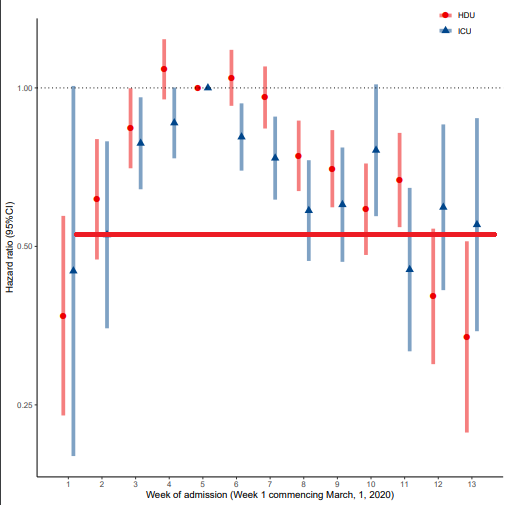
I would go so far as to say that this study implies that any differences in ICU mortality in England due to COVID-19 are ~almost certainly~ down to admission criteria (which were strained during the peak in early April)
So, back to the question at the beginning of the thread: are your chances of dying from COVID-19 lower today than they were in March?
Honestly, while we'd hope so, I'm not sure we can conclude much either way
Honestly, while we'd hope so, I'm not sure we can conclude much either way
• • •
Missing some Tweet in this thread? You can try to
force a refresh