If epidemic growing, question isn’t really ‘are more restrictions needed?’ The question is ‘given restrictions will eventually have to come in, do you want to have COVID at a high or low level over winter?’ 1/
https://twitter.com/AdamJKucharski/status/1314587565866061825?s=20
With almost daily 100k infections in England & growing (imperial.ac.uk/news/207534/co…), we'd eventually expect to see some effects of immunity. But even if restrictions introduced to keep R near 1, that infection level means can expect huge number of hospitalisations & deaths first. 2/
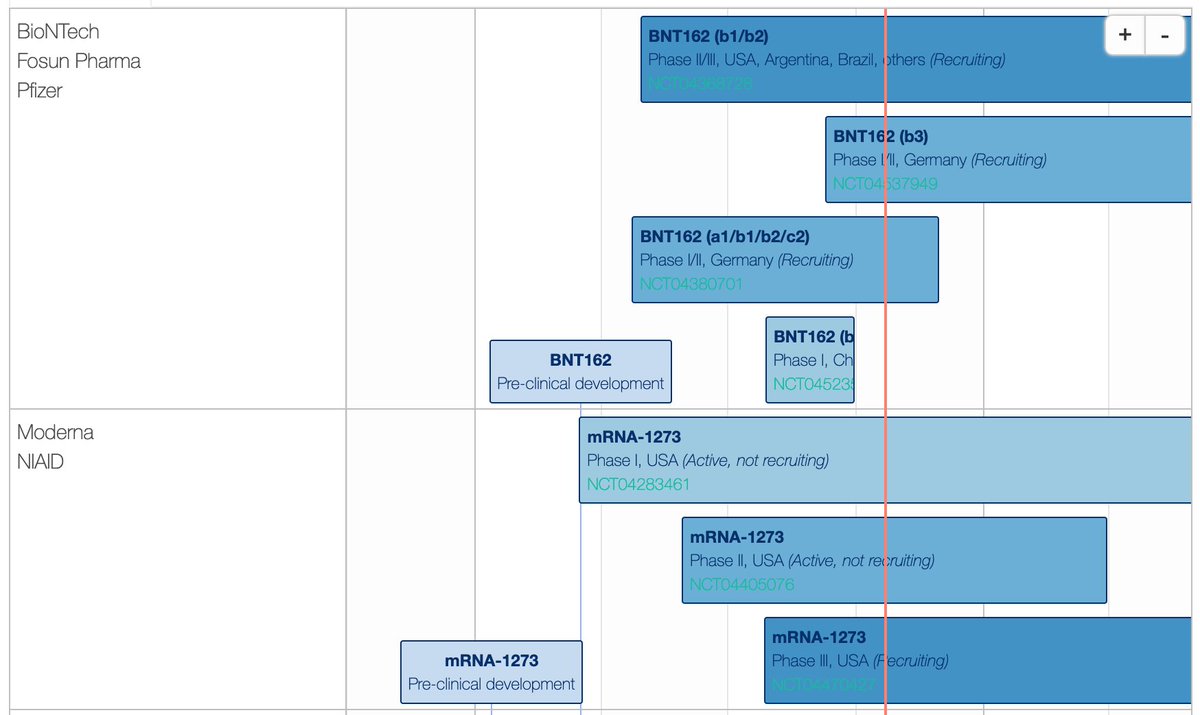
Getting to lower infection levels requires restrictions earlier, but opens up more targeted control options (more of which are becoming available, e.g. theguardian.com/world/2020/oct…), which could mean less disruption in longer term. 3/
https://twitter.com/AdamJKucharski/status/1312749956915224576?s=20
So that’s the choice. High levels of infection, hospitalisations, deaths & disruption to wider healthcare, and hope for some eventual immunity. Or lower levels of infection, more targeted measures, and hope for better treatment/vaccine options in future. 4/4
• • •
Missing some Tweet in this thread? You can try to
force a refresh