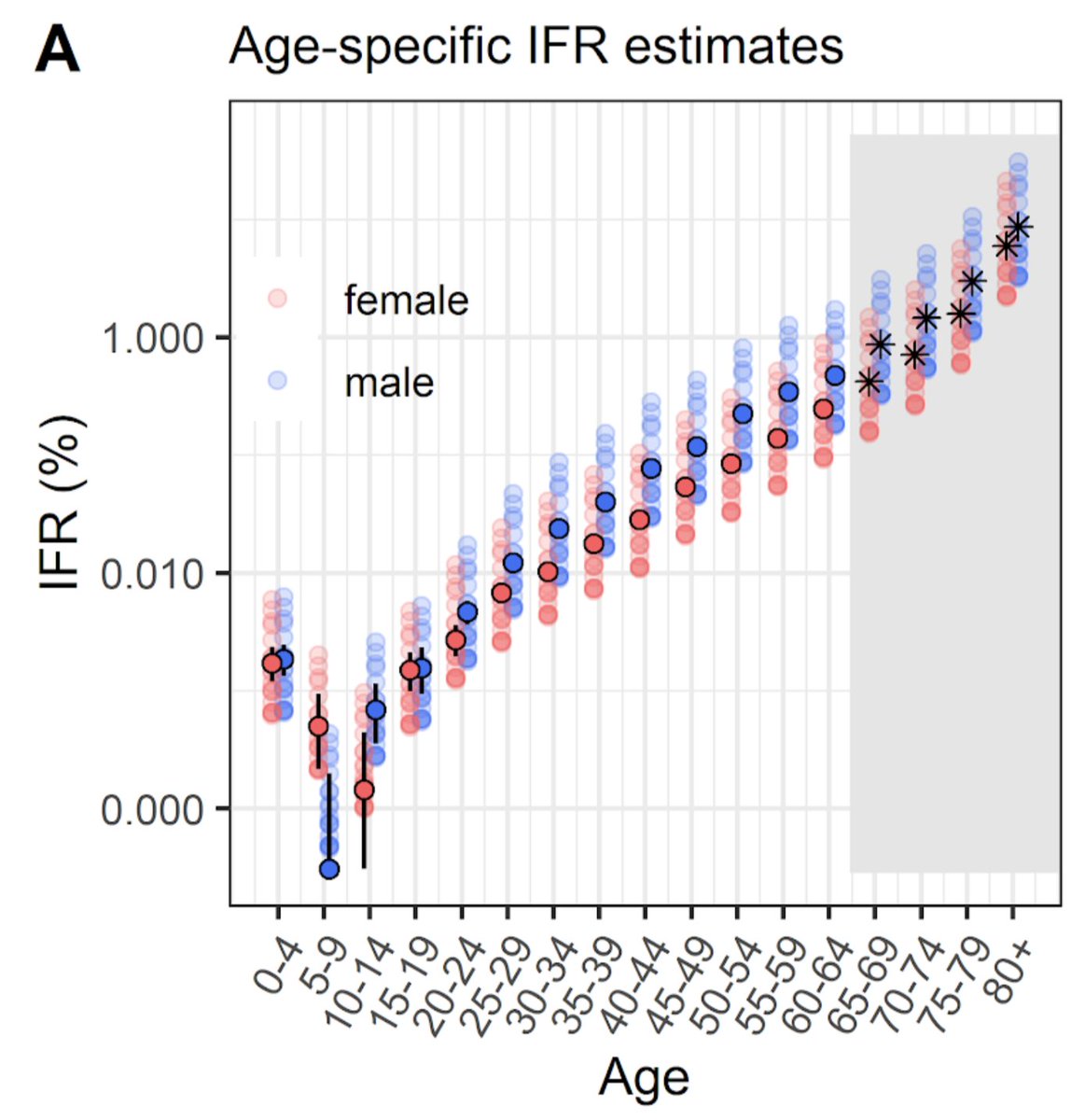
I'm increasingly seeing people quote a single 'global' estimate of infection fatality risk (IFR) for SARS-CoV-2 & use this value to try and make conclusions about specific countries. But, of course, this is missing out a crucial aspect of risk... 1/
We've known since the early days of the pandemic that fatality risk is strongly dependent on age (as well as other factors), which means that estimates will depend on population structure and age group that gets infected. 2/
For example, Singapore has reported around 58k cases and 28 deaths, which would imply that less than 0.05% of local infections resulted in death. But lot of these infections were concentrated in groups of younger migrant workers, rather than the wider - and older - population. 3/
When epidemics are larger, reaching beyond clearly defined clusters, we'd expect more cases in older groups because of the inter-generational social links within most populations:
https://twitter.com/AdamJKucharski/status/1307731922018336775?s=204/
Early estimates, which used traveller testing (thelancet.com/journals/lanin…) and patterns from Diamond Princess outbreak (eurosurveillance.org/content/10.280…) to adjust for under-reporting, put IFR at 0.6-0.7% in China. 5/
Remember, these early estimates didn't use any serological data. Subsequent studies have refined these analyses (e.g. medrxiv.org/content/10.110… & imperial.ac.uk/mrc-global-inf…), showing that a single 'global IFR' obscures crucial variability between countries. 6/6 
• • •
Missing some Tweet in this thread? You can try to
force a refresh