Interesting new preprint trying to assess surface transmission of COVID-19/SARS-CoV-2.
tl;dr RNA is everywhere but in very low amounts; surface sampling could be useful for surveillance. Risk of infection unknown b/c study didn't look at live/infectious virus.
Short thread
tl;dr RNA is everywhere but in very low amounts; surface sampling could be useful for surveillance. Risk of infection unknown b/c study didn't look at live/infectious virus.
Short thread
https://twitter.com/SeqH2O/status/1323361394301968384
Background
One of the huge early questions about transmission of SARS-CoV-2 was if the virus could be easily transmitted on surfaces. We all heard 1000s of times how much we should wash our hands, in part, to protect us against surface transmission. But...
One of the huge early questions about transmission of SARS-CoV-2 was if the virus could be easily transmitted on surfaces. We all heard 1000s of times how much we should wash our hands, in part, to protect us against surface transmission. But...
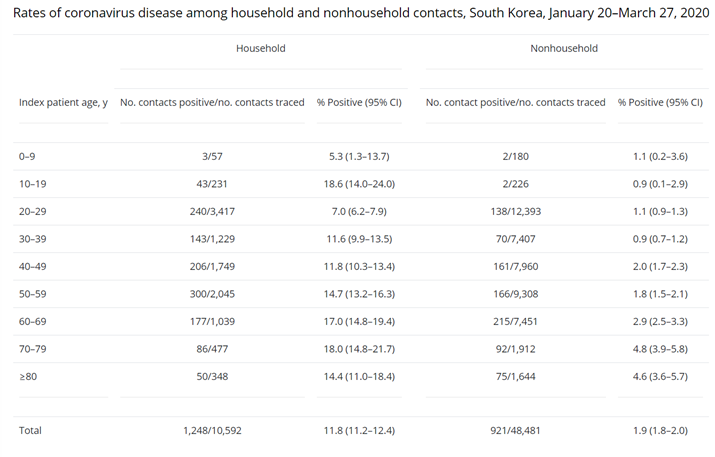
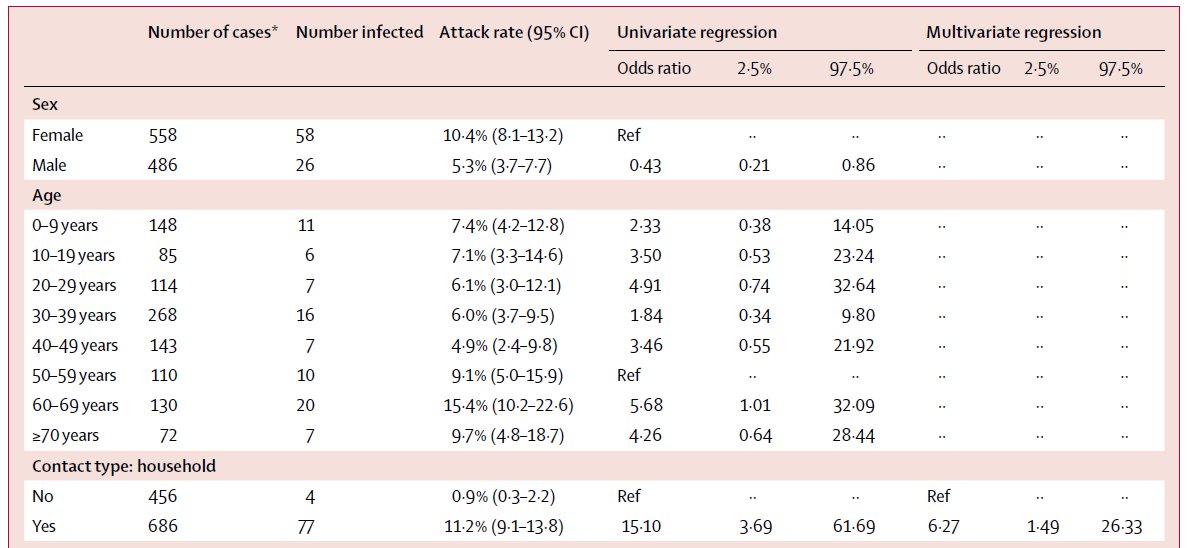
Epidemiological evidence rarely suggested surface transmission was major issue. The best evidence for the absence of its importance (which is a hard thing to study!) was that (nearly?) all early cases in some locations (e.g. Singapore) could be traced back to known close contact.
A few cases have been linked to surface transmission (trash bin in NZ: rnz.co.nz/news/national/…; possibly an elevator, a chair & at a mall:
https://twitter.com/DiseaseEcology/status/1279097818351726592), but in general it's not thought to be an important mechanism.
Even CDC, which still puts hand washing as a top priority for protecting yourself, clearly states that it's a rare transmission pathway:
https://twitter.com/DiseaseEcology/status/1313193505276133376
This new study swabbed a bunch of high-touch surfaces in MA & found SARS-CoV-2 RNA on ~8% of 348 samples. Initial reaction might be: yikes! It's everywhere! But remember, test is for RNA, not infectious virus.
medrxiv.org/content/10.110…
medrxiv.org/content/10.110…

Sadly authors don't try to culture any of their samples, so it's not clear if ANY had infectious virus. Also, there's (still) no estimate of the infectious dose for SARS-CoV-2 (@angie_rasmussen) so even if they had cultured some, they couldn't really put a risk probability on it.
But the authors DO claim to estimate a risk of infection & even state an upper bound in abstract. How can they do this? Magic! Sort of. A QMRA (quantitative microbial risk assessment). 



For QMRA authors used data from other viruses for many parameters. I think authors should remove this calculation. It provides a false sense of quantification when none is actually possible (@callin_bull might use it as an example), even within order of magnitude. 

So what can we learn from this study? It provides interesting insight into how often one can pick up viral RNA on high touch surfaces & suggests these might be ways to do surveillance, similar to sewage.
Authors claim it might even be a leading indicator of cases but I don't find this convincing. Authors have to exclude some early points to get the correlation to be significant & even then it's not especially strong to me. However, I still think it's very useful. 

One huge advantage of this sampling strategy (compared to sewage, for example) is that one can target specific locations (doorknob of building) & if building use is by a known population (e.g. a school) one could then test people when RNA is detected on surfaces.
If RNA is detected before cases (which is likely in a young pop where most cases will be mild or asymptomatic), one could possibly monitor a large population w/ a much smaller # of samples.
So, I would love to see follow-up studies by other groups (schools!) & see if surface sampling can indeed detect RNA before cases are observed. We need all the tools we can to find infected people & this could be one more useful tool in our toolbox!
• • •
Missing some Tweet in this thread? You can try to
force a refresh