As epidemic trajectories in Europe rise back towards their spring peaks, a thread on normalisation during a pandemic... 1/ 

In late Feb & early March, we modelled scenarios for what effect widespread social distancing measures might have in UK. Like others, we'd already modelled contact tracing (thelancet.com/journals/langl…) but characteristics of infection suggested additional measures would be needed. 2/
At the time we were doing this modelling, fewer than 3000 COVID deaths had been reported globally (below from 1st March). I remember doing media during this period and could tell many saw the potential impact of COVID-19 as rather abstract, given observed numbers to date... 3/ 

In our analysis during that period, we considered a range of measures, including self-isolation when ill, shielding of older groups, school closures, social distancing... Two crucial factors influenced these scenario estimates: severity & transmission dynamics. 4/ 

Early severity estimates using traveller testing (thelancet.com/journals/lanin…) and age-adjusted patterns from Diamond Princess data (eurosurveillance.org/content/10.280…) put IFR at 0.6-0.7% in China. UK has similar, albeit slightly older demography, which would mean similar IFR. 5/
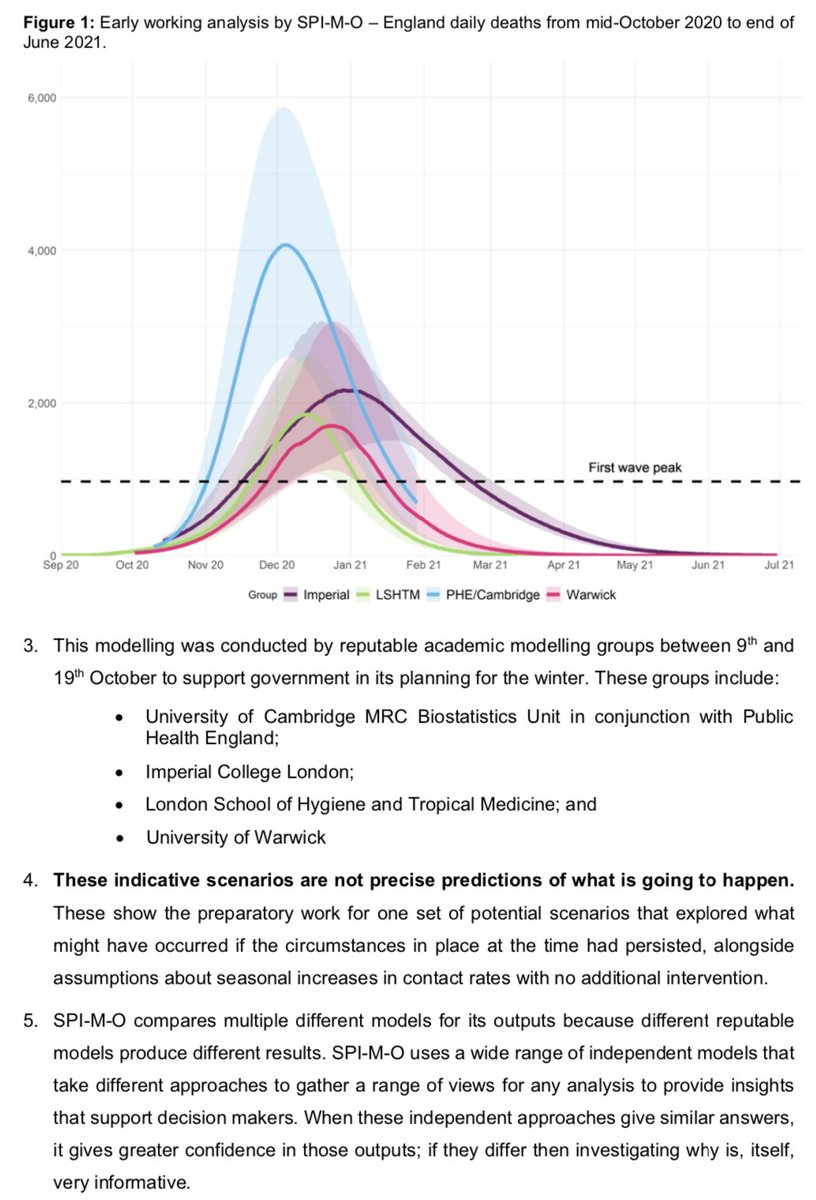
Using age structured transmission models, accounting for differences in contact structure between home/work/school etc, Imperial (imperial.ac.uk/mrc-global-inf…) and LSHTM (thelancet.com/journals/lanpu…) concluded that uncontrolled epidemic could lead to hundreds of thousands of deaths. 6/
Many commentators subsequently focused on these big numbers in the 'do nothing' scenarios, but in scenarios where lockdowns were triggered once given number in ICU, estimates were much lower - some point estimates even lower than the subsequent reality. 7/ 



Some disagreed with these assumptions, claiming IFR actually as low as ~0.01% (e.g. unherd.com/2020/05/oxford…), which implied couldn't have many deaths. Arguments have since shifted – while virus has continued spreading, indifferent to claims otherwise:
https://twitter.com/AdamJKucharski/status/1308350331231797248?s=208/
But here we are again, with deaths across Europe rising - numbers that were once thought astonishing, and are now seen by many as normal. So I think it's important to occasionally reflect on this transition, and how once big numbers came to feel so small. 9/9
• • •
Missing some Tweet in this thread? You can try to
force a refresh