1/ It's indescribable seeing results from NYC EMS ambulance runs showing how cardiac arrests skyrocketed during COVID
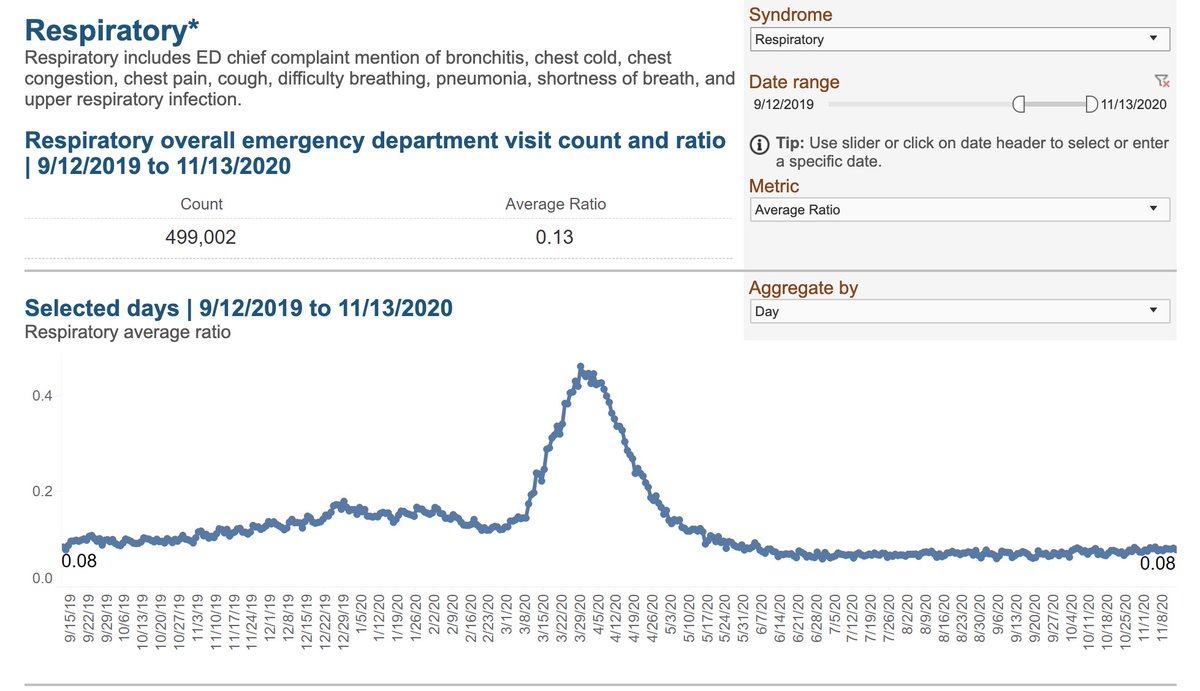
(I started a program to monitor these symptoms in real time--among the very first application of syndromic surveillance in public health, 2 decades ago)
(I started a program to monitor these symptoms in real time--among the very first application of syndromic surveillance in public health, 2 decades ago)
https://twitter.com/Farzad_MD/status/1246443356303110144

2/ Every day, crews from @FDNY are called to 20 to 30 patients who have collapsed, and attempt resuscitation. Can you imagine?
It's never like the movies. Most patients die, ribs cracked. 75% of the time you never get a heart rate back.
On April 6, there were 305.
305.
It's never like the movies. Most patients die, ribs cracked. 75% of the time you never get a heart rate back.
On April 6, there were 305.
305.
3/ In the dry language of medical research the researchers describe the horrible statistics.
During the peak, most patients had nonshockable presenting rhythms of asystole and pulseless electrical activity. 92.2% of the time they called off the resuscitation without a pulse.
During the peak, most patients had nonshockable presenting rhythms of asystole and pulseless electrical activity. 92.2% of the time they called off the resuscitation without a pulse.
4/ The patients were those who you would expect to suffer complications from COVID.
Older patients (mean age 72)
High blood pressure and diabetes are common
But only 23% had a history of heart disease
And controlling for all that, twice as likely to be black or hispanic
Older patients (mean age 72)
High blood pressure and diabetes are common
But only 23% had a history of heart disease
And controlling for all that, twice as likely to be black or hispanic

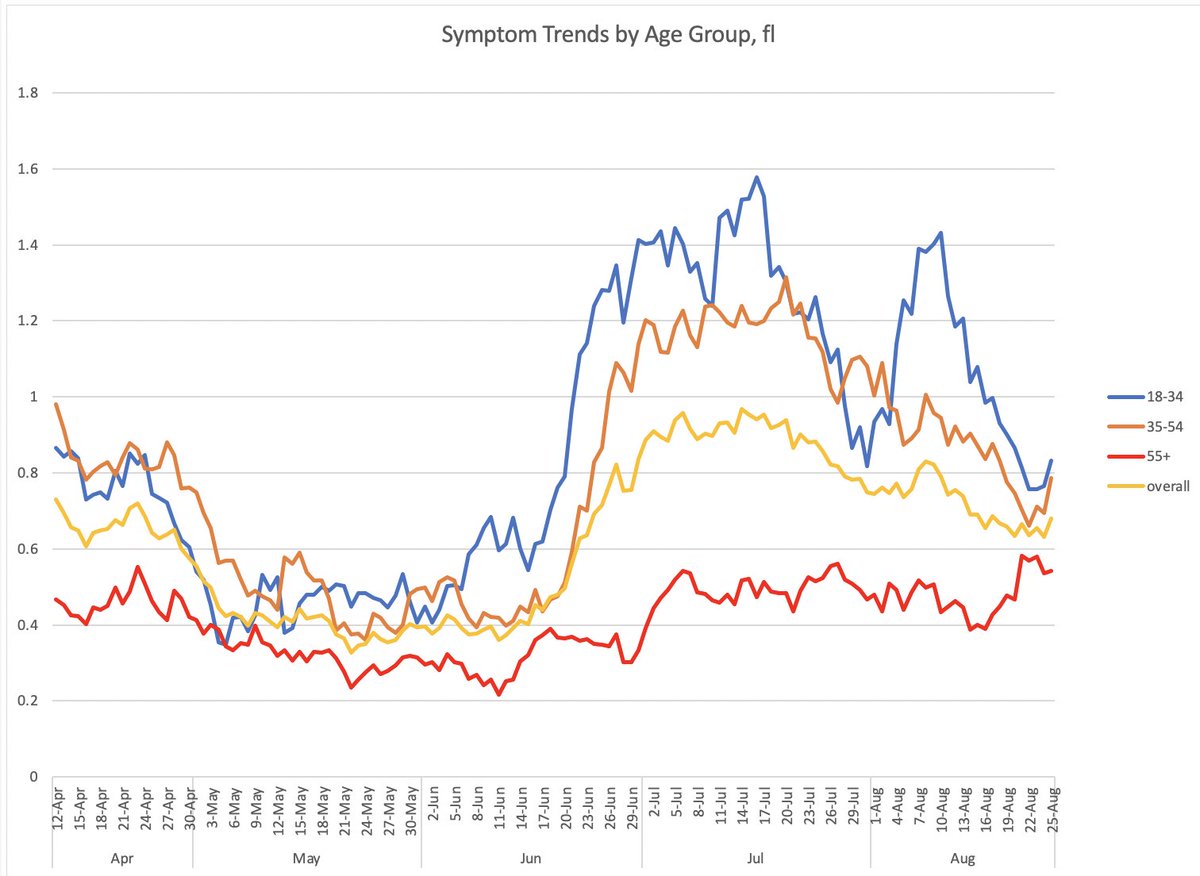
5/ This is from COVID.
The authors discuss whether it could be from people delaying medical care, but that is an epidemic curve.
You might expect delayed care to have continued to take a toll after the outbreak peak at the end of March, but it fell just as rapidly as COVID did
The authors discuss whether it could be from people delaying medical care, but that is an epidemic curve.
You might expect delayed care to have continued to take a toll after the outbreak peak at the end of March, but it fell just as rapidly as COVID did
6/ These deaths are part of why we UNDERcount deaths from COVID, as @WeinbergerDan has shown in his excess mortality analysis
jamanetwork.com/journals/jamai…
jamanetwork.com/journals/jamai…
7/ What is it going to take for us to take COVID seriously again?
Do we need to see ambulance crews overwhelmed with cardiac arrests in every city?
Do we need to see ambulance crews overwhelmed with cardiac arrests in every city?
• • •
Missing some Tweet in this thread? You can try to
force a refresh