1/ Opening schools in the midst of a COVID surge is a hard problem with unavoidable tradeoffs.
There are absolutist statements on either side of the debate, so I expect passionate rebuttals, but let me lay out a decision-making framework, from an epidemiologists' perspective
There are absolutist statements on either side of the debate, so I expect passionate rebuttals, but let me lay out a decision-making framework, from an epidemiologists' perspective
https://twitter.com/axios/status/1333099688355106822
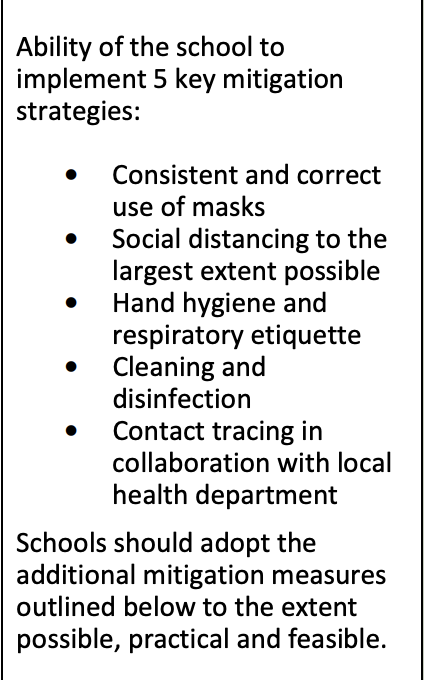
2/ First off, we have to make sure that the schools have the resources and space to implement the 5 key mitigation
strategies correctly and consistently.
Not a given.
*Masks
*Social distancing
*Contact tracing
*Hand hygiene
*Cleaning and disinfection
first 2 >> last 2
strategies correctly and consistently.
Not a given.
*Masks
*Social distancing
*Contact tracing
*Hand hygiene
*Cleaning and disinfection
first 2 >> last 2
3/ Let's say we have some resources for testing, how does that contribute?
What we are trying to achieve?
Do you think the goal is Screening (identify asymptomatic infectious cases before they can expose others) or Surveillance (understand incidence to inform policy)?
What we are trying to achieve?
Do you think the goal is Screening (identify asymptomatic infectious cases before they can expose others) or Surveillance (understand incidence to inform policy)?
4/ Either one is feasible, but we have to be really clear about what we are trying to accomplish.
If you really think you are using testing to ensure that asymptomatic cases are screened out before they can expose others, it needs to be FREQUENT (2x a week) and FAST (<24h TAT)
If you really think you are using testing to ensure that asymptomatic cases are screened out before they can expose others, it needs to be FREQUENT (2x a week) and FAST (<24h TAT)
5/ This can work.
@testing4america is supporting the safe reopening of historically Black colleges and universities like @DelStateUniv
But is has to be fast, frequent, and "for real" - ie mandatory if you want to go in-person.
whyy.org/articles/delaw…
@testing4america is supporting the safe reopening of historically Black colleges and universities like @DelStateUniv
But is has to be fast, frequent, and "for real" - ie mandatory if you want to go in-person.
whyy.org/articles/delaw…
6/ I won't get into Antigen vs PCR issue here, but right now my perspective (and that of @testing4america) is to focus on PCR tests, and to reduce the cost through pooling, w testing all samples in positive pools ("Dorfman pooling")
pool size calculator bilder.shinyapps.io/PooledTesting/
pool size calculator bilder.shinyapps.io/PooledTesting/
7/ But that's still VERY EXPENSIVE
If you have 1,200 faculty/students, pool size 12, will probably cost you ~$20 per student for pooled PCR at 1% positivity rate
That's minimum $50,000 a week-a cool $Million for the next 20 weeks Can't we test once a week? What if we stagger?
If you have 1,200 faculty/students, pool size 12, will probably cost you ~$20 per student for pooled PCR at 1% positivity rate
That's minimum $50,000 a week-a cool $Million for the next 20 weeks Can't we test once a week? What if we stagger?
8/ In general, testing once a week means that most of the infections will occur before the infection is caught and isolated
theoretically, would work if you could figure out the logistics for splitting school into 2 cohort (aiding social distancing) 1/2 in person, 1/2 virtual ..
theoretically, would work if you could figure out the logistics for splitting school into 2 cohort (aiding social distancing) 1/2 in person, 1/2 virtual ..
9/ Each cohort gets tested Wed morning, goes to school for 4 consecutive school days (Thu/Fri/Mon/Tues) every 2 weeks, then 9 days of remote learning
Assuming greatest risk is during school days, then nearly all infections should have time to become detectable by following Wed
Assuming greatest risk is during school days, then nearly all infections should have time to become detectable by following Wed

10/ Those logistics are *hard*
-Got to get the kids into testing sites on non school day (buses?)
-Turn around time has to be <15 hours
-Mandatory testing may raise issues of health equity
-Teachers will have both in-person and remote students.
Is there another way?
-Got to get the kids into testing sites on non school day (buses?)
-Turn around time has to be <15 hours
-Mandatory testing may raise issues of health equity
-Teachers will have both in-person and remote students.
Is there another way?
11/ Let's look at surveillance testing
Goal is to detect a rise in cases and move away from in-person if a substantial increase in excess cases emerges
Operationally easier, less expensive, doesn’t require 100% participation–but isn't powered to prevent chains of transmission
Goal is to detect a rise in cases and move away from in-person if a substantial increase in excess cases emerges
Operationally easier, less expensive, doesn’t require 100% participation–but isn't powered to prevent chains of transmission
12/ Surveillance testing will not significantly *create* a safe environment in the presence of community spread outside of the school.
It does require having a principled framework for deciding when school would be shifted back to remote learning based on test results
It does require having a principled framework for deciding when school would be shifted back to remote learning based on test results
13/ While it is impossible to keep schools completely safe from COVID-19, our primary aim should be to ensure that in-person school does not cause a substantial increase in excess cases (and subsequent morbidity and mortality) in the larger school community- including families
14/ How many cases before schools shut down?
Many cases identified among faculty and students will reflect community infection, unrelated to school
Can we define “substantial increase”
Can we define “excess” cases (over community baseline)?
Can we operationalize thresholds?
Many cases identified among faculty and students will reflect community infection, unrelated to school
Can we define “substantial increase”
Can we define “excess” cases (over community baseline)?
Can we operationalize thresholds?
15/ Here's a framework:
“Less than 5% chance that cases spread at school will result in a death in the school community”
Assuming IFR 0.5%/50% household transmission rate to adults
That's ~10 extra cases among school staff, or 20 extra cases among students (pop 1,000)
Is that
“Less than 5% chance that cases spread at school will result in a death in the school community”
Assuming IFR 0.5%/50% household transmission rate to adults
That's ~10 extra cases among school staff, or 20 extra cases among students (pop 1,000)
Is that
16/ Epidemiology gives us no special legitimacy in making value decisions about 1,000 kids in school vs _n_ lives saved.
You can place your own values, and this framework will relate that to thresholds for deciding when the risk is too high
But lets be honest about tradeoffs
You can place your own values, and this framework will relate that to thresholds for deciding when the risk is too high
But lets be honest about tradeoffs
17/ Can we define "excess cases"?
Here's an approach.
Get a pre-opening baseline by testing students/faculty, and compare it to the community infection estimate
@youyanggu has made a great tool to make that lookup easy
eg my county is at 1.2% right now
covid19-projections.com/infections/cou…
Here's an approach.
Get a pre-opening baseline by testing students/faculty, and compare it to the community infection estimate
@youyanggu has made a great tool to make that lookup easy
eg my county is at 1.2% right now
covid19-projections.com/infections/cou…
18/ That's your school community's baseline rate of infection before school reopening. You can then use community rate to adjust your school's "baseline" as time goes on
eg. 1.2% community infection rate
0.6% school basline (6 cases per 1,000)
At 2% community - expect 10 cases
eg. 1.2% community infection rate
0.6% school basline (6 cases per 1,000)
At 2% community - expect 10 cases
19/ This is a key point-
Just cause you have 14 cases in a week in the school testing doesn't mean that there were 14 cases "caused by" in-person school.
If community baseline correlates w 10 cases a week in school population, that's an excess of ~4 cases.
Make sense?
Just cause you have 14 cases in a week in the school testing doesn't mean that there were 14 cases "caused by" in-person school.
If community baseline correlates w 10 cases a week in school population, that's an excess of ~4 cases.
Make sense?
20/ I know, small numbers, lots of error in estimates, etc
but there's a whole body of science for "control charts" used to shut down processes (think assembly line) when cumulative deviations from expected rates exceed thresholds
Google sheet version?
cdc.gov/mmwr/preview/m…
but there's a whole body of science for "control charts" used to shut down processes (think assembly line) when cumulative deviations from expected rates exceed thresholds
Google sheet version?
cdc.gov/mmwr/preview/m…
21/ In summary, to open schools:
*decide how many excess cases you're willing to tolerate over next 20 weeks (400~1 death)
*begin weekly pooled PCR testing
*monitor excess cases c/w expected baseline
*If trends statistically exceed your tolerance, close down or intensify testing
*decide how many excess cases you're willing to tolerate over next 20 weeks (400~1 death)
*begin weekly pooled PCR testing
*monitor excess cases c/w expected baseline
*If trends statistically exceed your tolerance, close down or intensify testing

22/ Would love to hear your responses.
Huge thanks to @bijans for thinking through w me
Other references:
1) @CDCgov indications cdc.gov/coronavirus/20…
2) excellent @DukeMargolis @cmyeaton @RockefellerFdn piece rockefellerfoundation.org/wp-content/upl…
Huge thanks to @bijans for thinking through w me
Other references:
1) @CDCgov indications cdc.gov/coronavirus/20…
2) excellent @DukeMargolis @cmyeaton @RockefellerFdn piece rockefellerfoundation.org/wp-content/upl…
• • •
Missing some Tweet in this thread? You can try to
force a refresh