#tweetorial To obtain blood cultures or not to culture? This was inspired by the ? from @reverendofdoubt and @GermHunterMD reply.
A pt w/ a hip fracture on POD1 has fever of 100.8. HR 90, BP 110/75, SpO2 96% ambient air. No localizing symptoms. Do you obtain blood cultures?
A pt w/ a hip fracture on POD1 has fever of 100.8. HR 90, BP 110/75, SpO2 96% ambient air. No localizing symptoms. Do you obtain blood cultures?
2/My reflex when I hear fever is to order blood cultures. It’s not wrong to make sure, right? As a resident, I remember grumbling at the ED for not ordering cultures on that CAP patient. First, what are the harms of ordering unnecessary blood cultures?
3/ Aside from the cost, there is a high rate of contamination on blood cultures from 0.6% to over 6%. In conditions with a low pretest probability of bacteremia, this represents a large prob that a + culture is contamination. ncbi.nlm.nih.gov/pmc/articles/P…
4/ 1 study found that 1/2 of the pts w/ contaminated blood cultures received antimicrobials. While this study is older, but I have seen clinically that pts with + cultures often get started on vancomycin while PCR testing/further cultures pending.
pubmed.ncbi.nlm.nih.gov/9650937/
pubmed.ncbi.nlm.nih.gov/9650937/
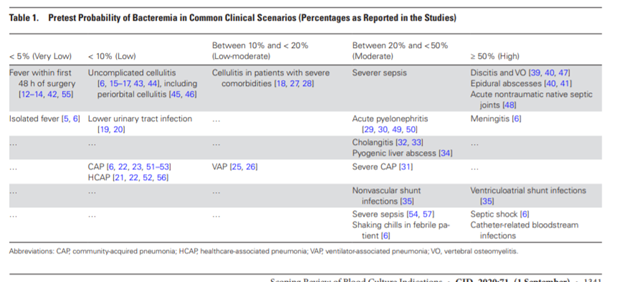
5/ So, who which conditions have low risk of bacteremia?
Very low (<5% yield)- Fever in the first 48 hours after surgery, generalized fever
Low (<10%)- cellulitis, cystitis/prostatitis , nonsevere CAP/HCAP
Low to moderate- (10-20%) VAP, cellulitis w/ comorbidities
Very low (<5% yield)- Fever in the first 48 hours after surgery, generalized fever
Low (<10%)- cellulitis, cystitis/prostatitis , nonsevere CAP/HCAP
Low to moderate- (10-20%) VAP, cellulitis w/ comorbidities
6/Moderate (20 <50%) acute pyelonephritis, severe CAP, cholangitis, pyogenic liver abscess, VP shunt
High (>50%) septic shock, meningitis, endovascular infections, discitis, vertebral osteomyelitis, epidural abscess, nontraumatic native septic joints
pubmed.ncbi.nlm.nih.gov/31942949/
High (>50%) septic shock, meningitis, endovascular infections, discitis, vertebral osteomyelitis, epidural abscess, nontraumatic native septic joints
pubmed.ncbi.nlm.nih.gov/31942949/
7/ In surgery patients, most bacteremia occurs after post-operative day 4. Fever common after surgery and usually not related to bacteremia. It is common to get cytokine release after surgery.
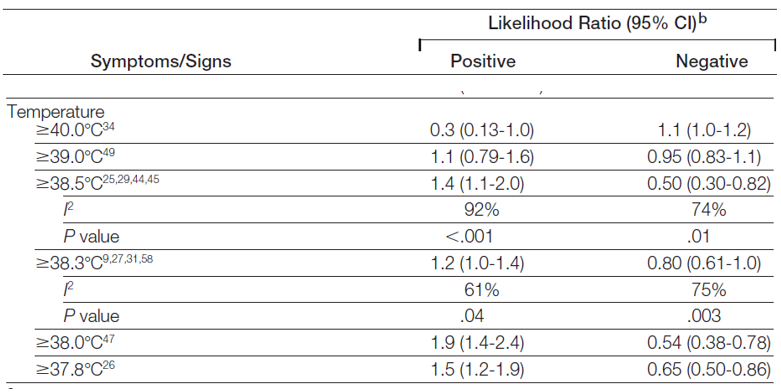
8/ What other factors ⬆️ bacteremia risk? Chills in febrile pts has a + LR 2.2. Chills defined as extremely cold w/ generalized bodily shaking even under a thick blanket + LR 4.7. The LR of + cultures does not increase linearly w/ the degree of fever. pubmed.ncbi.nlm.nih.gov/22851117/ 
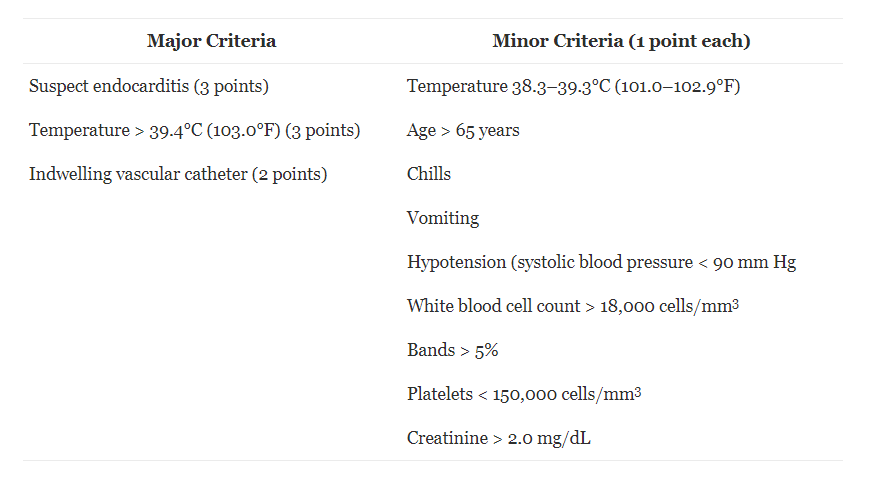
9/ The Shapiro rule was developed for ED patients and has a sens 97% with - LR of .08. pubmed.ncbi.nlm.nih.gov/18486413/ 
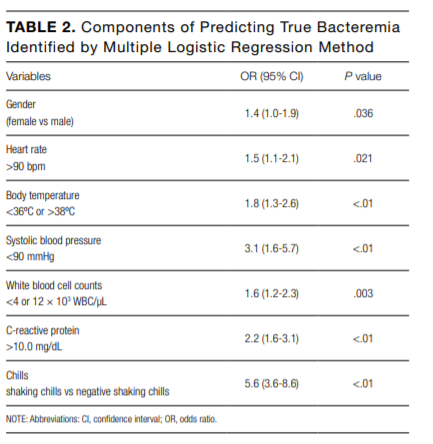
10/ Another article used the combination of shaking chills and poor food consumption (<80%) which increased pre-test prob of bacteremia to 47.7% in hospitalized pts. Patients with GI pathology were excluded. Other sig risk factors below:
pubmed.ncbi.nlm.nih.gov/28699938/
pubmed.ncbi.nlm.nih.gov/28699938/
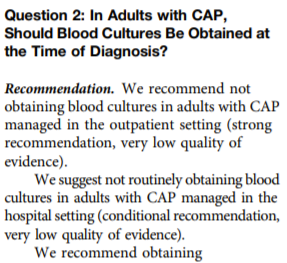
The 2019 IDSA guidelines suggest against blood cultures in uncomplicated CAP (atsjournals.org/doi/pdf/10.116…). Most studies show that even those with CAP, cultures do not change mng significantly (pubmed.ncbi.nlm.nih.gov/12684305/) 
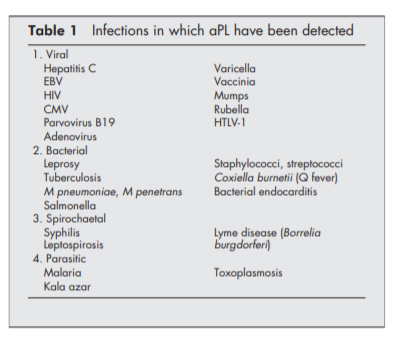
12/ It is important to recognize that in most studies participants are in immunocompetent hosts and the threshold for culturing is is lower in immunocompromised hosts. The JAMA review also emphasizes that cultures should be obtained if endocarditis suspected.
Conclusion:
☄️In conditions such as uncomplicated CAP, cystiyis, cellulitis, Post op fever <2 days post op cultures are low yield ⬆️ risk of false + contamination and generally should not be obtained.
☄️Shaking chills/rigors (w/ or w/o anorexia) ⬆️ risk of bacteremia.
☄️In conditions such as uncomplicated CAP, cystiyis, cellulitis, Post op fever <2 days post op cultures are low yield ⬆️ risk of false + contamination and generally should not be obtained.
☄️Shaking chills/rigors (w/ or w/o anorexia) ⬆️ risk of bacteremia.
☄️High risk conditions (such as meningitis, endovascular infection, or epidural abscess, septic shock) cultures should be obtained.
☄️Blood cultures can be considered in inter risk conditions if at risk of endovascular infection, unable to culture 1 site, or would change mng.
☄️Blood cultures can be considered in inter risk conditions if at risk of endovascular infection, unable to culture 1 site, or would change mng.
Also, this podcast gives a great summary:
coreimpodcast.com/2019/10/02/blo…
coreimpodcast.com/2019/10/02/blo…
• • •
Missing some Tweet in this thread? You can try to
force a refresh