#Ogitorial No35: hypothetical 41F #COVID19 intubated after failing NIV trial (24h).
A ETT 25cm
B SpO2 82% FiO2 1 Vt350 P12
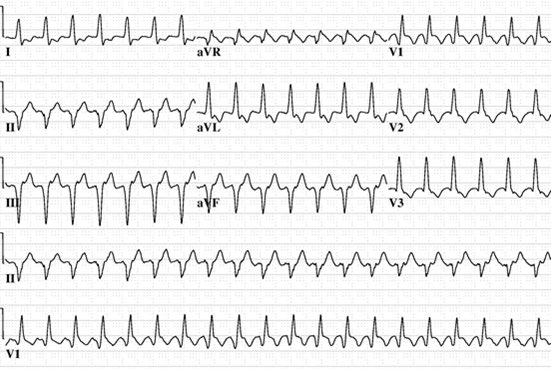
❤️BP 110/80 HR 95, CapRef 1.5”
D avpU (propofol)
E Obese, no rash, soft abdomen
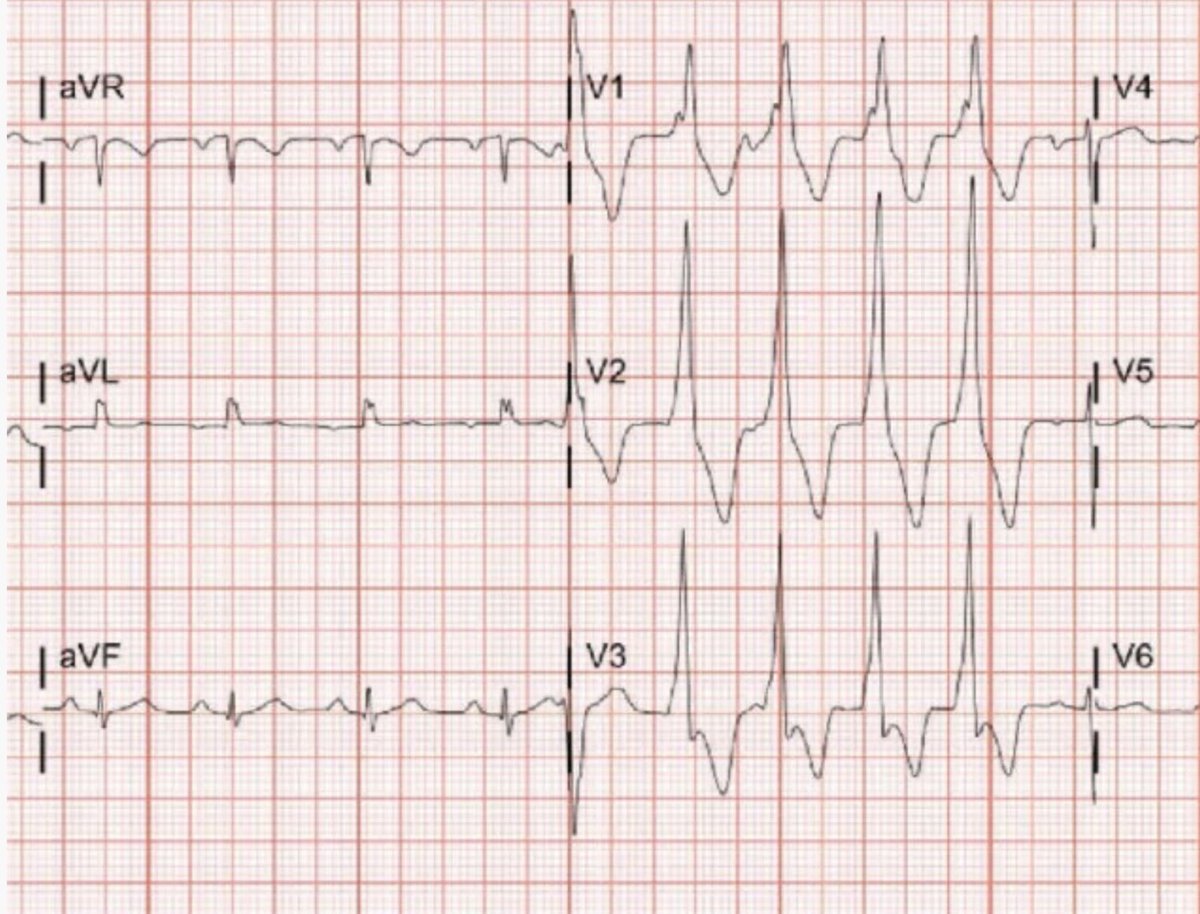
U bil B lines, RV=LV, EF~60%,
L pH 7.29, PCO2 35, Cr 1.4, Lactate 2.2 Hb10

A ETT 25cm
B SpO2 82% FiO2 1 Vt350 P12
❤️BP 110/80 HR 95, CapRef 1.5”
D avpU (propofol)
E Obese, no rash, soft abdomen
U bil B lines, RV=LV, EF~60%,
L pH 7.29, PCO2 35, Cr 1.4, Lactate 2.2 Hb10

Patient got remdesivir & dexamethasone. SpO2 88% after bolus NMB & pulling ETT(3cm). As you increase PEEP to 18, driving pressure improves, but the SpO2 drops to 72% without hypotension. You decrease PEEP back to previous but SpO2 still 70s. The next step is: #FOAMcc #MedTwitter
1/ With inhaled NO SpO2 improved to 97%, and after 2h FiO2 was down to 40% and rapid weaning.
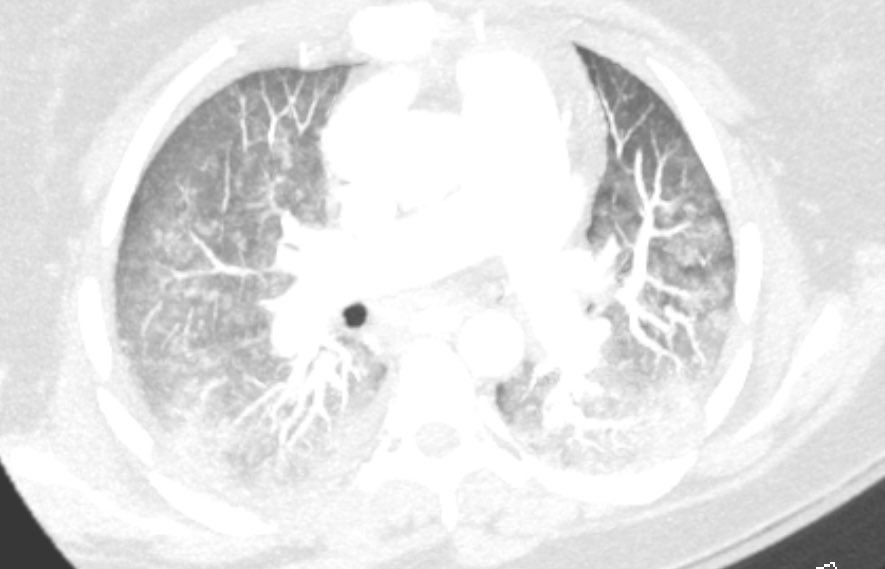
Bubble study confirms suspected intermittent #PFO shunt which occurs in up to 19% #ARDS with ⬆️rescue Rx & ⬇️VFD
pubmed.ncbi.nlm.nih.gov/20601861/
pubmed.ncbi.nlm.nih.gov/33252722/
pubmed.ncbi.nlm.nih.gov/33150525/
Bubble study confirms suspected intermittent #PFO shunt which occurs in up to 19% #ARDS with ⬆️rescue Rx & ⬇️VFD
pubmed.ncbi.nlm.nih.gov/20601861/
pubmed.ncbi.nlm.nih.gov/33252722/
pubmed.ncbi.nlm.nih.gov/33150525/

2/ A paradoxic response to PEEP with severe ⬇️O2 despite improvement in compliance, and in the absence of hypotension is suggestive of R to L shunt through PFO (due to ⬆️PA/RV pressure). If available, iNO can quickly reduce RV pressure leading to shunt closure; prone can help too 

• • •
Missing some Tweet in this thread? You can try to
force a refresh