1/ Covid (@UCSF) Chronicles, Day 282
Holiday greetings – hope you’re getting a little R&R. I’m on clinical svc @ucsfhospitals – welcome break from a Life of Zoom, leavened by a little Netflix. Today, update on Covid in SF/CA, & lessons from first 2 wks of vaccine distribution.
Holiday greetings – hope you’re getting a little R&R. I’m on clinical svc @ucsfhospitals – welcome break from a Life of Zoom, leavened by a little Netflix. Today, update on Covid in SF/CA, & lessons from first 2 wks of vaccine distribution.
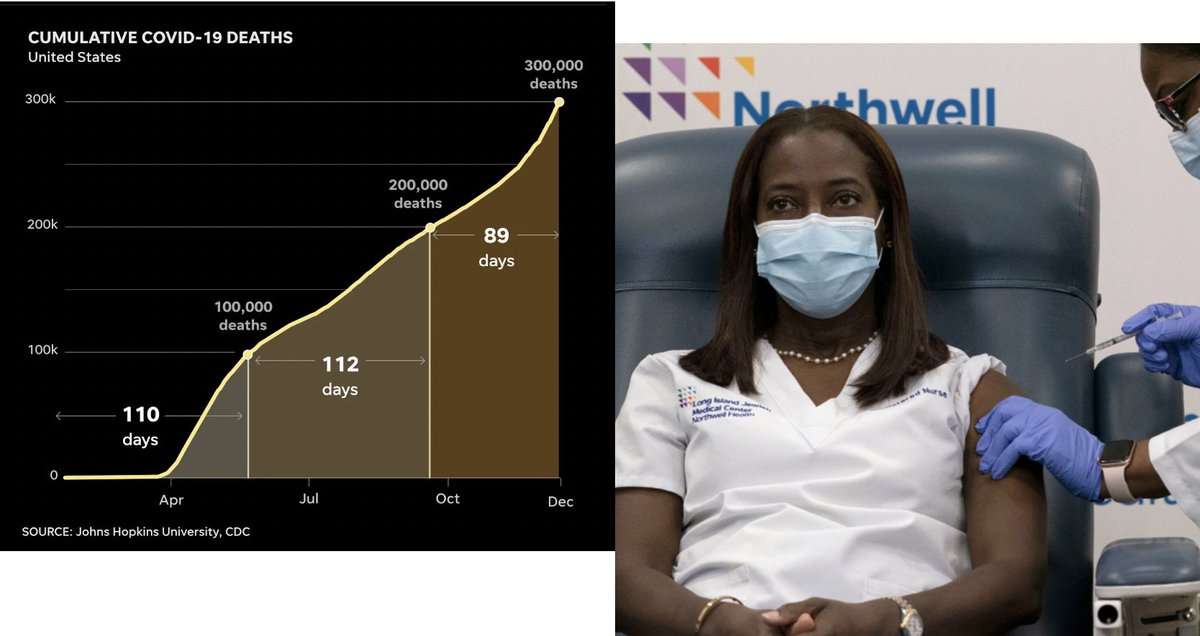
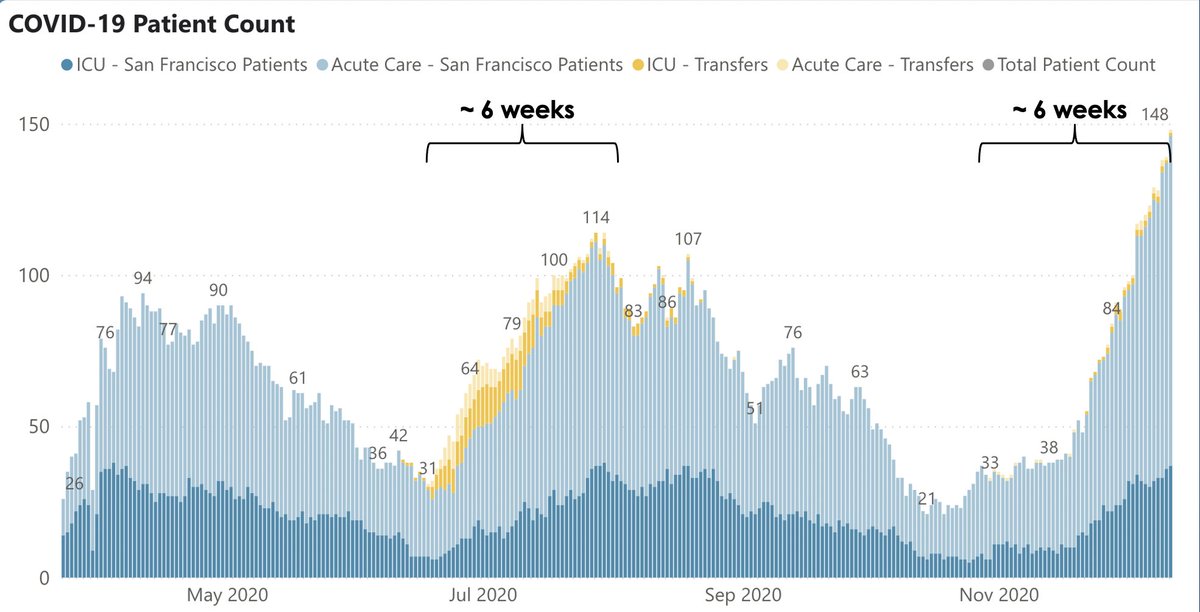
2/ @UCSFHospitals, 60 pts in hospital, 12 on vents (Fig on L). Curve shows we may have plateaued – at a pretty high # but one that isn’t overly stressing system. Our test positivity rates (Fig R) have inched down a bit in the past week. Maybe things are starting to turn around. 



3/ SF cases up to 288/d (Fig L) – low when compared to many regions (incl. SoCal), but 10x SF's Oct cases. Test positivity still inching up, now 4.3%. 176 Covid pts in SF hospitals; perhaps hint of a plateau? (Fig R). Cumulative deaths=178, w/ only 12 in past 30d – amazingly low. 


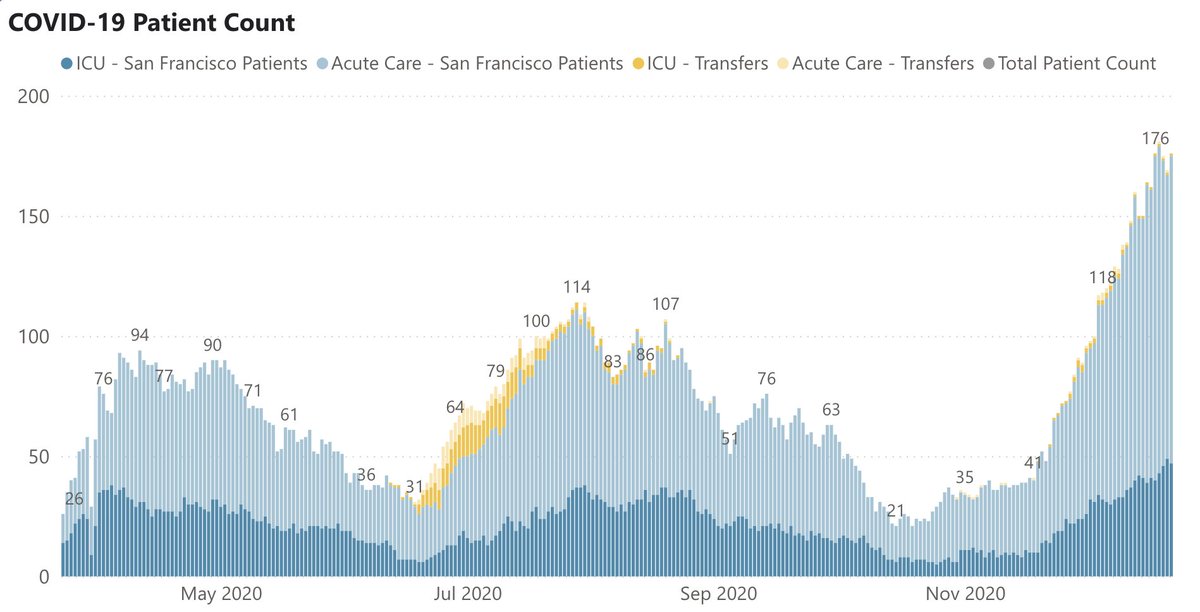
4/ The overall picture for SF is that, yes, we’re having a real surge, but things are not out of control, either @UCSF or the city. Kudos to our public health leaders, & to San Franciscans for continuing to follow guidelines. That’s what’s keeping the city from being overwhelmed.
5/ In contrast, the situation in Southern California is awful. This figure, from @sfchronicle, shows the tale of 2 cities: LA vs. SF. The contrast is important to see, as the “CA surge” has become a national story. It's really a story of two very different epidemics in one state. 

6/ LA’s #'s are eye-popping: 16,525 cases/d; 6,155 Covid pts in LA hospitals (Fig L); 145 died yesterday; total deaths 9,153; test pos. rate: 16.3% (Fig R). Yes, LA has more people than SF, but only 11x more. So, per capita, SoCal experience is order of magnitude worse than SFs. 



7/ Driven mostly by LA surge, for the 1st time CA leads the U.S. in Covid cases (Fig). Thankfully, U.S. overall seems to have plateaued, mostly due to a big drop in the Midwest, after a brutal 2 months. Sadly, this could all pick up again, based on behavior over Xmas & New Year. 

8/ Let’s turn to lessons learned from the first 2 weeks of vaccine distribution. Distribution of Pfizer vaccine began ~14d ago; Moderna's last week. Our experience to date mostly comes from large healthcare organizations, though nursing homes are starting to vaccinate residents.
9/ The first vaccination programs were in large hospitals that enjoy robust computer systems, HR systems that can sort & track all their employees, w/ generally collaborative cultures in which MDs, RNs & administrators learn to work together in what can be a charged environment.
10/ You’d think that, if anybody can get vaccine distribution right, it would be in places like this, right? Yet we've heard many stories of chaos & conflict, such as the protests @StanfordMed over an algorithmic distribution process that favored older...tinyurl.com/y9bkn6g3
11/ …but clinically inactive faculty over residents, & the struggles @MassGenBrigham tinyurl.com/ydf5wvz6, where a computer program designed to allocate first come-first served led to resentment by night shift workers who missed their invites (the program ultimately crashed).
12/ Then came today’s @nytimes story about @nyphospital & @MountSinaiNYC Hospitals tinyurl.com/y85w7pdu, where stories of cheating & line jumping seem like vaccine distribution by way of Lord of the Flies. I think we got it right @UCSF: we bucketed our people into 4 groups…
13/ … based on Covid exposure risk and gave departments an opportunity to review the lists & suggest changes if people were mis-categorized. Then – within each group – we chose people by random draw, giving them an opportunity to schedule their vaccination over the next 4 days.
14/ A few lessons emerge. First, this is rationing of a scarce & precious resource: tough stuff. Knowing that it’ll get better in time (ie, if you don’t get a shot now, you will in 1-3 months) is small comfort, particularly when the stakes can be – or feel like – life or death.
15/ Second, communication is key & establishing trust is paramount. People have to believe the system is fair & won’t be gamed: by VIP faculty, leaders, donors, or anybody. Third, across-group comparisons are inevitable. @UCSF, random selection meant that, within a given group…
16/… a janitor or transporter might go before a department chair. And leaders w/ no patient contact would be in the lowest priority group. Fourth, while distribution order seems like the dominant issue (it’s certainly the most charged one), logistics & IT systems matter as well.
17/ It takes time to vaccinate thousands of people – they need to sign in, fill out questionnaires, get their shots, & wait for 15-30 minutes to be sure they don’t have a reaction. Meanwhile, tracking systems have to know who got which vaccine when. This will become even more…
18/ …complicated if additional vaccines are approved.
While today’s worry is about vaccine supply, it may be the actual process of getting people vaccinated – the nuts and bolts of getting shots into people’s arms – that proves to be the bottleneck in reaching herd immunity.
While today’s worry is about vaccine supply, it may be the actual process of getting people vaccinated – the nuts and bolts of getting shots into people’s arms – that proves to be the bottleneck in reaching herd immunity.
19/ We’re lucky that the 2 available vaccines (Pfizer & Moderna) use the same technology & seem equal in efficacy & safety. A coming flashpoint may be if @US_FDA approves a vaccine (such as @AstraZeneca) that's less effective (AZ was ~70% effective in clinical trial) and people…
20/ … begin shopping (w/ sharp elbows) for their preferred shot. And things'll get even more dicey as we move to the next groups for vaccination. While sorting by older age will be relatively easy (driver’s license or similar), expect more battles when we try to figure out who…
21/ is an essential worker & who has an underlying health condition. If plan is “the honor system,” as it currently seems to be tinyurl.com/y9wmkhmu, well, the rocky experience in hospitals to date may be a dress rehearsal for a real dumpster fire. I’m old enough to remember…
22/ …gas rationing during 1973 oil crisis tinyurl.com/y73g9oq3 System was odd/even; if your license plate’s last digit was odd, you got gas on odd days. Ditto even. It wasn’t perfect, but it was transparent, simple, & mostly fair. Perhaps we should consider it for vaccines.
23/ I'll have more to say about vaccination in the next week or two, including further thoughts on immunity passports, how being vaccinated is changing behavior (among both the vaccinated and those who are waiting), & what we’re learning about Covid vaccine hesitancy. At least...
24/ …@UCSF, vast majority of people who've received the magic email informing them that they’re eligible for their shot have said yes. But this is probably on the same gene as our high rate of mask wearing: SF people, as well as healthcare workers, generally follow the evidence.
25/ Whether UCSF’s strong uptake is matched by the rest of the U.S. will be key question of 2021. When scarcity is no longer a limiting factor, whether folks choose vaccination will determine if & when our lives return to normal.
Oh, and happy 80th, Tony! tinyurl.com/yc6g68mz
Oh, and happy 80th, Tony! tinyurl.com/yc6g68mz
• • •
Missing some Tweet in this thread? You can try to
force a refresh