1/ People are hardwired to get infuriated when they see injustice.
But I fear that applying this lens to covid vaccine distribution will lead to more deaths not fewer.
Stanford has screwed up, again. Some people who shouldn't have gotten it, did.
nbcbayarea.com/news/local/rac…
But I fear that applying this lens to covid vaccine distribution will lead to more deaths not fewer.
Stanford has screwed up, again. Some people who shouldn't have gotten it, did.
nbcbayarea.com/news/local/rac…
2/ What's the natural response then, from those all the way down the distribution chain, from state administrators to hospital execs worried about "wrong people" getting vaccinated first?
You spend more time collecting data, parsing into finer and finer gradations
You slow down
You spend more time collecting data, parsing into finer and finer gradations
You slow down
3/ Hospitals and nursing homes don't release more to staff until every i has been dotted.
States don't release more to hospitals and nursing homes until they've used up allotment
feds don't release more to states
Amidst a vaccine shortage, available supply sits in warehouses.
States don't release more to hospitals and nursing homes until they've used up allotment
feds don't release more to states
Amidst a vaccine shortage, available supply sits in warehouses.
4/ this is a good thread by @ashishkjha about the cascade of failed accountability and the last mile problem.
And I have my own indignation about how distribution has been prioritized.
Frontline PCPs can't get vaccine while SNF HVAC techs get it 😤
And I have my own indignation about how distribution has been prioritized.
Frontline PCPs can't get vaccine while SNF HVAC techs get it 😤
https://twitter.com/ashishkjha/status/1343768405116153858?s=19
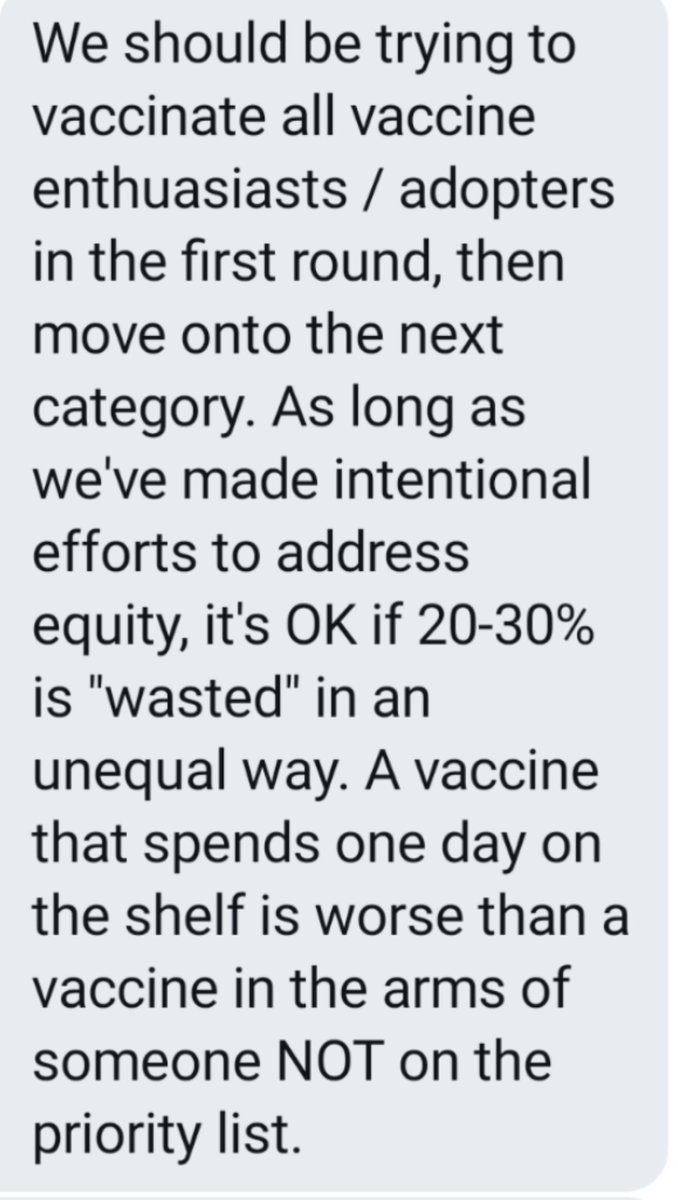
5/ But the fact remains that we have millions of doses sitting in warehouses because people are worried about screwing up prioritization
The system is stopped up, and needs disimpaction, not surgical precision
...and we should use the normal channels we use to give vaccines
The system is stopped up, and needs disimpaction, not surgical precision
...and we should use the normal channels we use to give vaccines
6/ I hope that @choucair and the incoming team consider how they can normalize these processes as vaccine supply ramps up even further (and I believe it will)
7/ and to return to where I started, we have to do this while deeply appreciating just how primal and powerful our reactions are to injustice.
If you haven't seen the cucumber-grape experiment video, it's worth a look :-)
If you haven't seen the cucumber-grape experiment video, it's worth a look :-)
8/ I appreciate the DMs from public health and hospital leaders saying in essence "this is exactly the problem we are having, but we can't talk about it publicly"
👇
👇
• • •
Missing some Tweet in this thread? You can try to
force a refresh