
#Cough 🫁🌬️ is important for ejecting foods and liquids from the #lungs to prevent #asphyxiation and #aspiration #pneumonia. In this tutorial, we will discuss why and how to assess voluntary #cough as a way to enhance your clinical #swallow evaluation. (Warning: long thread!) 
Evaluating #cough is important three reasons. First, weak coughs (#dystussia) are associated with #dysphagia and #aspiration in many patient populations. Therefore, assessing cough can improve the accuracy of predicting and identifying someone with #dysphagia.
Second, assessing #cough provides a more holistic understanding of #airway protection. In other words, we should try to understand how well a patient with #dysphagia can clear #aspirate material from the airway, in addition to understanding how frequently/severely they aspirate. 
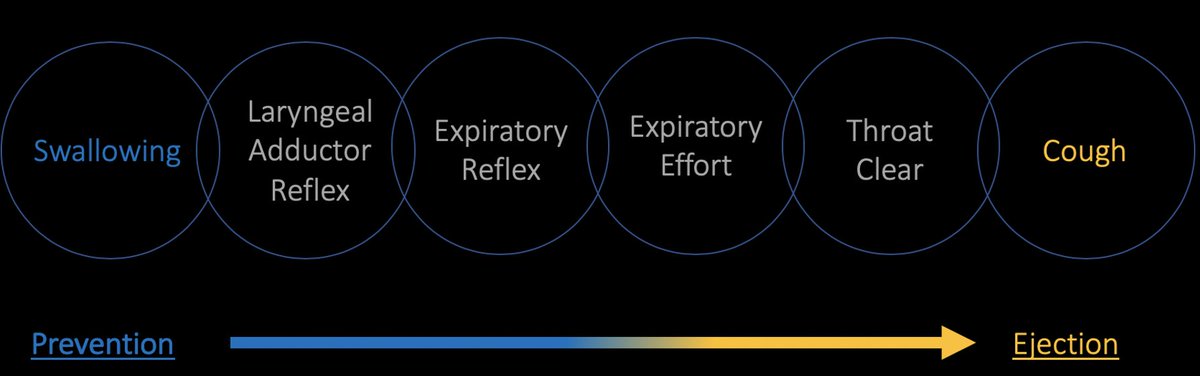
Third, if voluntary #cough is assessed and found to be impaired, then it may also be an important and clinically feasible therapy target to include in a one's rehabilitation plan 🧠💪🏋️♀️ (stay tuned for an upcoming tutorial on voluntary cough skill training! #VCST).
Two types of voluntary coughs can be assessed clinically: “single” 🗣️💨 and “sequential” 🗣️💨💨💨 voluntary coughs. For each, provide a verbal instruction and an audio-visual model (see below).
Single Voluntary Cough
Verbal instruction: “Cough hard once, like this.”
Audio-visual model: Take a deep breath in and then cough hard once.
Verbal instruction: “Cough hard once, like this.”
Audio-visual model: Take a deep breath in and then cough hard once.
Sequential Voluntary Cough
Verbal instruction: “Cough as if something went down the wrong pipe. It might look something like this.”
Audio-visual model: Take a deep breath in and then perform a three-cough epoch (i.e., one breath in followed by three coughs).
Verbal instruction: “Cough as if something went down the wrong pipe. It might look something like this.”
Audio-visual model: Take a deep breath in and then perform a three-cough epoch (i.e., one breath in followed by three coughs).
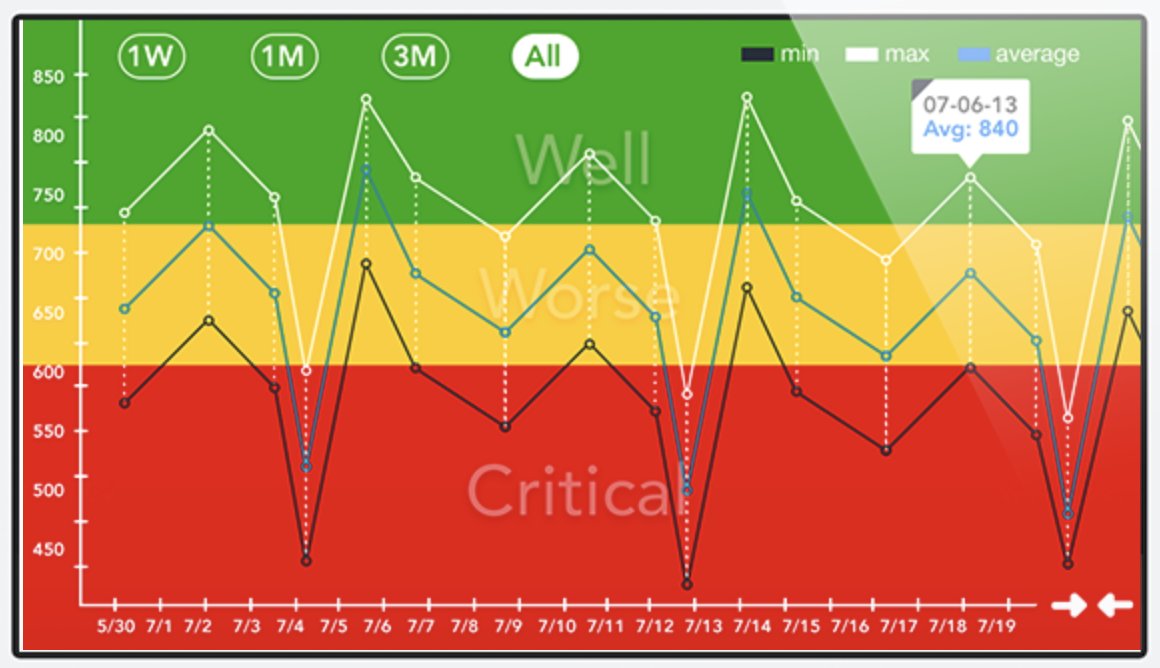
The patient should complete three trials of each (minimum) so you can assess the average and #variability in #cough strength 💪🏋️♀️📏. Coughs can then be assessed using subjective (audio-perceptual) and objective (instrumental) methods (see below).
Audio-perceptual assessment involves subjectively listening 🗣️💨👂 for cough strength (weak/strong), quality (normal, breathy, strained, effortful, discoordinated, throat clear), and effectiveness (effective/ineffective).
Objective methods involve coughing into instruments capable of measuring airflow 🗣️💨📏👩🔬. Handheld peak flow meters can be used as a cheap, portable, and feasible method to objectively assess single and sequential #cough peak expiratory flow rate (#PEFR).
Compare #cough #PEFR to healthy norms and values associated with #dysphagia & #aspiration. More comprehensive norms need to be developed, but I consider PEFR <300 L/min to be abnormal. See my below slide for some references and my general (informal) interpretation guide. Cheers! 

• • •
Missing some Tweet in this thread? You can try to
force a refresh


