1/ read this @adamcancryn @tylerpager piece, and let's discuss some of the points raised
‘There is a palpable concern’: Biden presses advisers over 100 million Covid shot goal politi.co/2XHhk1f
‘There is a palpable concern’: Biden presses advisers over 100 million Covid shot goal politi.co/2XHhk1f
2/ first, I am so glad @JoeBiden *is* putting a hard to reach goal out there
When @matkendall and I set our first public targets
@ONC_HealthIT a longtime fed told us "never give them a date AND a number"
It's risky, it's gutsy, and it's the right thing to do for the country.
When @matkendall and I set our first public targets
@ONC_HealthIT a longtime fed told us "never give them a date AND a number"
It's risky, it's gutsy, and it's the right thing to do for the country.
3/ It will be very hard to hit 100M in 100 days
But the very fact that this article was written EVEN BEFORE THEY START points to the intense focus it brings.
The new admin may miss their first big test, but vaccinate tens of millions more than if they shunned responsibility
🇺🇸
But the very fact that this article was written EVEN BEFORE THEY START points to the intense focus it brings.
The new admin may miss their first big test, but vaccinate tens of millions more than if they shunned responsibility
🇺🇸
4/ I'm also really happy to hear that @JoeBiden is "urging advisers to avoid generalities and drill down on the particulars"
The details are everything in a job like this. It's not enough to say, breezily, we give it to the states, then it's their problem.
That approach failed
The details are everything in a job like this. It's not enough to say, breezily, we give it to the states, then it's their problem.
That approach failed
5/ "Pushing on details" <> "don't trust the team"
“He wants to know about the practical details. I think that’s a good thing because that makes sure the plans are grounded in reality, but I don’t take from those conversations that he doesn’t believe in his team.”
@vivek_murthy
“He wants to know about the practical details. I think that’s a good thing because that makes sure the plans are grounded in reality, but I don’t take from those conversations that he doesn’t believe in his team.”
@vivek_murthy
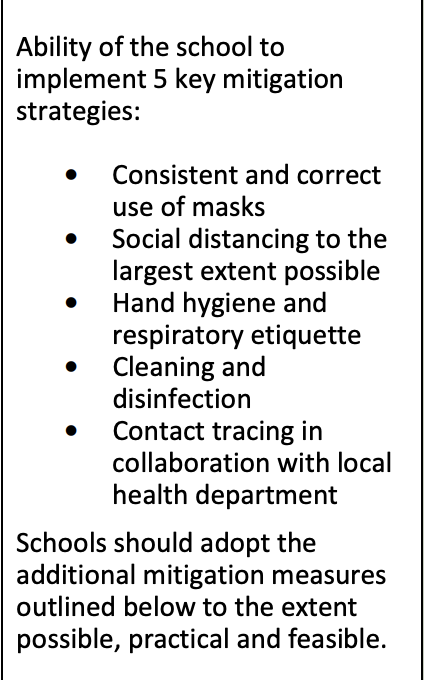
6/ and what is going to change, to make 10M a reality?
These strategies are good, but there's one big piece of advice I would have for @JeffZients @NQuillian @choucair
In a public health emergency, take advantage of the systems we use during peacetime
primary care practices
These strategies are good, but there's one big piece of advice I would have for @JeffZients @NQuillian @choucair
In a public health emergency, take advantage of the systems we use during peacetime
primary care practices
7/ Yes, we do need to give state and local public health officials more resources, but also more guidance and more tools.
For all the parlor generals out there- read this searing interview w a Florida county manager- would you do better? are you sure?
washingtonpost.com/nation/2021/01…
For all the parlor generals out there- read this searing interview w a Florida county manager- would you do better? are you sure?
washingtonpost.com/nation/2021/01…
8/ Yes, we need feds to not abdicate their role and engage directly (c/f testing debacle)
Setting up field centers to cover high volume urban centers as well as underserved rural areas makes sense.
But we also need to open the CDC's (non-state) pipeline beyond CVS/Walgreens
Setting up field centers to cover high volume urban centers as well as underserved rural areas makes sense.
But we also need to open the CDC's (non-state) pipeline beyond CVS/Walgreens
9/ This is the system CDC has established to take orders for the vaccine supply purchased by the feds and to get them shipped (by McKesson) to the recipients.
Right now, the only "provider organizations" getting vaccine from CDC (vs states) are the pharmacies
Expand this pipe
Right now, the only "provider organizations" getting vaccine from CDC (vs states) are the pharmacies
Expand this pipe

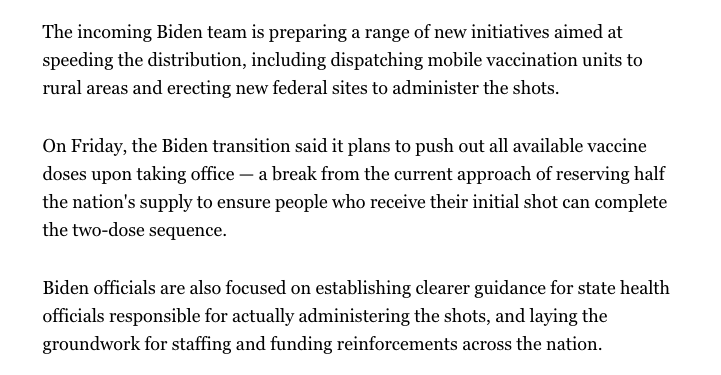
10/ Yes, pushing out more vaccine doses so they are not sitting in federal warehouses is good.
But we have a huge "last mile" problem.
Feds -> State -> Hospitals -> ? -> High risk elderly
Trickle down from hospitals with excess doses before they spoil is not a good plan.
But we have a huge "last mile" problem.
Feds -> State -> Hospitals -> ? -> High risk elderly
Trickle down from hospitals with excess doses before they spoil is not a good plan.
11/ Non-hospital physician practices can't even figure out how to get their own staff vaccinated.
https://twitter.com/rshawnm/status/1347538646174474241?s=20
12/ We need willing arms as well as vaccine supply- that's why a large portion of annual vaccines are given by community PCPs
Given vaccine resistance in many, it will be critical to have trusted practices *proactively reach out* to high risk patients
Given vaccine resistance in many, it will be critical to have trusted practices *proactively reach out* to high risk patients
https://twitter.com/rshawnm/status/1347547187178303488?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh