Our recent work on vaccine prioritization for COVID-19 is now published in @ScienceMagazine, but this paper has evolved because of both formal and informal peer review. So while the paper is linked, here's a quick summary of the results. 🧵 1/
science.sciencemag.org/content/early/…
science.sciencemag.org/content/early/…
First, rather than reading another Twitter summary, there's a great discussion of this work in the broader context of vaccination strategies by two vaccine/modeling experts @MeaganCFitz @Alison_Galvani. Highly recommended for both theory & history. 2/
science.sciencemag.org/content/early/…
science.sciencemag.org/content/early/…
IMO there are 2 intuitive ideas in vaccine prioritization:
Intuition 1: directly protect the vulnerable.
Intuition 2: vaccinate to break transmission chains & indirectly protect vulnerable.
When intuition supports two opposing conclusions, don't use intuition—use math. 🤓 3/
Intuition 1: directly protect the vulnerable.
Intuition 2: vaccinate to break transmission chains & indirectly protect vulnerable.
When intuition supports two opposing conclusions, don't use intuition—use math. 🤓 3/
We used an SEIR model with age groups by decade, and considered variation in:
* vaccine efficacy
* transmission-blocking effects
* rollout speed
* demography & contact patterns
* IFR [by age]
* existing antibodies
* vaccine hesitancy
Then, we simulated 1 year of transmission. 4/
* vaccine efficacy
* transmission-blocking effects
* rollout speed
* demography & contact patterns
* IFR [by age]
* existing antibodies
* vaccine hesitancy
Then, we simulated 1 year of transmission. 4/
By comparing vaccine rollouts to a no-vaccine scenario, we measured reductions in (a) mortality, (b) total infections, and (c) years of life lost.
This allowed us to see which intuition would actually save more lives: protect the vulnerable or move toward herd immunity? 5/
This allowed us to see which intuition would actually save more lives: protect the vulnerable or move toward herd immunity? 5/
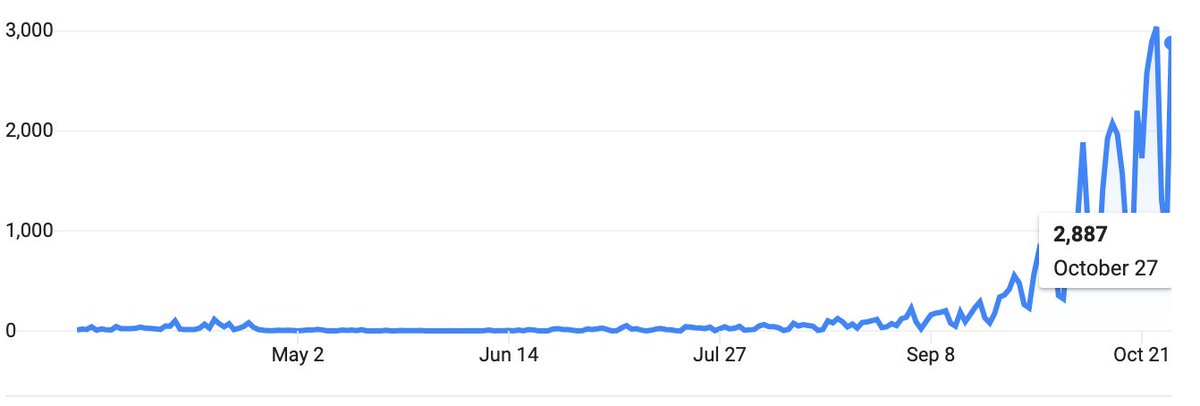
The left plot shows the 5 strategies we investigated. On the right, there are simulation outputs for no vaccine (dashed line) and with vaccines rolled out out at 0.2% of the population per day (grey area).
The purple line (60+) ends in fewer deaths in both columns. 6/
The purple line (60+) ends in fewer deaths in both columns. 6/

It would take forever to look at tons of individual plots so instead, we summarized impacts across vaccine supply levels.
Here, for any vaccine supply between 0% and 50%, in this scenario (see paper), prioritizing adults 60+ reduces mortality more than alternatives. 7/
Here, for any vaccine supply between 0% and 50%, in this scenario (see paper), prioritizing adults 60+ reduces mortality more than alternatives. 7/

These curves depend on the scenarios and parameters, so we created an interactive calculator using the same mathematical model as the paper.
You can explore various scenarios, countries, vaccines, and rollout speeds. ⤵️
vaxfirst.colorado.edu 8/
You can explore various scenarios, countries, vaccines, and rollout speeds. ⤵️
vaxfirst.colorado.edu 8/
To build a broader understanding, it helps to be able to view a lot of simulations at once (h/t Reviewers 😎) and see which strategy was BEST to ⬇️ mortality.
For example, here are 2000 combinations of vaccine rollout speed, supply, & transmission. Purple=prioritize 60+ best. 9/
For example, here are 2000 combinations of vaccine rollout speed, supply, & transmission. Purple=prioritize 60+ best. 9/

👆 notice that this plot shows that IF we could keep transmission low from here on out (low R), and IF the vaccine blocks transmission, then we might also consider prioritizing those 20-49 (teal).
But if vaccines block transmission poorly, this plot becomes all purple (60+). 10/
But if vaccines block transmission poorly, this plot becomes all purple (60+). 10/
In the paper, we show lots of other scenario combinations, that help explore unknowns:
* How well does vaccine block transmission?
* Does efficacy hold up for older folks?
* Do results vary by country?
* How important is rollout speed?
* What add'l vax options do Taiwan, NZ have?
* How well does vaccine block transmission?
* Does efficacy hold up for older folks?
* Do results vary by country?
* How important is rollout speed?
* What add'l vax options do Taiwan, NZ have?
In general:
If the goal is to reduce mortality, prioritizing adults 60+ is the most robust way to achieve that goal across countries, vaccines, and current unknowns (transmission blocking, efficacy for older folks, etc). 12/
If the goal is to reduce mortality, prioritizing adults 60+ is the most robust way to achieve that goal across countries, vaccines, and current unknowns (transmission blocking, efficacy for older folks, etc). 12/
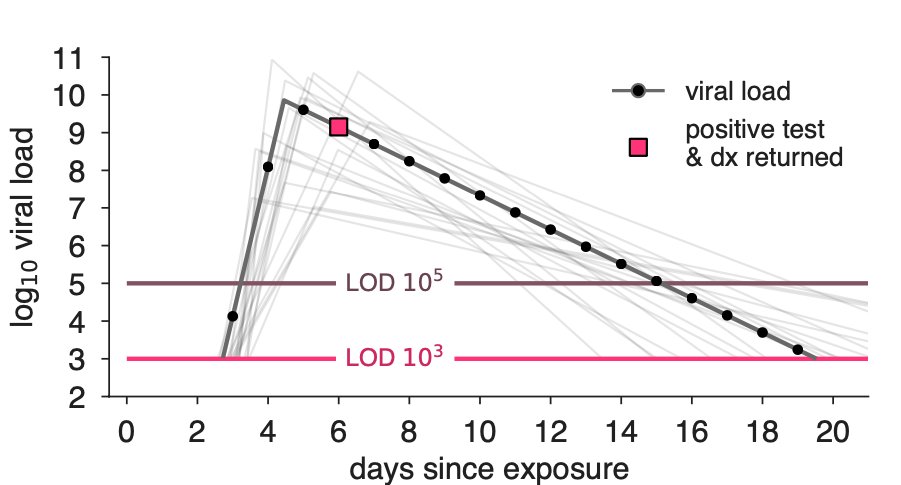
Finally, let's not forget that it's "vaccines AND..."
We can take other actions to save lives while we wait in the queue:
* reducing transmission by continuing to wear masks and avoiding indoor gathering,
* using rapid screening tests
* working to decrease vax hesitancy 13/
We can take other actions to save lives while we wait in the queue:
* reducing transmission by continuing to wear masks and avoiding indoor gathering,
* using rapid screening tests
* working to decrease vax hesitancy 13/
This work was driven by @bubar_kate, backed by a wonderful & generous team: @StephenKissler @mlipsitch @sarahcobey @yhgrad. Kyle Reinholt 🧙♂️built interactive tools. 14/14
📄 Paper: science.sciencemag.org/content/early/…
💻 Code: github.com/kbubar/vaccine…
📈 Online Tools: vaxfirst.colorado.edu
📄 Paper: science.sciencemag.org/content/early/…
💻 Code: github.com/kbubar/vaccine…
📈 Online Tools: vaxfirst.colorado.edu
• • •
Missing some Tweet in this thread? You can try to
force a refresh