1/ The Denmark variant story was pointed out by several people as being quite concerning- this line struck me - "Cases involving the variant are increasing 70 percent a week in Denmark, despite a strict lockdown"
But the actual data was hard to pin down- so I dug it up
But the actual data was hard to pin down- so I dug it up
https://twitter.com/Bob_Wachter/status/1353044436855312384
2/ "The U.K. variant was 2 percent of sequenced coronavirus cases the last full week of 2020. By the second week of January, it had risen to 7 percent."
But in the context of declining cases what does that mean?
No link to data in article but it's here: covid19genomics.dk/statistics
But in the context of declining cases what does that mean?
No link to data in article but it's here: covid19genomics.dk/statistics
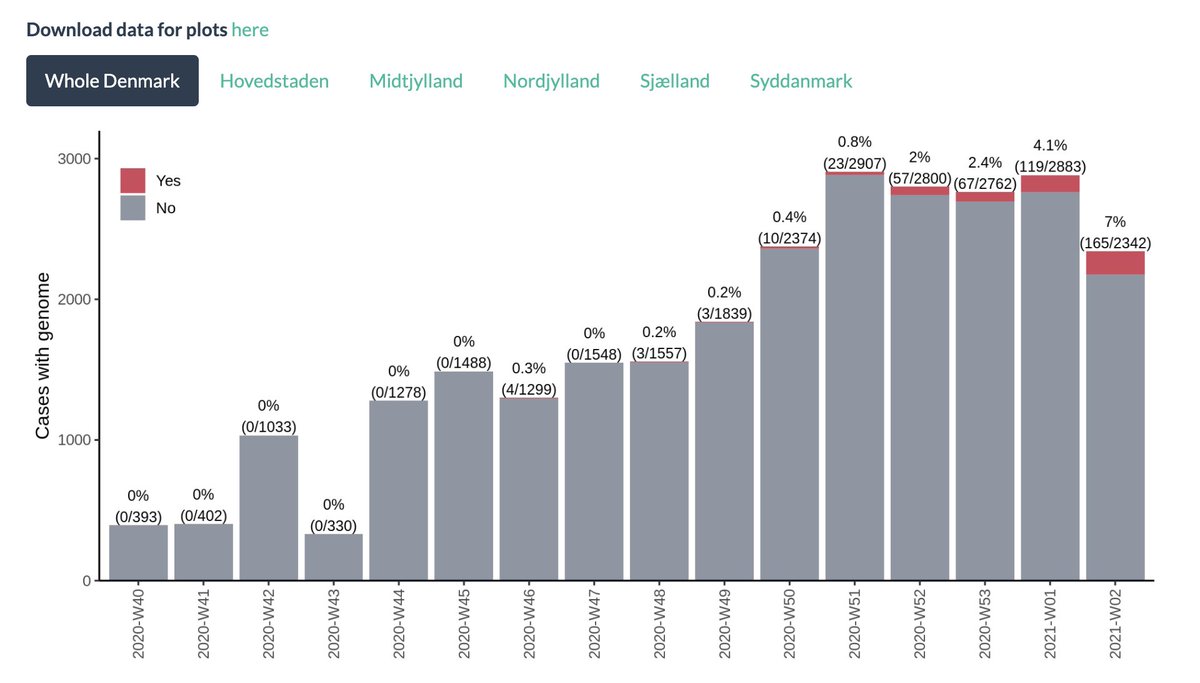
3/ But those aren't actually the true cases, cause despite the headline "Denmark is sequencing all coronavirus samples..." while they are *trying* to sequence all, the number of cases with a genome of sufficient quality relative to the total number of cases ranges w-w from 10-36% 
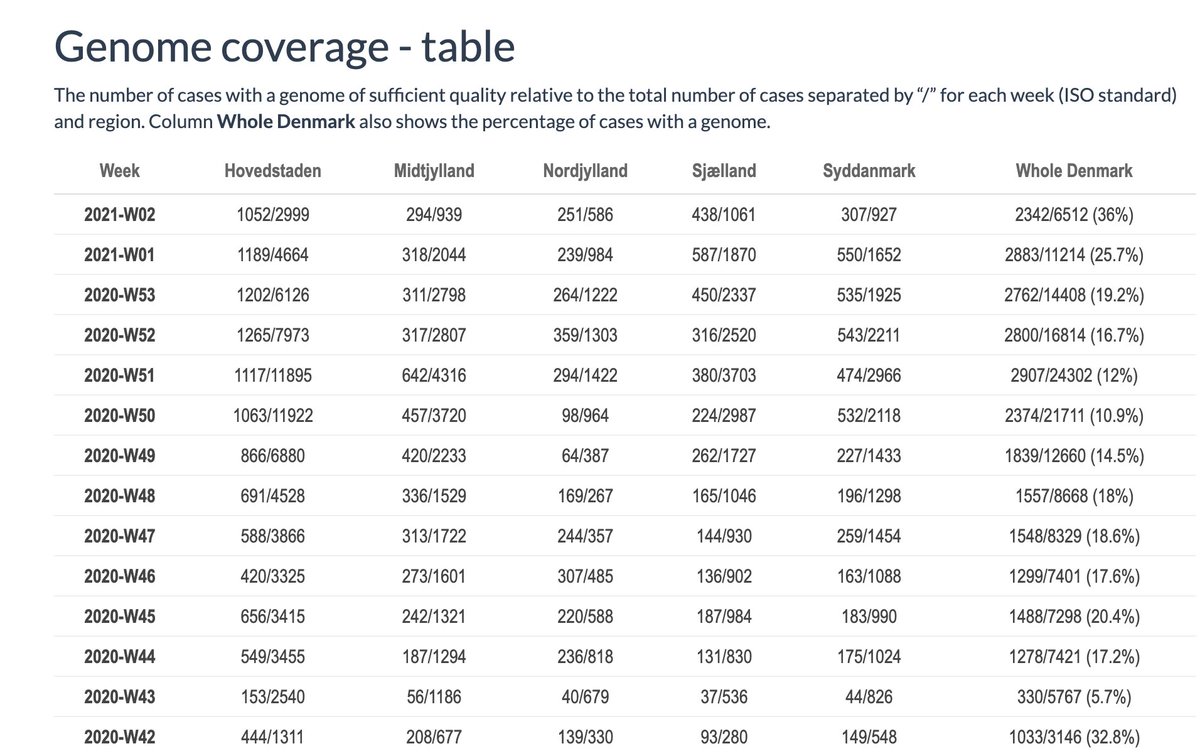
4/ In other words you need cases/week, variant rate and proportion tested to estimate the weekly number of the new variant in Denmark and understand how fast the variant is spreading.
This is what it looks like (yes, error bars had finite population adjustment, epi geeks)
This is what it looks like (yes, error bars had finite population adjustment, epi geeks)
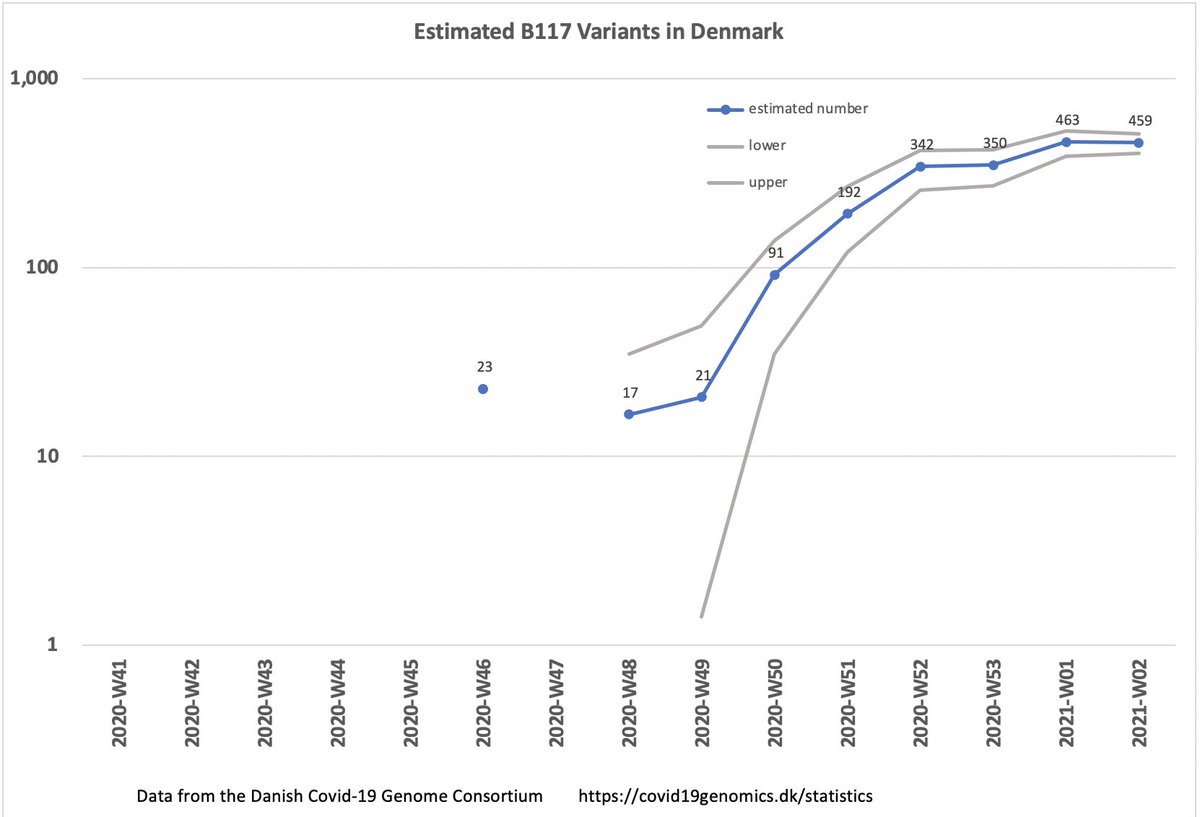
5/ That looks .... a lot better in recent weeks.
It looks like it hasn't doubled in past month.
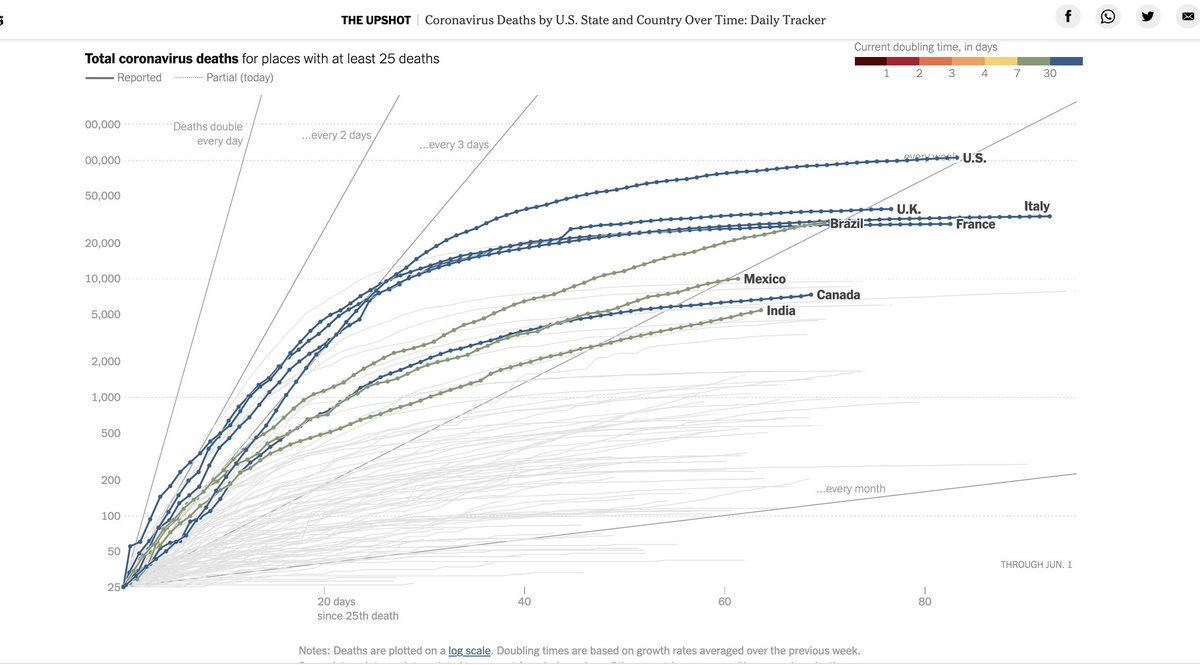
For context, here's what doubling time has looked like in different countries over time
The bottom-most line is doubling every month
It looks like it hasn't doubled in past month.
For context, here's what doubling time has looked like in different countries over time
The bottom-most line is doubling every month
6/ So, yes, a great explanation of exponential growth, but it appears that Denmark's restrictions have had a strong impact despite the new variant.
the initial spurt was certainly super concerning, but remember also that this outbreak is defined by lumpy super-spreader events
the initial spurt was certainly super concerning, but remember also that this outbreak is defined by lumpy super-spreader events
7/ The actual data from Denmark suggests a LOWER increase in infectiousness than original UK data, as
@trvrb has pointed out
Yes, it's a race between the variant and the vaccine, but we can't let ourselves get freaked out folks. What we knew worked before, still works
@trvrb has pointed out
Yes, it's a race between the variant and the vaccine, but we can't let ourselves get freaked out folks. What we knew worked before, still works
• • •
Missing some Tweet in this thread? You can try to
force a refresh