There is a stronger evidence basis for calorie counting as a core behavioral strategy for reducing food intake than “eating to satiety.”
Eating foods that reduce the risk of overeating and promoting satiety and less hunger is impt but this is an unproven behavioral strategy.
Eating foods that reduce the risk of overeating and promoting satiety and less hunger is impt but this is an unproven behavioral strategy.
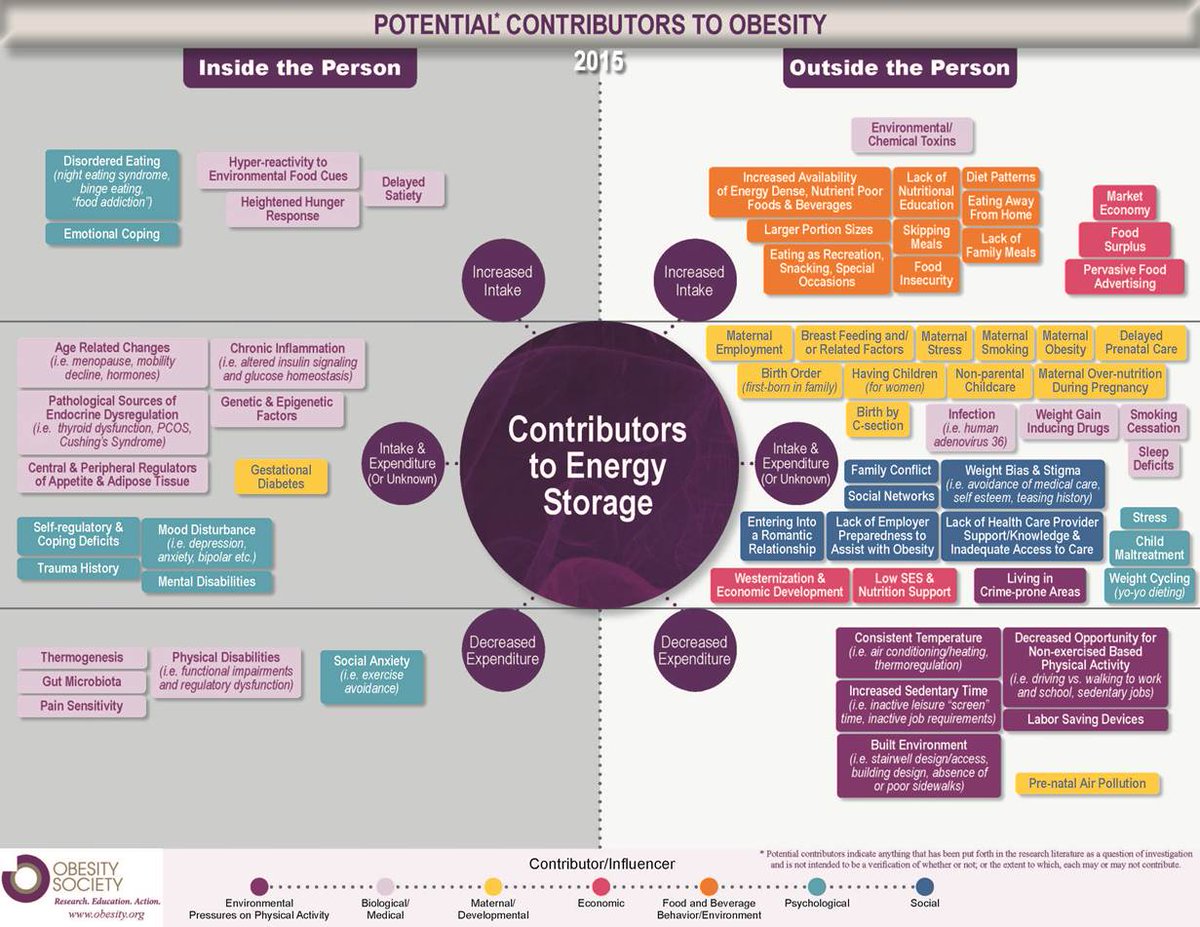
The reality is appetite is complex; regulated by a number of factors acting on two neural circuits. Also, we know people can eat past satiety given higher level neural circuitry involved in the complex regulation of feeding. But, hey, people like oversimplifying things. 🤷🏼♂️ 

People struggle to be healthy in an OB environment, and w/o monitoring, typically overeat without knowing. Calorie counting serves as a way to self-monitor and should not be viewed as an "exact science." People pushing this narrative have no idea what they are talking about.
Basically, every effective long-term behavioral study incorporates some aspect of calorie-counting or food journaling to facilitate self-monitoring.
People do not know how much they eat: nejm.org/doi/full/10.10…
Self-monitoring: ncbi.nlm.nih.gov/pmc/articles/P…
Effective behavioral approach w/ Calorie Counting: pubmed.ncbi.nlm.nih.gov/27670400/
Self-monitoring: ncbi.nlm.nih.gov/pmc/articles/P…
Effective behavioral approach w/ Calorie Counting: pubmed.ncbi.nlm.nih.gov/27670400/
Also, eating to satiety may not even be an effective strategy because the brain of individuals with obesity is more sensitive to hunger and less sensitive to satiety: sciencedirect.com/science/articl…
My opinion is a combo of behavioral and psychological approaches most c/w acceptance-based therapy that utilizes psychological flexibility and trains the pre-frontal cortex to deal with uncomfortable thoughts & feelings around food is the best strategy: pubmed.ncbi.nlm.nih.gov/30344017/
@DavidMacklinMD thoughts?
• • •
Missing some Tweet in this thread? You can try to
force a refresh