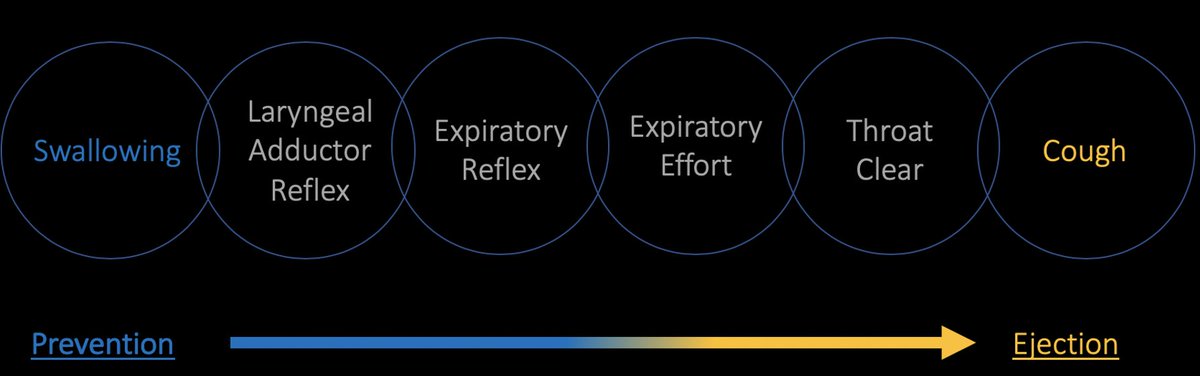
Ever wonder how to rehabilitate weak and ineffective #cough 🗣️💨 in people with #dysphagia 😷? In this tutorial, we will discuss how to train voluntary cough function through Voluntary Cough Skill Training (#VCST).
#VCST is a treatment paradigm intended to improve the accuracy 🏹🎯 and consistency of performing strong 💪 and effective coughs in people with #dystussia in order to increase the ability to eject #penetrant and #aspirate material from the #larynx and #lungs 🫁 after #swallowing.
#VCST is a skill-training treatment paradigm used to target single 🗣️💨 and sequential 🗣️💨💨💨 voluntary #cough. There is not a strict protocol to adhere to. Instead, the practice conditions for #VCST should be guided by principles of #motorlearning 🧠
Below, I will take you through general considerations for skill-training treatment planning, and use the attached article 📚 as an example of how to apply these considerations specifically to #VCST.
pubs.asha.org/doi/abs/10.104…
pubs.asha.org/doi/abs/10.104…
First, determine the number of reps/set, sets/session, sessions/day, and days/week📈. For #VCST, you may consider 5 reps/set, 10 sets/session, 1 session/day, 3 days/week, 4 weeks 🗓️. This could be completed for both single and sequential coughs (20 sets/session total).
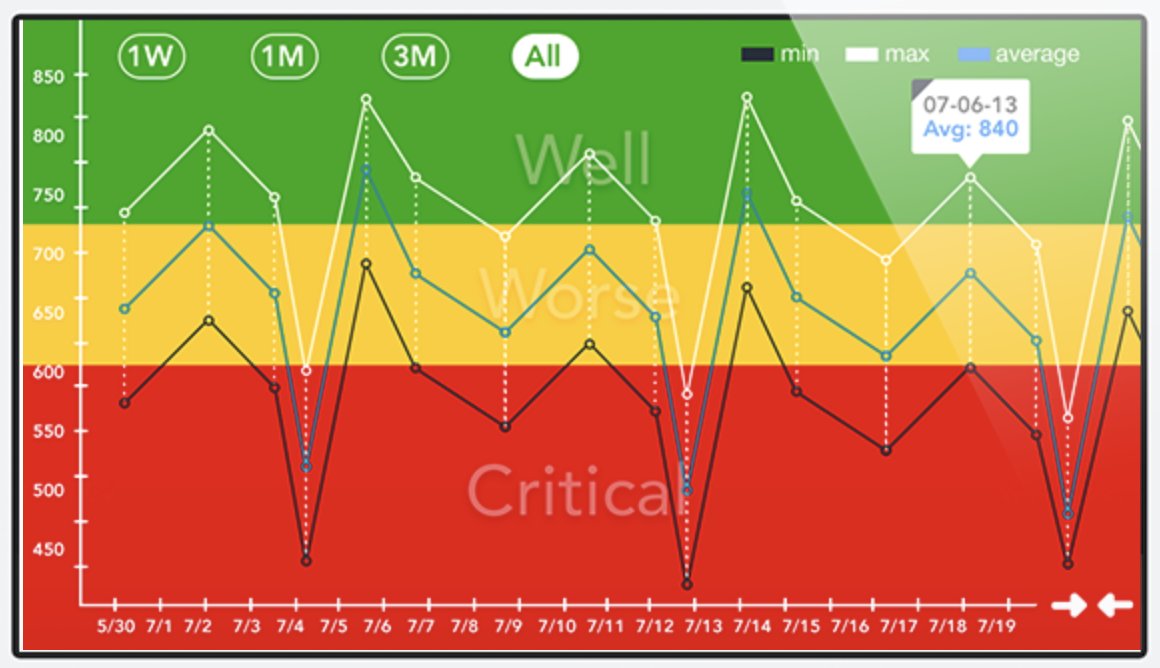
Second, create a 'performance bandwidth' rule to determine the type, timing, and frequency of feedback. For example, provide accuracy feedback after every 5 trials following sets of ≥80% accuracy, but provide accuracy and prescriptive feedback after sets of <80% accuracy.
Third, determine the role of constant vs variable practice. Research in the limb literature often finds #variablepractice may enhance #motorlearning. Therefore, you may consider 6 sets of “strong” coughs, 2 sets of “weak” coughs, and 2 sets of “medium-strong” coughs 

Consider purchasing a handheld peak flow meter to facilitate #VCST. Peak flow meters serve two purposes. First, they are used to evaluate voluntary cough (see previous tutorial). Second, they can be used to objectively determine the accuracy of each weak/strong practice trial. 

As a loose guideline, you may consider “weak” coughs to be 60-150 L/min, “medium-strong” coughs to be 150-250 L/min, and “strong” coughs to be >250 L/min. If your peak flow meter as movable markers, set them accordingly
Here is an example of strong, weak, and medium strong single voluntary coughs.
Here is an example of strong, weak, and medium-strong sequential voluntary coughs.
Don’t forget! Motor performance does not necessarily represent #motorlearning. Someone may demonstrate low accuracy the first few training sessions, but may in fact be learning! Motor learning is inferred through increased accuracy, consistency, retention, and generalization.
See below article as an additional reference.
pubs.asha.org/doi/full/10.10…
journals.physiology.org/doi/full/10.11…
frontiersin.org/articles/10.33…
sciencedirect.com/science/articl…
pubs.asha.org/doi/full/10.10…
journals.physiology.org/doi/full/10.11…
frontiersin.org/articles/10.33…
sciencedirect.com/science/articl…
As an FYI, I'll be adding this tutorial, along with others, to my professional website at jamescurtis.me in the next few weeks.
Correction: jamescurtisphd.me
• • •
Missing some Tweet in this thread? You can try to
force a refresh