#Rheumatology Fun
Let’s take a deep dive into a unique subset of rheumatic diseases 👇
This week's RTL guest tweetorial from @MithuRheum!
Let’s take a deep dive into a unique subset of rheumatic diseases 👇
This week's RTL guest tweetorial from @MithuRheum!
CASE 1:
🔹A 52 yo male presents to clinic w/ 6 months of hand ulcerations on the dorsal surface of the hands & elbow, oral ulcers, a violaceous periorbital rash and mild arthralgias
🔸CT chest demonstrates nodular opacities
🔹A 52 yo male presents to clinic w/ 6 months of hand ulcerations on the dorsal surface of the hands & elbow, oral ulcers, a violaceous periorbital rash and mild arthralgias
🔸CT chest demonstrates nodular opacities

Based on the clinical presentation and photograph of the ulcers, which of the following is the most likely diagnosis?
🤔
🤔
On exam:
🩺You note bilateral inspiratory crackles at the 🫁 bases, although he's breathing comfortably on room air
💪Musculoskeletal exam reveals no synovitis
🦾Manual muscle strength exam is 5/5 throughout all major muscle groups
Which laboratory test do you order next? 🧐
🩺You note bilateral inspiratory crackles at the 🫁 bases, although he's breathing comfortably on room air
💪Musculoskeletal exam reveals no synovitis
🦾Manual muscle strength exam is 5/5 throughout all major muscle groups
Which laboratory test do you order next? 🧐
Inflammatory myopathies:
◾️Aka idiopathic inflammatory myopathies (IIM); can present with a variety of symptoms & most commonly *symmetric proximal muscle weakness*
◽️Other signs include: heliotrope rash 👀, Gottron’s papules (see image), interstitial lung disease, dysphagia
◾️Aka idiopathic inflammatory myopathies (IIM); can present with a variety of symptoms & most commonly *symmetric proximal muscle weakness*
◽️Other signs include: heliotrope rash 👀, Gottron’s papules (see image), interstitial lung disease, dysphagia

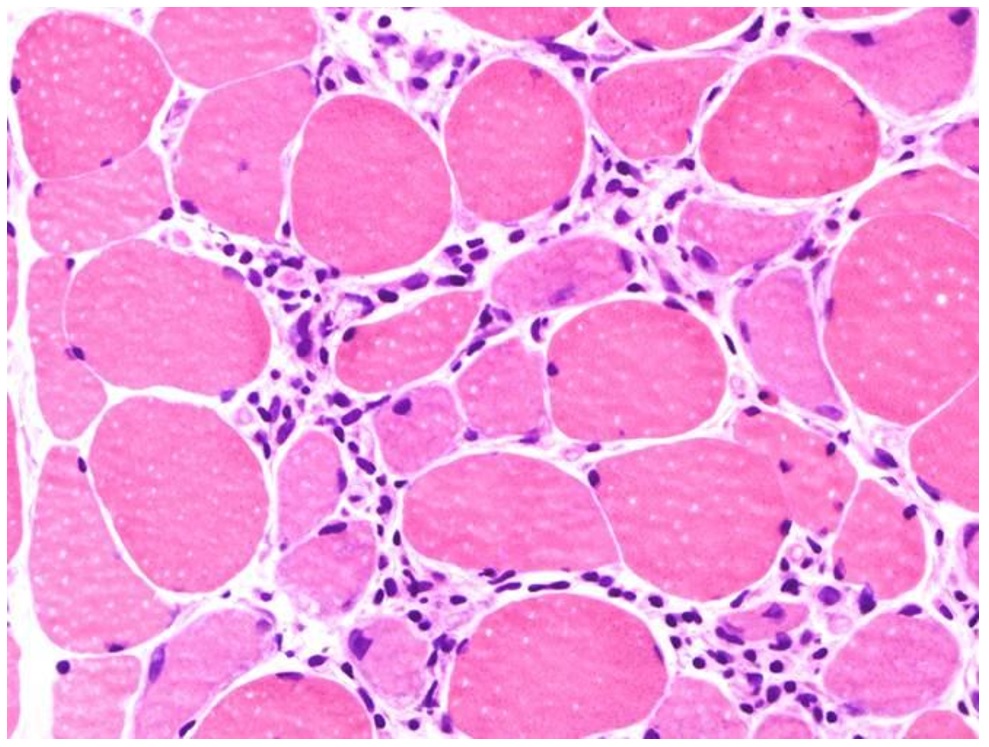
IIM mechanism?
Lymphocytic infiltrates in muscle tissue and expression of autoantibodies against muscle are part of the immune mechanisms contributing to myositis!
T- and B-cell proliferation and activation can be seen on muscle biopsy
👇👇👇
Lymphocytic infiltrates in muscle tissue and expression of autoantibodies against muscle are part of the immune mechanisms contributing to myositis!
T- and B-cell proliferation and activation can be seen on muscle biopsy
👇👇👇
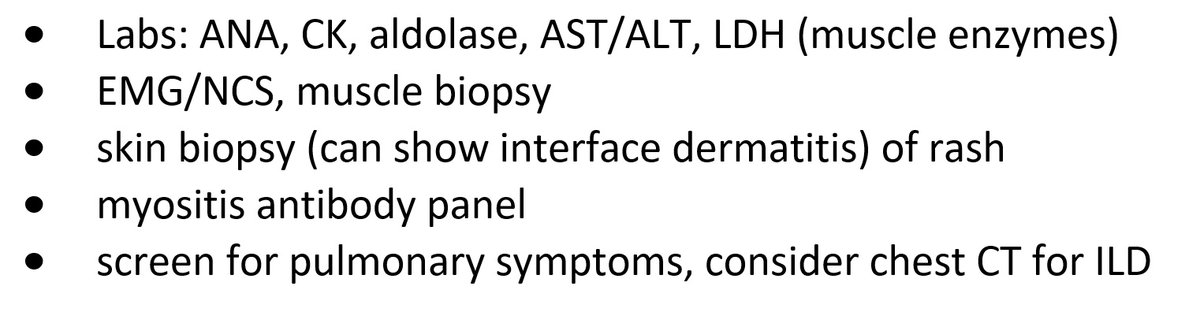
After a comprehensive physical exam, here is some of the diagnostic workup that should be considered if you have a patient and are concerned for myositis:
💪🧪🫁
💪🧪🫁
Laboratory workup reveals:
+ANA 1:160 (homogenous)
Normal CK & aldolase
You suspect this patient has MDA-5 Dermatomyositis (DM), an idiopathic inflammatory myopathy (aka myositis)
MDA-5 DM can be clinically amyopathic w/ rapidly progressive interstitial lung disease (ILD) 💪🫁
+ANA 1:160 (homogenous)
Normal CK & aldolase
You suspect this patient has MDA-5 Dermatomyositis (DM), an idiopathic inflammatory myopathy (aka myositis)
MDA-5 DM can be clinically amyopathic w/ rapidly progressive interstitial lung disease (ILD) 💪🫁

Clinical features in MDA-5 DM include:
🔸Cutaneous ulcers
🔹Oral ulcers
💇Alopecia
🫁Pulmonary symptoms 2/2 ILD
MDA-5 myositis can be clinically amyopathic!
❗️this means that pts may *not* have muscle weakness on exam & can have normal muscle enzymes (CK, AST, ALT, aldolase)
🔸Cutaneous ulcers
🔹Oral ulcers
💇Alopecia
🫁Pulmonary symptoms 2/2 ILD
MDA-5 myositis can be clinically amyopathic!
❗️this means that pts may *not* have muscle weakness on exam & can have normal muscle enzymes (CK, AST, ALT, aldolase)

🆕 - skin biopsy now shows interface dermatitis
🩺 because of *new* dyspnea on exertion 🏃, you evaluate the patient and admit for further workup
Which laboratory marker should be checked to determine prognosis?
🩺 because of *new* dyspnea on exertion 🏃, you evaluate the patient and admit for further workup
Which laboratory marker should be checked to determine prognosis?
🩸Ferritin level is an important prognostic marker for development of rapidly progressive ILD (RP-ILD) & mortality
From a 2012 study:
MDA-5 DM patients with RP-ILD had ⬆️ ferritin than those without ILD
MDA-5 DM patients who died also had ⬆️ ferritin than patients who lived
👇
From a 2012 study:
MDA-5 DM patients with RP-ILD had ⬆️ ferritin than those without ILD
MDA-5 DM patients who died also had ⬆️ ferritin than patients who lived
👇
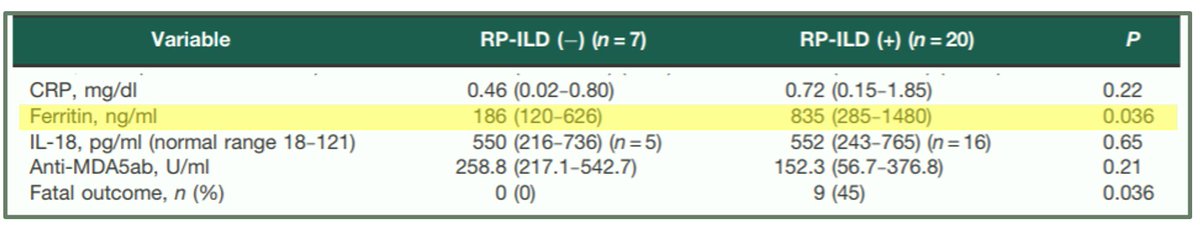
Notably, there was *no* difference in CRP levels between these two MDA-5 DM groups: w/ RP-ILD & w/o RP-ILD
🩸it's possible the hyperferritinemia is not simply a reflection of the acute phase response, but a true pathophysiological mechanism
🚨a viral trigger may be associated!
🩸it's possible the hyperferritinemia is not simply a reflection of the acute phase response, but a true pathophysiological mechanism
🚨a viral trigger may be associated!
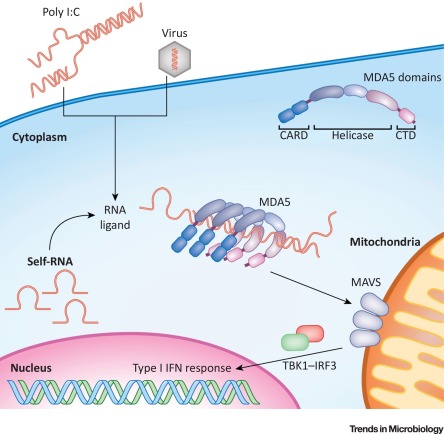
What is MDA-5?
🧬MDA5 is an interferon-induced RNA helicase which senses ssRNA viruses (e.g. SARS-CoV-2!)
🧐Some hypothesize MDA-5 DM as a form of macrophage activation syndrome - given high ferritin & IL-18 levels - that targets skin and lungs related to an infectious trigger
🧬MDA5 is an interferon-induced RNA helicase which senses ssRNA viruses (e.g. SARS-CoV-2!)
🧐Some hypothesize MDA-5 DM as a form of macrophage activation syndrome - given high ferritin & IL-18 levels - that targets skin and lungs related to an infectious trigger
CASE 2:
Suppose instead you have a patient with:
▪️Psoriatic-like lesions
▫️Hyperkeratotic papules on palmar & digital flexor surfaces
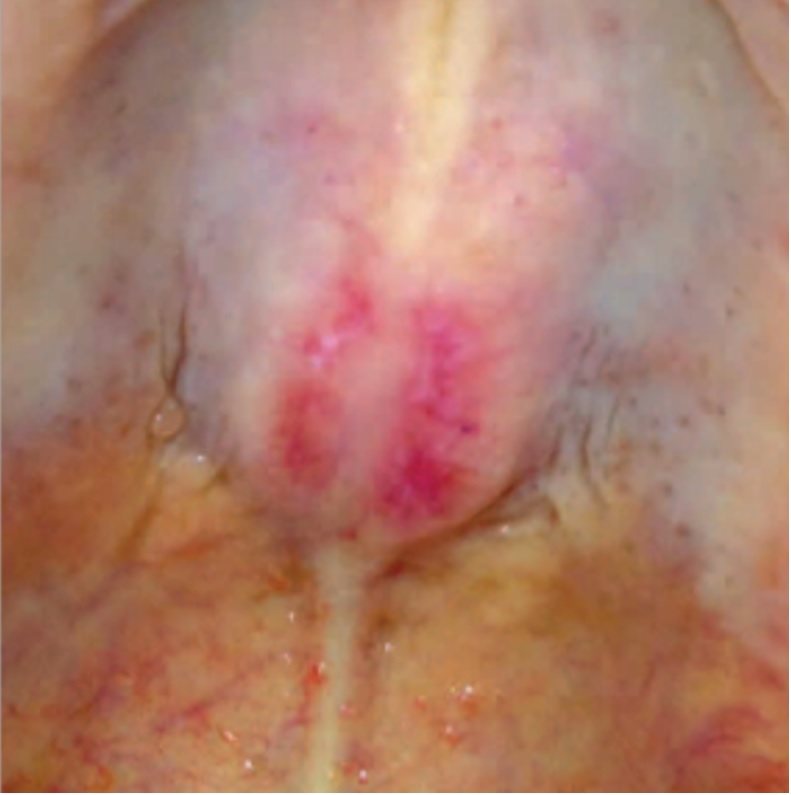
▪️This lesion 👇 on the roof of the mouth
Suppose instead you have a patient with:
▪️Psoriatic-like lesions
▫️Hyperkeratotic papules on palmar & digital flexor surfaces
▪️This lesion 👇 on the roof of the mouth
🧪Which myositis-specific antibody do you suspect will come back positive on the myositis antibody panel in this patient?🧪
🥁... this patient has TIF1y dermatomyositis
🔹TIF1y DM can cause psoriasis-like lesions & this finding of an ovoid palatal patch (symmetric curved erythema on hard palate w/ white macules)
🔸It's important to screen patients w/ DM for malignancy, especially if TIF1y positive!
🔹TIF1y DM can cause psoriasis-like lesions & this finding of an ovoid palatal patch (symmetric curved erythema on hard palate w/ white macules)
🔸It's important to screen patients w/ DM for malignancy, especially if TIF1y positive!
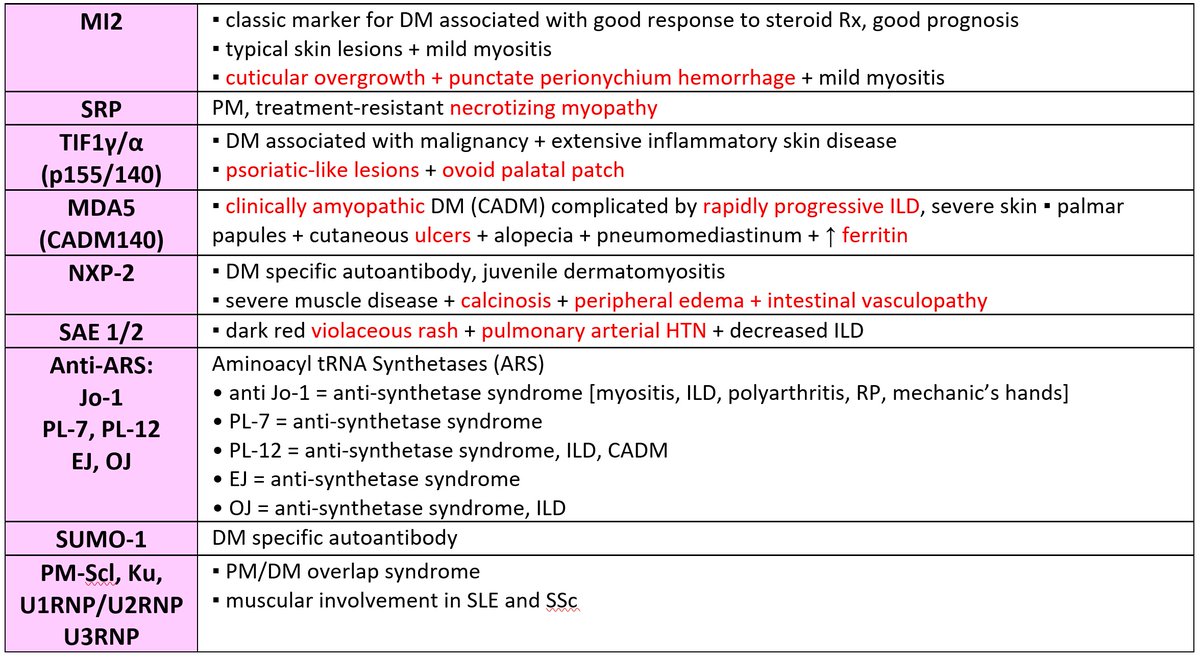
So... why do these antibodies matter, clinically?
🩺 recognizing specific phenotypes associated with myositis-specific antibodies (MSAs) can help identify the particular IIM subtype and its various systemic manifestations
More examples?
see ⬇️
🩺 recognizing specific phenotypes associated with myositis-specific antibodies (MSAs) can help identify the particular IIM subtype and its various systemic manifestations
More examples?
see ⬇️
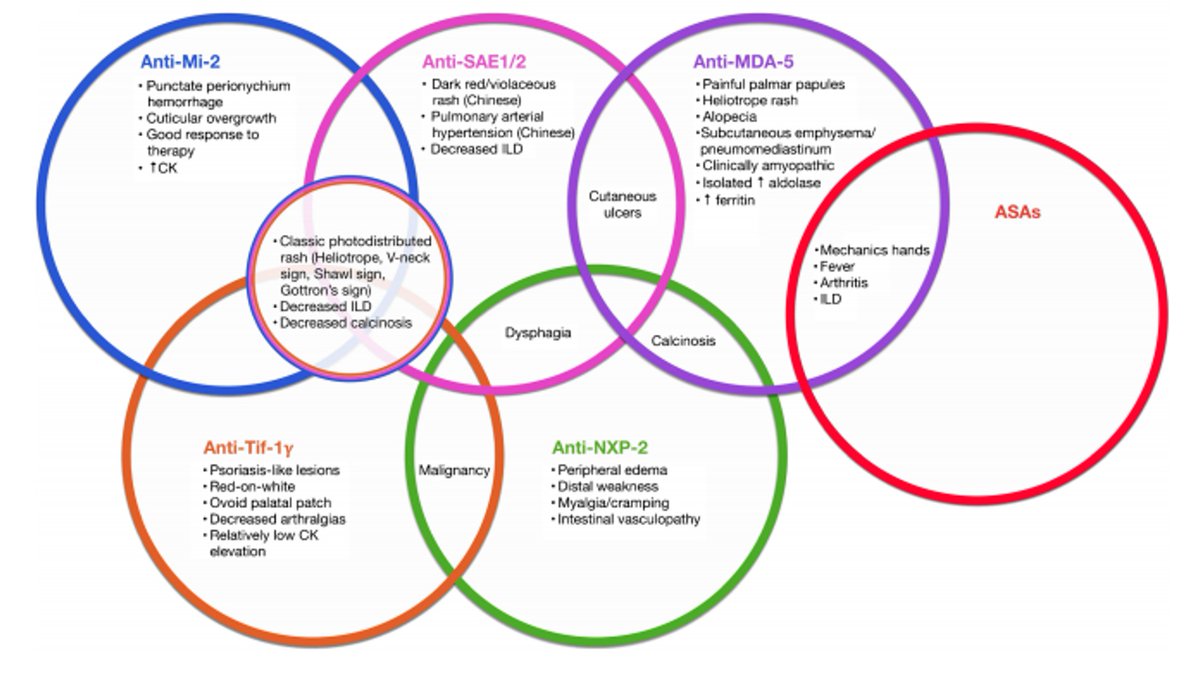
Here's a reference chart to keep the different types of myositis-specific antibodies (MSAs) organized!
✏️📚✏️
✏️📚✏️
Keep in mind that some autoantibodies are *non-specific*
While they can be detected in patients with myositis, they are also seen in other autoimmune disorders (e.g. Ro52 in scleroderma)!
🔍these are called myositis-associated antibodies (MAAs)🔍
MSAs vs MAAs:
While they can be detected in patients with myositis, they are also seen in other autoimmune disorders (e.g. Ro52 in scleroderma)!
🔍these are called myositis-associated antibodies (MAAs)🔍
MSAs vs MAAs:
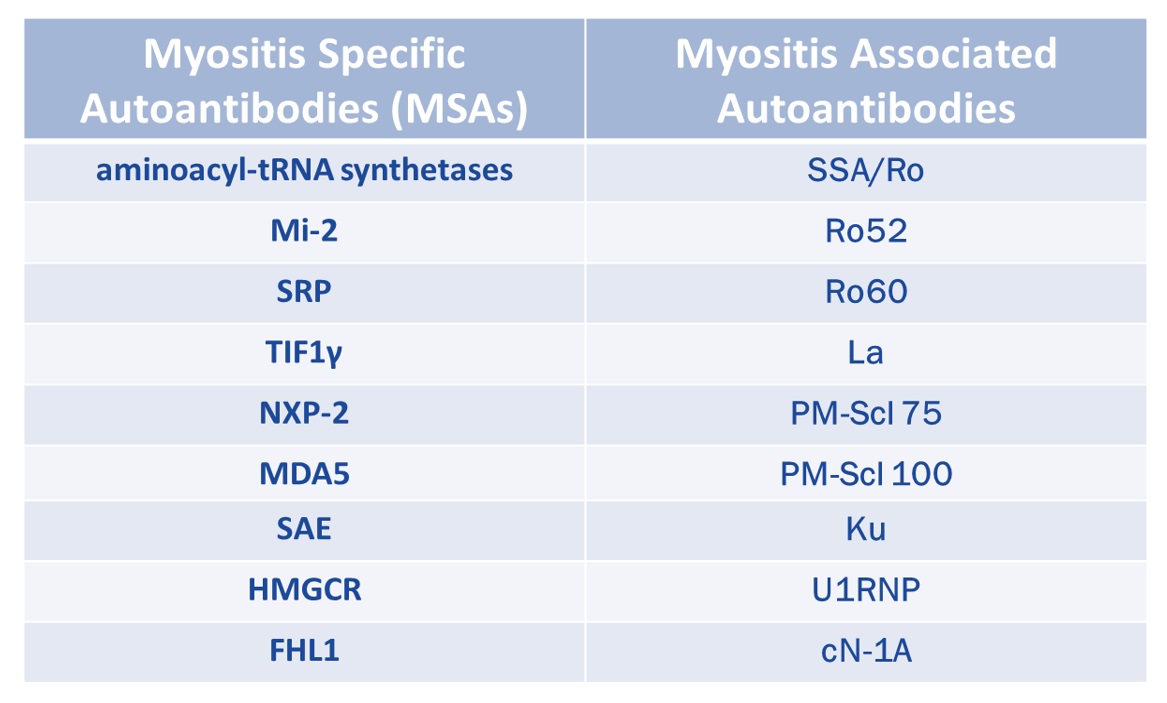
One can check the myositis antibody panel to see which of the MSAs are included at their institution
Of note: specific types of inflammatory myopathies – such as HMGCR necrotizing myopathy – are *not* included in the MyoMarker 3 panel (most commonly used myositis Ab panel)
Of note: specific types of inflammatory myopathies – such as HMGCR necrotizing myopathy – are *not* included in the MyoMarker 3 panel (most commonly used myositis Ab panel)
To learn more about the identification of myositis-specific antibodies (MSAs) and association with distinct clinical phenotypes, check out this article by myself and @LisaCriscione:
the-rheumatologist.org/article/myosit…
the-rheumatologist.org/article/myosit…
REFs (1/2):
(1) pubmed.ncbi.nlm.nih.gov/31365803/
(2) Gono et. al. Rheumatology (Oxford). 2012 Sep;51(9):1563-70.
(3) Gono et. al. Rheumatology (Oxford). 2010 Jul;49(7):1354-60.
(4) Fiorentino et. al. J Am Acad Dermatol. 2011 Jul;65(1):25-34.
(1) pubmed.ncbi.nlm.nih.gov/31365803/
(2) Gono et. al. Rheumatology (Oxford). 2012 Sep;51(9):1563-70.
(3) Gono et. al. Rheumatology (Oxford). 2010 Jul;49(7):1354-60.
(4) Fiorentino et. al. J Am Acad Dermatol. 2011 Jul;65(1):25-34.
REFs (2/2):
(5) Moghadam-Kia S et al. Curr Rheumatol Rep. 2018 Oct 31;20(12):78.
(6) Bernet et. al. JAMA Dermatol. 2016 Sep 1;152(9):1049-51.
(7) Wolstencroft PW & Fiorentino DF. Curr Rheumatol Rep. 2018 Apr 10;20(5):28.
(8) sciencedirect.com/science/articl…
(5) Moghadam-Kia S et al. Curr Rheumatol Rep. 2018 Oct 31;20(12):78.
(6) Bernet et. al. JAMA Dermatol. 2016 Sep 1;152(9):1049-51.
(7) Wolstencroft PW & Fiorentino DF. Curr Rheumatol Rep. 2018 Apr 10;20(5):28.
(8) sciencedirect.com/science/articl…
@DavidLeverenz @LisaCriscione @TheMyositisAssc @MyositisSupport @UKMyositis @didemsayginmd @docrota @drhectorchinoy @pekor002 @DrJohanLim @k_vaishnani @AnnKumfer @medrants
• • •
Missing some Tweet in this thread? You can try to
force a refresh