Final presentation for Day 2 of Design Research 2021
Paul Merrel, Rebecca Hendry, Sean Rom and Peta Marks
— The one-two punch: Context and co-design
#dr2021
Paul Merrel, Rebecca Hendry, Sean Rom and Peta Marks
— The one-two punch: Context and co-design
#dr2021
Content Warning: Eating Disorders
People with eating disorders often present with at least one addition mental illness. Around 22% access support for their easting disorder and only a small amount receive evidence based care.
The majority of people with eating disorders are not being identified or given the best possible treatment for their illness.
Early intervention is incredibly important, but people go 30 years without identification, even when regularly visiting their primary care practitioner for co-morbid health concerns and conditions.
The clinical digital support tool is focussed on getting new evidence to practitioners quickly to improve health outcomes for patients
It takes on average 17 years for a research innovation to make it into practice.
It takes on average 17 years for a research innovation to make it into practice.
There's a number of complex issues when trying to create better outcomes for people experiencing an eating disorder
Health systems
Practice issues
Workforce issues
Stigma and stereotyping
Individual factors
Health systems
Practice issues
Workforce issues
Stigma and stereotyping
Individual factors
Many people get directed to non-evidence based treatments for eating disorders.
People speak to their GP's the most about mental health issues, but they're unable to be aware of everything.
People speak to their GP's the most about mental health issues, but they're unable to be aware of everything.
Bec is now going to discuss how the research was conducted.
The bulk of the research was completed remotely.
It gave them access to a breadth of geographic locations, metro, regional and rural.
It meant they got a great breadth of context from GP's as well
The bulk of the research was completed remotely.
It gave them access to a breadth of geographic locations, metro, regional and rural.
It meant they got a great breadth of context from GP's as well
Spoke to people with lived experience and their families in remote areas where it's difficult to get treatment
A feature of the approach is to humanise the work that we're doing — the language used in research is really important, and in the culture of healthcare it can be easy to use 'patient' but where ever possible they used language with the purpose of avoiding disempowering terms
The reimbursed the GP's and people with lived experience at the same rate — important for balancing power.
They're sharing art work from autoethnography people shared before coming into interviews so it was easier for them to articulate their experience
They needed a way to understand the missing context of being in the room with a GP, being in thier consulting room. So the team masked up and did 'Tech Tours' to see how patient interactions happened, the tech uses, how they would show it, where they gave them information
The detail and nuance from these sessions were integral for the design and adoption. It needed to fit in with how they worked.
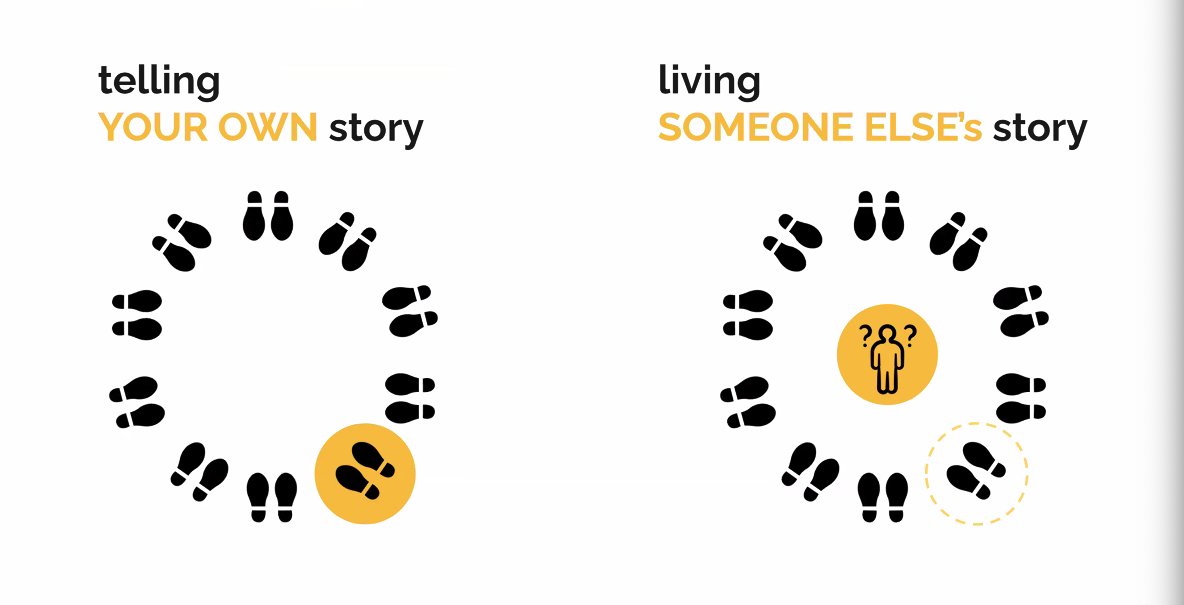
Often peoples mental model is that cognition happens inside an individual.
What actually happens is that cognition is distributed among actors and context in which the interaction takes place.
The tool being the DAAS21 form that the GP and person work through together
What actually happens is that cognition is distributed among actors and context in which the interaction takes place.
The tool being the DAAS21 form that the GP and person work through together
After prototyping in person, they ran remote prototyping sessions.
They went back to people they interviewed to show them what their input created, and they gave even better feedback seeing the prototype created
They went back to people they interviewed to show them what their input created, and they gave even better feedback seeing the prototype created
What they learned.
How can health use co-design and context to speed up change and make a positive impact on people's lives?
Dan Hill's pace layers — it's important to move slow enough to keep people safe, and fast enough to help people.
How can health use co-design and context to speed up change and make a positive impact on people's lives?
Dan Hill's pace layers — it's important to move slow enough to keep people safe, and fast enough to help people.
A lot of research isn't funded all the way through to translation and implementation — lots of hoops — co-design increases the likelihood an intervention will be acceptable to the people it's purporting to help and de-risks when we get to the translation stage,
Everything that we can do to reduce the risk of translation will speed up the entire process.
It also helps to make decisions about what to move forward with.
It also helps to make decisions about what to move forward with.
How can we avoid co-creation theatre?
It's important for us to consider how we focus on doing the actual work more so than talking about doing the work.
People can THINK they're doing it but might not be able to do it well.
It's important for us to consider how we focus on doing the actual work more so than talking about doing the work.
People can THINK they're doing it but might not be able to do it well.
Doing it well makes it quite a bit of investment, money, time and everyone involved.
They looked at different models but they really wanted to spend time on individual conversations and map out the themes that came from them
They looked at different models but they really wanted to spend time on individual conversations and map out the themes that came from them
In mental health the ethos of "nothing about us without us" needs to extend across the entire process of health, and to make sure that this is not just a slogan.
You must consult and be lead by people at as many points of the process as possible
You must consult and be lead by people at as many points of the process as possible
They could improve their processes by consulting at more points in the process, including having GP's and other people presenting their findings together.
What can we do differently to continue co-design?
InsideOut took the report and the recommendation and the practice manager looked at the practice workflows to identify where we could make change in that system to support GP's
InsideOut took the report and the recommendation and the practice manager looked at the practice workflows to identify where we could make change in that system to support GP's
They needed to include what to spend or not spend on.
The meld prototypes at the end of the additional scrutiny held up.
The meld prototypes at the end of the additional scrutiny held up.
If they knew what then what they knew now they would have extended the research to include all of the processes the go in to making the GP and patient relationship work.
That way they could have moved to building quicker.
That way they could have moved to building quicker.
@threadreaderapp unroll please
• • •
Missing some Tweet in this thread? You can try to
force a refresh