
Study of 25,661 UK healthcare workers (including 8,278 with past COVID-19), showing past infection offers 84% protection against reinfection (93% for symptomatic disease) over 1-7 months. The emergence of the UK variant didn’t make reinfection more likely.
thelancet.com/journals/lance…
thelancet.com/journals/lance…
During the study, participants had a PCR test every 2 weeks, and an antibody test every 4 weeks, so we can be reasonably sure the majority of cases would have been detected.
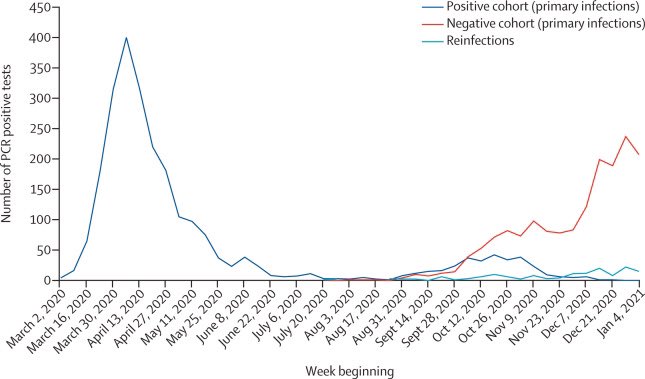
There were 1,704 infections in people who hadn’t previously had COVID-19 (of which 17% were asymptomatic), and 2 probable and 153 possible reinfections (1.9%), of which 49% were asymptomatic.
The researchers were generally unable to perform genomic sequencing, and as such could not confirm the reinfections were genuine. Some probably reflect persistent viral shedding. This means their estimate of protection (84%) is probably an underestimate.
Healthcare workers are also a high-risk population, and may be exposed to the virus more often and in higher amounts. The rate of reinfection may therefore be lower in the general population.
However, the participants in this study were generally young (median age: 46 years; range: 18-84 years; IQR: 35-54 years). Older people (whose immune response may be less effective) might be less well protected.
In summary most people who’ve had COVID-19 are probably protected from reinfection over the short to medium term. However, vaccination remains the best way to protect yourself.
Those who’ve had COVID-19 should also get vaccinated to ensure they’re protected as much as possible.
Those who’ve had COVID-19 should also get vaccinated to ensure they’re protected as much as possible.
• • •
Missing some Tweet in this thread? You can try to
force a refresh






