So, remember C3,4,5 keeps you alive?!
Yes, today’s Tweetorial from @icmteaching, @ICUltrasonica and myself is all about the diaphragm!
It’s a pretty vital muscle, and a muscle often forgotten. It’s no wonder why, when it’s weak, your patients won’t liberate from the ventilator!
Yes, today’s Tweetorial from @icmteaching, @ICUltrasonica and myself is all about the diaphragm!
It’s a pretty vital muscle, and a muscle often forgotten. It’s no wonder why, when it’s weak, your patients won’t liberate from the ventilator!

So, does #POCUS have a role in assessing it. Of course it does!🤷♂️😂
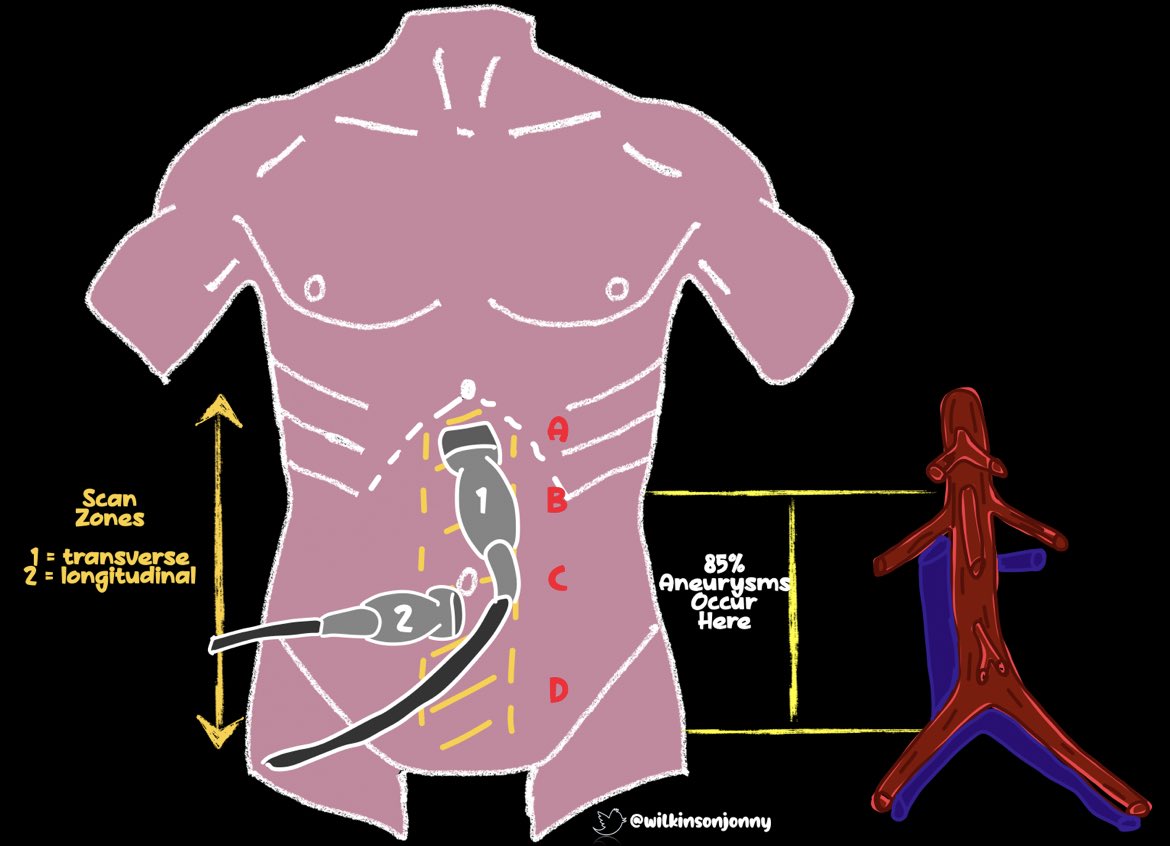
We use 3 probe positions:
1) Mid axillary/RUQ point - marker 12 O’clock
2) Mid clavicular/Subcostal - marker 12 O’clock
3) Mid clavicular/subcostal - marker 3 O’clock
We use 3 probe positions:
1) Mid axillary/RUQ point - marker 12 O’clock
2) Mid clavicular/Subcostal - marker 12 O’clock
3) Mid clavicular/subcostal - marker 3 O’clock
Here’s MidAx/RUQ position:
The lung curtain does get in the way here, so run M-mode low down to catch the diaphragm.
We use the vital organ (liver or spleen) as our scan window and discriminator between chest cavity and abdominal cavity👍
The lung curtain does get in the way here, so run M-mode low down to catch the diaphragm.
We use the vital organ (liver or spleen) as our scan window and discriminator between chest cavity and abdominal cavity👍
Speaking of M-mode, it is sensitive for movement / gaging distance. So after you get the B-mode view, run it through the diaphragm👍
⭐️ We can measure the diaphragm’s EXCURSION.
>1cm indicates good spontaneous effort and should mean ‘weanability’, from the ventilator.
⭐️ We can measure the diaphragm’s EXCURSION.
>1cm indicates good spontaneous effort and should mean ‘weanability’, from the ventilator.
Next, position 2:
Place the probe mid clav/SC/marker to 12 O’clock.
Here, we see the muscle bulk to the diaphragm and can appreciate its layers + thickening.
Inspiration -> it thickens
Expiration -> it thins
⭐️ This is diaphragm thickening index or Tdi:
Thin/thick x 100
Place the probe mid clav/SC/marker to 12 O’clock.
Here, we see the muscle bulk to the diaphragm and can appreciate its layers + thickening.
Inspiration -> it thickens
Expiration -> it thins
⭐️ This is diaphragm thickening index or Tdi:
Thin/thick x 100
Run your m-mode through now, we can really appreciate this.
Here we see this respiratory muscle thicken on a spont breath in and thin down on passive recoil expiration.
Tdi >30% = no sonographic diaphragmatic dysfunction. It is 71% specific for extubation success 👏
Here we see this respiratory muscle thicken on a spont breath in and thin down on passive recoil expiration.
Tdi >30% = no sonographic diaphragmatic dysfunction. It is 71% specific for extubation success 👏
Finally, position 3:
Probe mid ax/SC /marker to 9 O’clock.
Just another view and not a million miles from a cardiac subcostal. We can see the heart, part of the IVC and there’s minimal lung curtain interference.
Probe mid ax/SC /marker to 9 O’clock.
Just another view and not a million miles from a cardiac subcostal. We can see the heart, part of the IVC and there’s minimal lung curtain interference.
Yup, run that M-mode through to appreciate movement and measure it again.
Happy probing!
#FOAMed #FOAMcc #foamus #echofirst #foamem
Happy probing!
#FOAMed #FOAMcc #foamus #echofirst #foamem
The evidence to support its usage.
There isn’t heaps of outcome data, but assessment to note extreme wasting, poor excursion and poor Tdi certainly predict success or failure of SBT and liberation from the vent!
pubmed.ncbi.nlm.nih.gov/29435329/
There isn’t heaps of outcome data, but assessment to note extreme wasting, poor excursion and poor Tdi certainly predict success or failure of SBT and liberation from the vent!
pubmed.ncbi.nlm.nih.gov/29435329/
Download the full graphic here
criticalcarenorthampton.com/pocusgrams/
Tagging @PARADicmSHIFT @r_wiersema @sonophysio @SimonOrlob @iceman_ex @ThinkingCC @amit_pawa @Manoj_Wickram @dr_rajgupta @load_dependent @khaycock2 @zedunow @POCUSAcademy @IMPOCUSFocus @POCUSClub @kyliebaker888
criticalcarenorthampton.com/pocusgrams/
Tagging @PARADicmSHIFT @r_wiersema @sonophysio @SimonOrlob @iceman_ex @ThinkingCC @amit_pawa @Manoj_Wickram @dr_rajgupta @load_dependent @khaycock2 @zedunow @POCUSAcademy @IMPOCUSFocus @POCUSClub @kyliebaker888

Tagging @PracticalPOCUS @POCUSEcho @pocuseducation @POCUS_Society @TaotePOCUS @Pocus101 @hepocus @POCUSJournal @NephroP @pocusfoamed @POCUSbot @drzaf_pic @Nadia_Hdz_MD @shaskinsMD @elboghdadly @UltrasoundMD @NixLimerick @cianmcdermott @bhca @MJGriksaitis @rosie_hogg
• • •
Missing some Tweet in this thread? You can try to
force a refresh