1/
WHY is there a BABOON in my room?
A #tweetorial about the outcomes of hepatic coma, how far we have come, and how wild things got along the way
#livertwitter
WHY is there a BABOON in my room?
A #tweetorial about the outcomes of hepatic coma, how far we have come, and how wild things got along the way
#livertwitter
2/
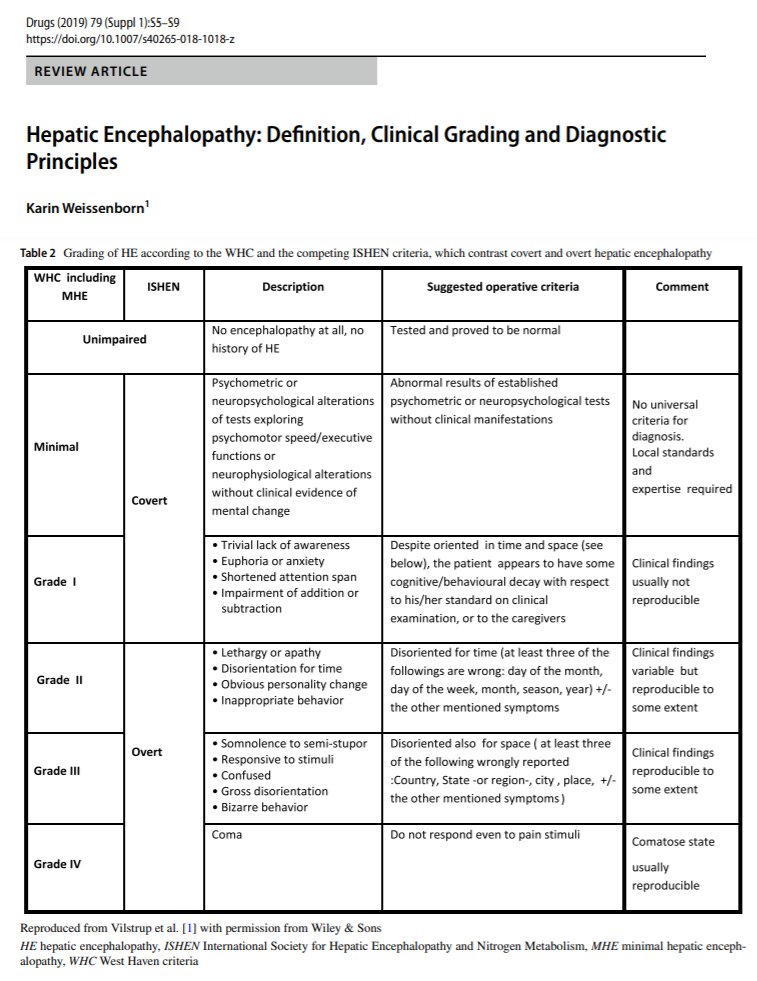
Up first: the lingo
Hepatic encephalopathy (HE) presents as a spectrum with subtle cognitive/motor deficits at one end (AKA "Covert HE") and coma at the other
HE/Coma can be caused by #cirrhosis (Type C, more common) and acute liver failure (Type A)

Up first: the lingo
Hepatic encephalopathy (HE) presents as a spectrum with subtle cognitive/motor deficits at one end (AKA "Covert HE") and coma at the other
HE/Coma can be caused by #cirrhosis (Type C, more common) and acute liver failure (Type A)

3/
What used to (1950s/60s) happen to patients with coma due to hepatic encephalopathy ("HE coma")?
1⃣Gabuzda said everyone died
2⃣Sherlock said it was 68% mortality, Stormont 63%
3⃣Prytz said it was 80% mortality at 6-months


What used to (1950s/60s) happen to patients with coma due to hepatic encephalopathy ("HE coma")?
1⃣Gabuzda said everyone died
2⃣Sherlock said it was 68% mortality, Stormont 63%
3⃣Prytz said it was 80% mortality at 6-months



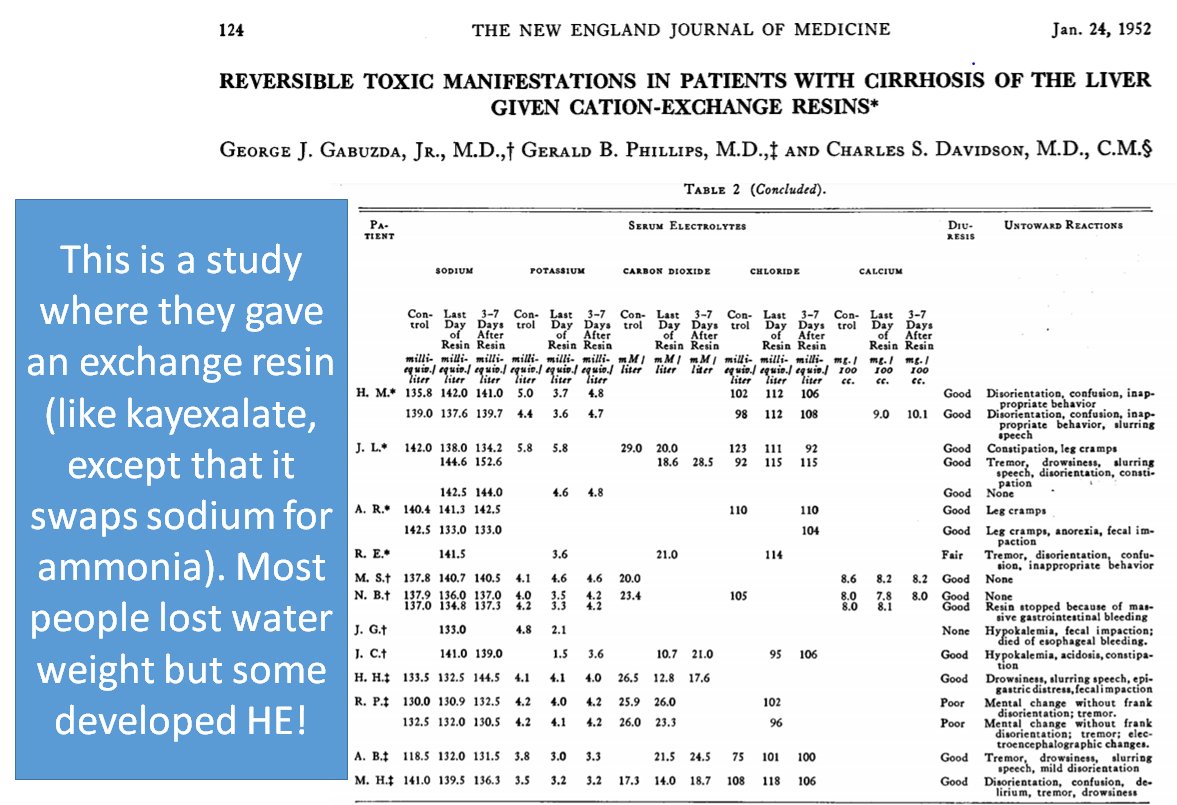
4/
HE coma was hopeless
And then, 1952-54, the big bang moment
We discovered ammonia as a trigger
While ammonia was n̳e̳v̳e̳r̳ thought to be the whole story, it was directly linked to HE and was a modifiable target

HE coma was hopeless
And then, 1952-54, the big bang moment
We discovered ammonia as a trigger
While ammonia was n̳e̳v̳e̳r̳ thought to be the whole story, it was directly linked to HE and was a modifiable target

5/
Ammonia comes from the gut.
You know what reduces ammonia?
Antibiotics!
Maybe by changing bacterial or gut metabolism, maybe by changing the bacteria themselves
In 1955, Silen showed that neomycin ⬇️⬇️ammonia levels.
Ammonia comes from the gut.
You know what reduces ammonia?
Antibiotics!
Maybe by changing bacterial or gut metabolism, maybe by changing the bacteria themselves
In 1955, Silen showed that neomycin ⬇️⬇️ammonia levels.

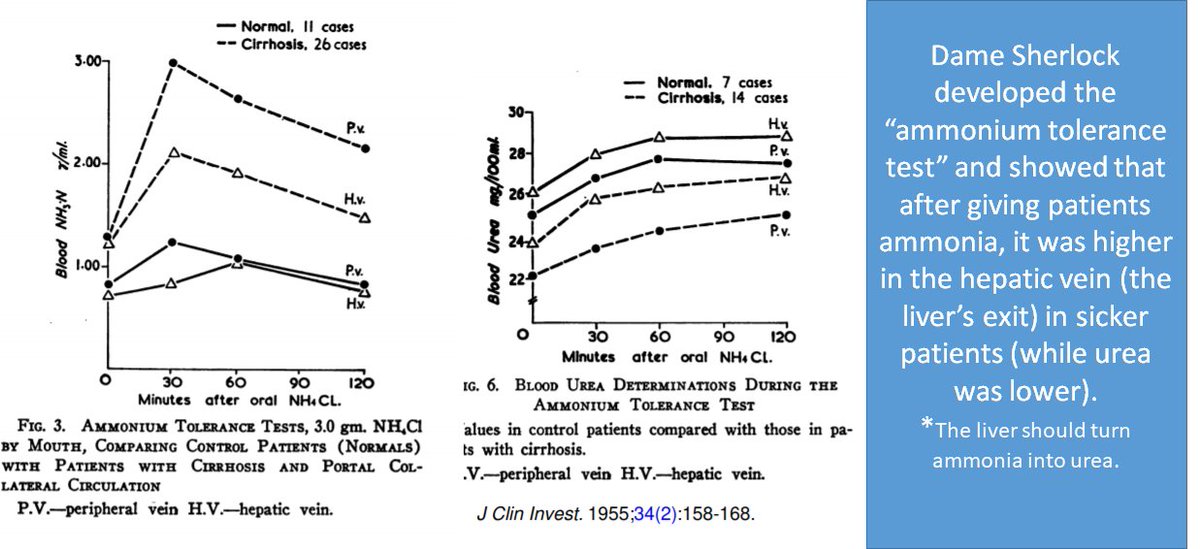
7/
We also learned that the liver efficiently clears ammonia from the blood but not so much in #cirrhosis
Check out the "Ammonium Tolerance Test"
We also learned that the liver efficiently clears ammonia from the blood but not so much in #cirrhosis
Check out the "Ammonium Tolerance Test"
8/
💡Can we treat HE by cleaning the blood with healthy liver?
Step One:
In 1958, Otto created "Eck fistulas" (connect the SMV-IVC) in dogs.
He then hooked another dog liver up to a circuit with the femoral artery and vein.
It cleared the ammonia.

💡Can we treat HE by cleaning the blood with healthy liver?
Step One:
In 1958, Otto created "Eck fistulas" (connect the SMV-IVC) in dogs.
He then hooked another dog liver up to a circuit with the femoral artery and vein.
It cleared the ammonia.


9/
Step two:
In 1961, Eiseman showed you could run blood through a liver removed from a recently deceased person. "Ex vivo" perfusion
It cleared the ammonia
Step two:
In 1961, Eiseman showed you could run blood through a liver removed from a recently deceased person. "Ex vivo" perfusion
It cleared the ammonia

10/
Step 3: Use it to treat hepatic coma
In 1965, an upstart surgeon named Starzl sewed a liver to the groin of comatose kids
In 1966, Sen reported 'ex vivo' perfusion of human livers hooked up to people in coma from acute liver failure or #cirrhosis
It rarely worked

Step 3: Use it to treat hepatic coma
In 1965, an upstart surgeon named Starzl sewed a liver to the groin of comatose kids
In 1966, Sen reported 'ex vivo' perfusion of human livers hooked up to people in coma from acute liver failure or #cirrhosis
It rarely worked


11/
💡Do we really need to take the donor liver out of the body??
In 1965, Burnell teamed up with Scribner to do “dialysis” by cross-circulating the blood of a woman in hepatic coma into a man dying of cancer.
She woke up! (though she later died from GI bleeding)

💡Do we really need to take the donor liver out of the body??
In 1965, Burnell teamed up with Scribner to do “dialysis” by cross-circulating the blood of a woman in hepatic coma into a man dying of cancer.
She woke up! (though she later died from GI bleeding)


12/
Despite poor outcomes, people were excited
But it was just not feasible to:
1⃣find people willing to be human dialysis machines
2⃣find suitable donors for ex-vivo liver perfusion
Two alternatives were considered
Despite poor outcomes, people were excited
But it was just not feasible to:
1⃣find people willing to be human dialysis machines
2⃣find suitable donors for ex-vivo liver perfusion
Two alternatives were considered
13/
First, people like Charlie Trey tried exchange transfusions.
Basically, replacing the blood with donor blood products.
It was mainly tried for acute viral hepatitis or halothane hepatitis.
Seemed promising.
But controlled trials failed.


First, people like Charlie Trey tried exchange transfusions.
Basically, replacing the blood with donor blood products.
It was mainly tried for acute viral hepatitis or halothane hepatitis.
Seemed promising.
But controlled trials failed.



14/
Second, many thought it would be easier to use animal livers
In 1965, Eiseman hooked up a pig liver to 8 patients with #cirrhosis in coma.
All patients died within 8 days.
But many woke up, including one man who requested a cigarette while still in the OR

Second, many thought it would be easier to use animal livers
In 1965, Eiseman hooked up a pig liver to 8 patients with #cirrhosis in coma.
All patients died within 8 days.
But many woke up, including one man who requested a cigarette while still in the OR


15/
The concept of cross-circulation - liver dialysis using a living being - again took hold
In 1968, Christian Barnard published twin papers in @TheLancet describing how to do it with a baboon and the outcome in one young woman with #cirrhosis
She left the hospital

The concept of cross-circulation - liver dialysis using a living being - again took hold
In 1968, Christian Barnard published twin papers in @TheLancet describing how to do it with a baboon and the outcome in one young woman with #cirrhosis
She left the hospital


16/
Which brings me to Hume's 1969 description:
He brought an awake baboon to the bedside, immobilized him in a cast, flushed his blood out and replaced it with human blood, and then hooked him up to a patient in hepatic coma who would awake to find a baboon in the room.

Which brings me to Hume's 1969 description:
He brought an awake baboon to the bedside, immobilized him in a cast, flushed his blood out and replaced it with human blood, and then hooked him up to a patient in hepatic coma who would awake to find a baboon in the room.


17/
By the mid 1970's, animal-man cross-circulation was on the out
1⃣It was HARD
2⃣often ineffective
3⃣...complicated
4⃣👇And Starzl started getting good at liver transplantation
By the mid 1970's, animal-man cross-circulation was on the out
1⃣It was HARD
2⃣often ineffective
3⃣...complicated
4⃣👇And Starzl started getting good at liver transplantation
https://twitter.com/ebtapper/status/1376886696726437891?s=20
18/
Above all, we got good at treating HE
⭐️HE is a biomarker of badness
⭐️People with HE died of sepsis, bleeding, not HE!
⭐️We learned to treat the badness
Bam! our patients started surviving
Game changers
1⃣Endoscopy/banding
2⃣Good antibiotics
3⃣ICU care
4⃣Lactulose!
Above all, we got good at treating HE
⭐️HE is a biomarker of badness
⭐️People with HE died of sepsis, bleeding, not HE!
⭐️We learned to treat the badness
Bam! our patients started surviving
Game changers
1⃣Endoscopy/banding
2⃣Good antibiotics
3⃣ICU care
4⃣Lactulose!

19/
Proof of progress: Remember how basically everyone in HE coma due to #cirrhosis used to die in the hospital?
1⃣By the 1970's, 49% died
2⃣By the 2000's, 30% died by 1-year

Proof of progress: Remember how basically everyone in HE coma due to #cirrhosis used to die in the hospital?
1⃣By the 1970's, 49% died
2⃣By the 2000's, 30% died by 1-year


20/
Liver support (eg MARS) have been trialed, rarely improving HE in #cirrhosis
They havent ⬆️survival
But HE in acute liver failure is different
Patients still die waiting for transplant, keeping the liver support dream alive
See: pig perfusion redux, auxiliary tx

Liver support (eg MARS) have been trialed, rarely improving HE in #cirrhosis
They havent ⬆️survival
But HE in acute liver failure is different
Patients still die waiting for transplant, keeping the liver support dream alive
See: pig perfusion redux, auxiliary tx


/Summary
☑️People with HE coma die because of the triggers: bleeding, infection.
☑️⬆️survival for coma due to HE is mostly a triumph for supportive care
☑️Patients in coma inspired us to try wild things, and ultimately led us to learn how to transplant
☑️People with HE coma die because of the triggers: bleeding, infection.
☑️⬆️survival for coma due to HE is mostly a triumph for supportive care
☑️Patients in coma inspired us to try wild things, and ultimately led us to learn how to transplant
end/
This concludes a #tweetorial on the history of outcomes and management of hepatic encephalopathy coma. Thank you for reading. I hope you enjoyed.
Thank you to @BloomPringle for reviewing and @HPB_Txp_Surg for the story (with @PeterAttiaMD) that inspired this
This concludes a #tweetorial on the history of outcomes and management of hepatic encephalopathy coma. Thank you for reading. I hope you enjoyed.
Thank you to @BloomPringle for reviewing and @HPB_Txp_Surg for the story (with @PeterAttiaMD) that inspired this
• • •
Missing some Tweet in this thread? You can try to
force a refresh