Body Politic has published an important open letter to the @NIH @NIHDirector urging the prioritization of #LongCOVID research that builds off prior research into #MECFS and related conditions.
👉 wearebodypolitic.com/bodytype/2021/… by @itsbodypolitic @fi_lowenstein @ItsAngInLA
👉 wearebodypolitic.com/bodytype/2021/… by @itsbodypolitic @fi_lowenstein @ItsAngInLA

In December, Congress provided $1.15 billion over 4 years for @NIH to “support research into the prolonged health consequences of #COVID19”. With many newcomers to the field there’s cause for concern that experienced #MECFS researchers may be overlooked. nih.gov/about-nih/who-… 
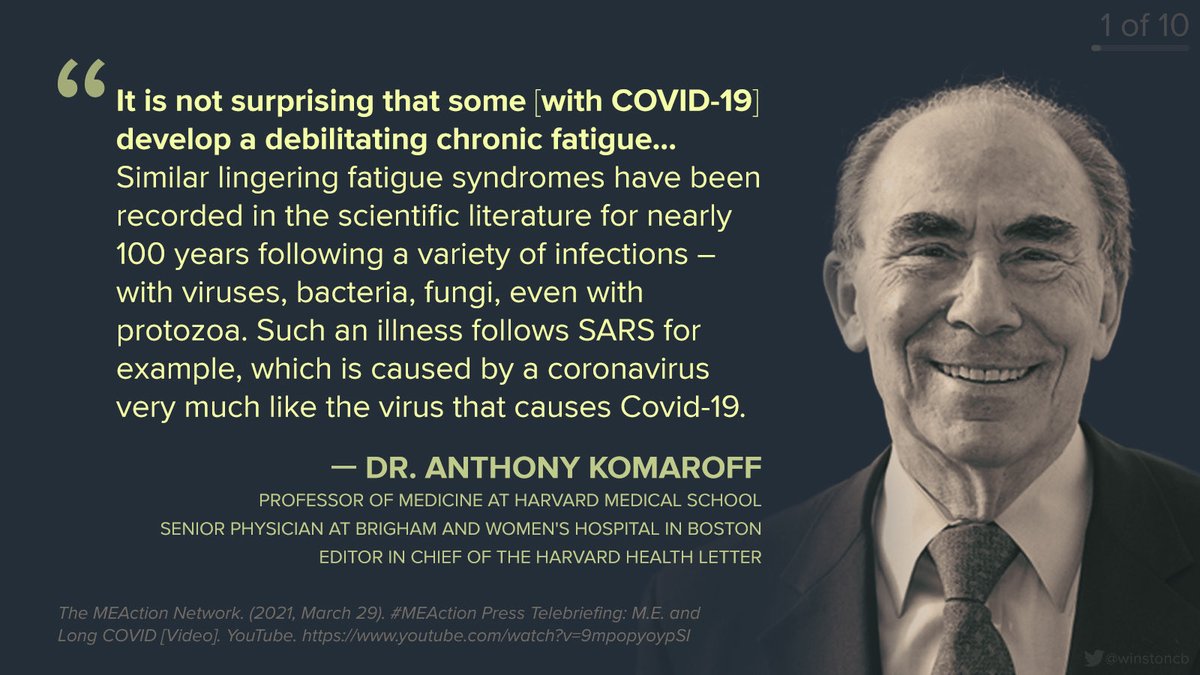
#LongCovid and #MECFS have much in common and are increasingly joining forces to drive change that might lead to diagnostics, treatments, and a cure. 

Many #LongCOVID #longhaulers meet diagnostic criteria for #MECFS and related disorders like #dysautonomia #MCAS and #POTS. 

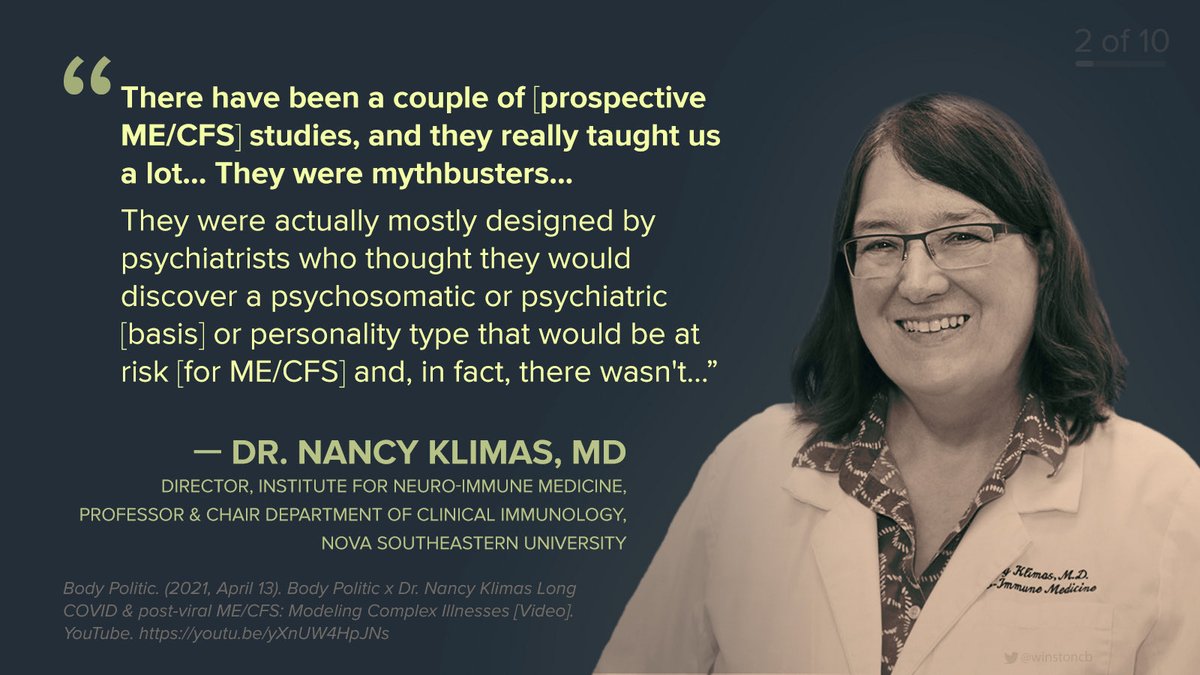
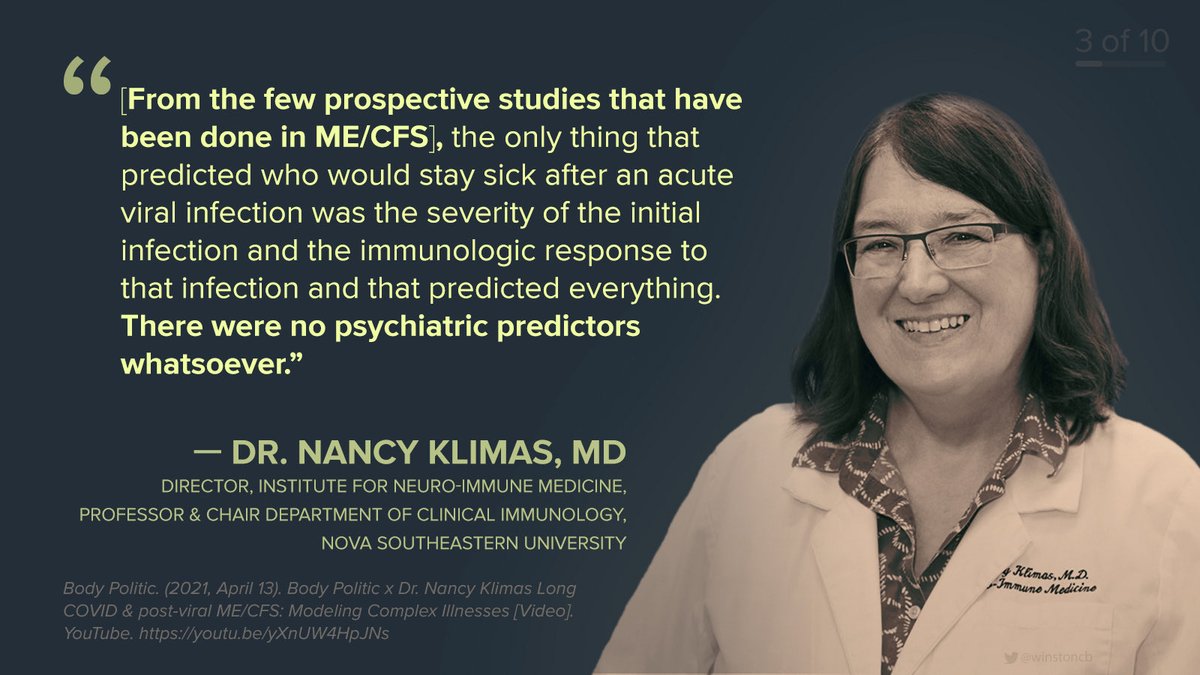
As much as we lament lack of funding that has substantially delayed scientific progress in #MECFS, as Dr. Klimas @ngklimas put it, “but by God we've been doing it anyway and there's just a lot of work [to build off of]” over recent decades that may be applicable to #LongCOVID. 

We’re used to hearing the framing that #MECFS “remains a mystery”, but in fact much has already been discovered thanks to intrepid researchers and patient-funded research. There are many hot leads to pursue. !["[ME/CFS discoveries continued] ...hypoperfusion, and c](/images/1px.png)
!["[ME/CFS discoveries continued] ...hypoperfusion, and c](https://pbs.twimg.com/media/E0GoAi-UYAA2XyV.jpg)
.@itsbodypolitic specifically cites the work of Ron Davis (cc @JanetDafoe) Nancy Klimas @ngklimas, Amy Proal @microbeminded2, Mike VanElzakker
@MBVanElzakker, Peter Rowe, Jarred Younger, Maureen Hanson @DrMaureenHanson, Alfred Gamboa, and foundations @4Workwell and @PolyBioRF.
@MBVanElzakker, Peter Rowe, Jarred Younger, Maureen Hanson @DrMaureenHanson, Alfred Gamboa, and foundations @4Workwell and @PolyBioRF.

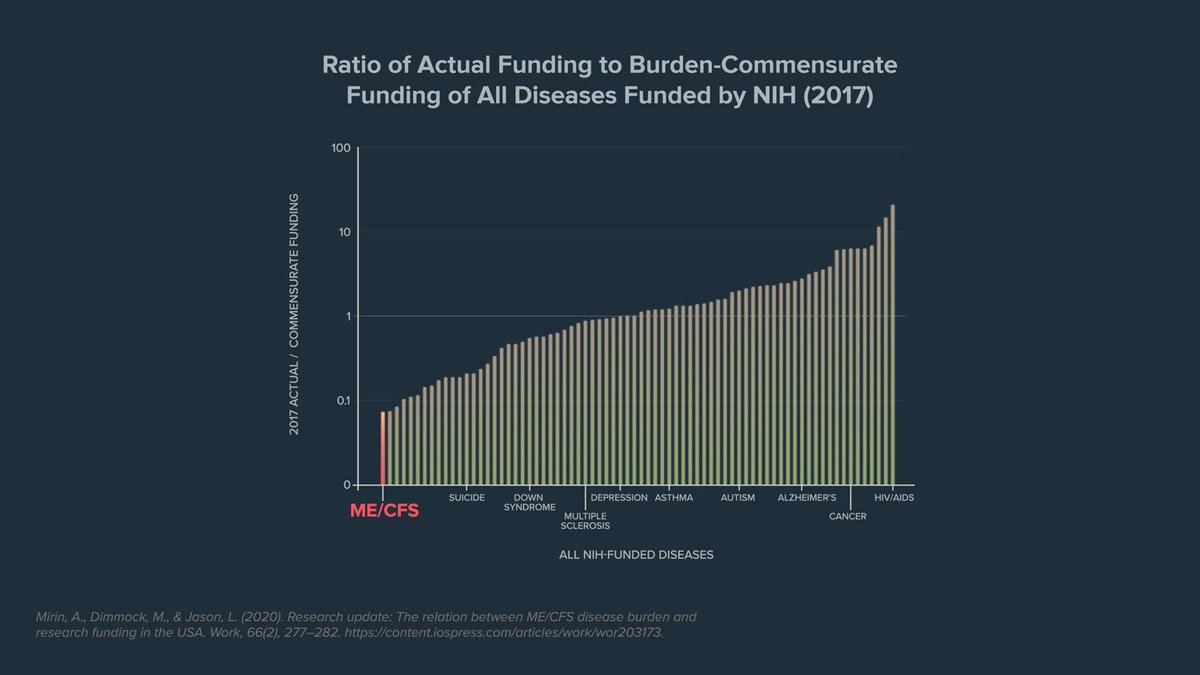
Despite enormous burden on patients and society, chronic post-viral conditions like #MECFS have been neglected for decades and we must now make up for lost time. (cc @NINDSdirector) 

So for the sake of #LongCOVID, #MECFS and related conditions we cannot waste our biggest chance at a breakthrough reinventing the wheel. 

Looking ahead, #LongCOVID #MECFS and related conditions must band together to drive change. 💪
🤝 #POTS #Fibromyalgia #Dysautonomia #MCAS #Lyme+ #GWI #EDS
👉 Read the whole open letter: wearebodypolitic.com/bodytype/2021/…
👉 For all quotes in this series, see @mecfsquotes.
🤝 #POTS #Fibromyalgia #Dysautonomia #MCAS #Lyme+ #GWI #EDS
👉 Read the whole open letter: wearebodypolitic.com/bodytype/2021/…
👉 For all quotes in this series, see @mecfsquotes.

• • •
Missing some Tweet in this thread? You can try to
force a refresh