A #tweetorial on proton pump inhibitors (PPIs)
Just for fun, which drug class is archetypal of a gastroenterologist? 😉
1/
Just for fun, which drug class is archetypal of a gastroenterologist? 😉
1/
2/
PPIs would be my pick!
The advent of these potent and effective acid suppression medications led to a paradigm shift in the mx of many GI conditions
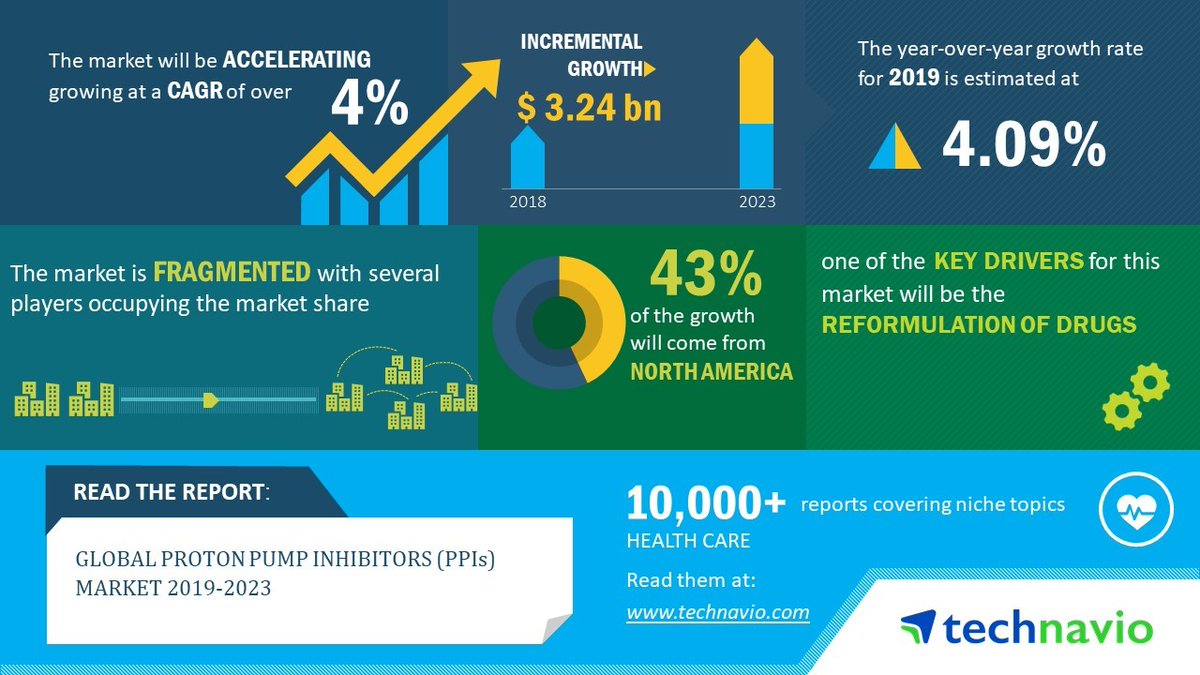
The market for PPIs is MASSIVE! Just the projected 5 year growth from 2018 - 2023 estimated to be $3.24 billion!
PPIs would be my pick!
The advent of these potent and effective acid suppression medications led to a paradigm shift in the mx of many GI conditions
The market for PPIs is MASSIVE! Just the projected 5 year growth from 2018 - 2023 estimated to be $3.24 billion!
3/
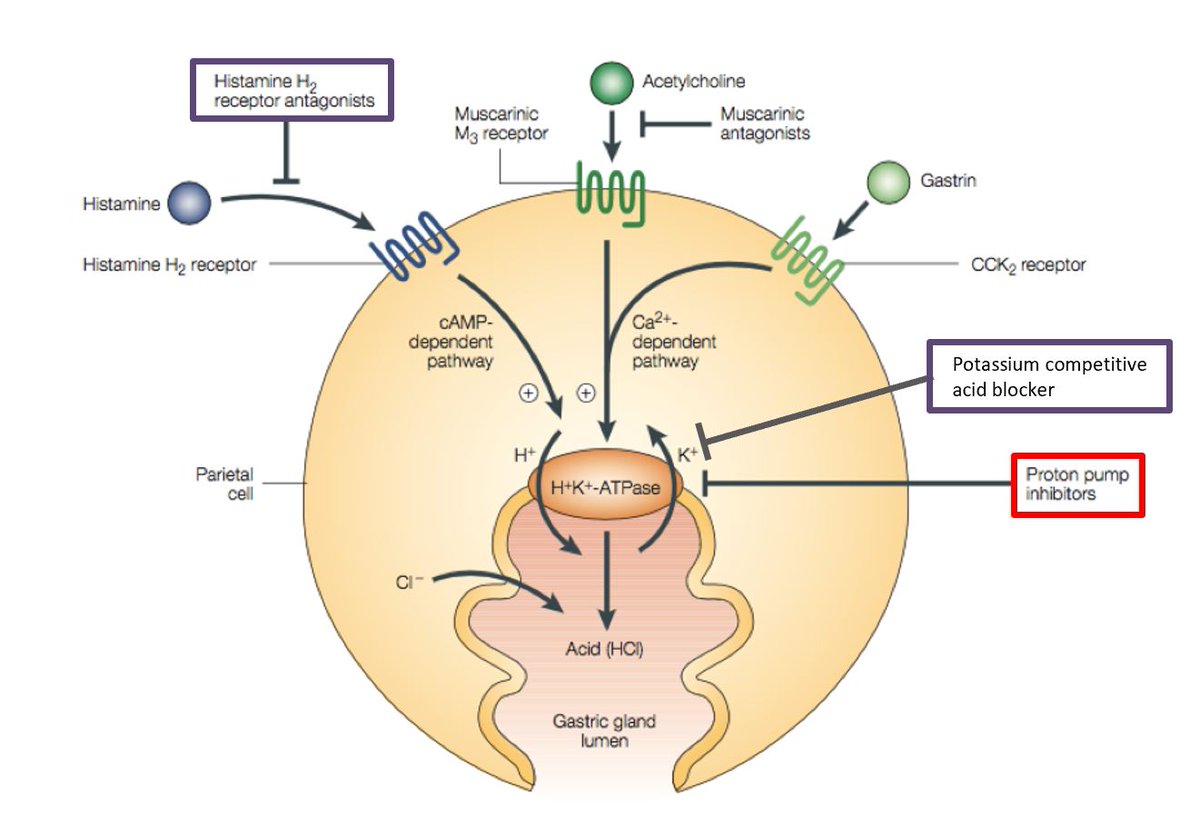
So how do #PPIs work?
A reminder on physiology: this class of drug acts on the gastric parietal cells by irreversibly blocking the hydrogen/potassium adenosine triphosphatase enzyme system (the H+/K+ ATPase, aka the gastric proton pump), hence the elegant name
So how do #PPIs work?
A reminder on physiology: this class of drug acts on the gastric parietal cells by irreversibly blocking the hydrogen/potassium adenosine triphosphatase enzyme system (the H+/K+ ATPase, aka the gastric proton pump), hence the elegant name
4/
Do they work? YES THEY DO!
They are great meds and essential for:
1⃣ Erosive esophagitis / Barrett's
2⃣ Peptic ulcer / prophylaxis for pts taking NSAIDs/aspirin / ZE
3⃣ H. pylori eradication
They are also prescribed for symptoms such as non-erosive reflux +/- dyspepsia
Do they work? YES THEY DO!
They are great meds and essential for:
1⃣ Erosive esophagitis / Barrett's
2⃣ Peptic ulcer / prophylaxis for pts taking NSAIDs/aspirin / ZE
3⃣ H. pylori eradication
They are also prescribed for symptoms such as non-erosive reflux +/- dyspepsia
5/
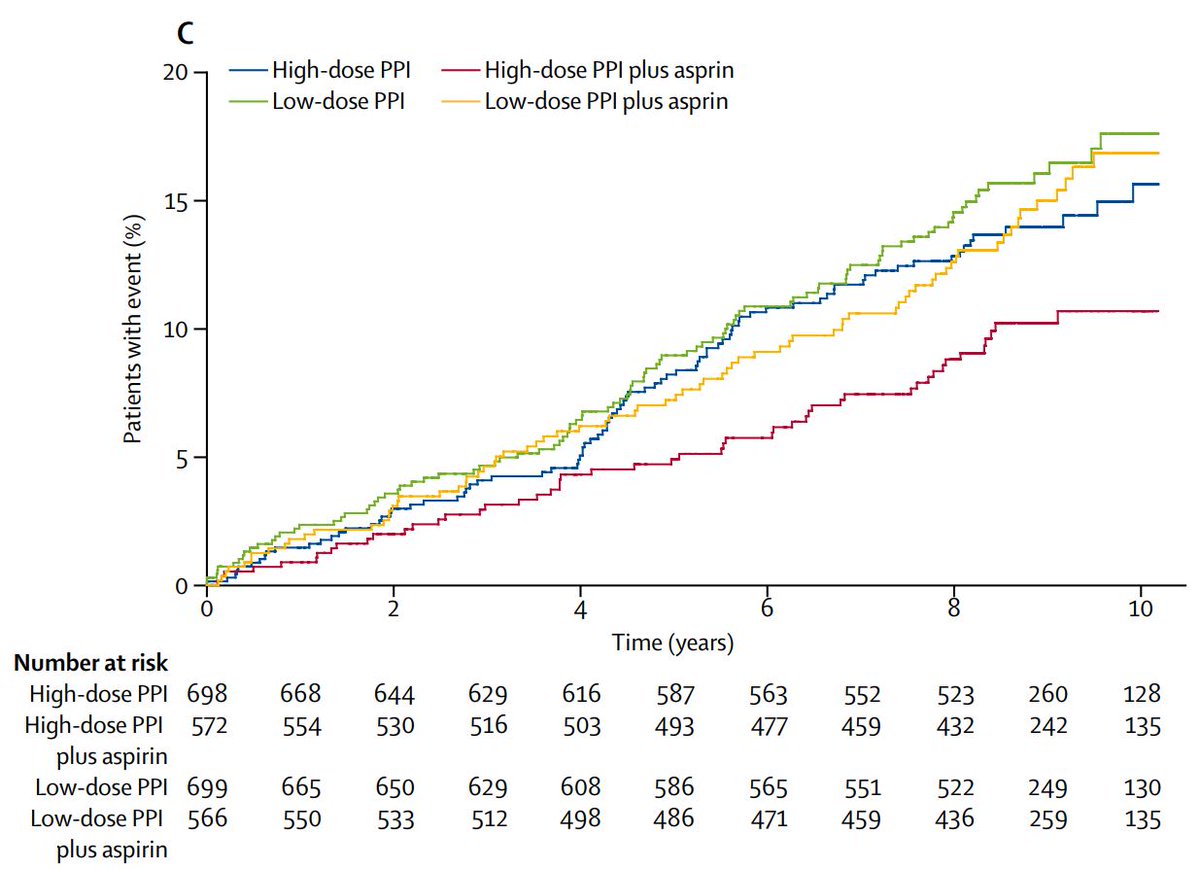
The AspECT trial in @TheLancet showed that a chemoprevention strategy of aspirin + high dose #PPI offered the best event-free survival in patients with Barrett's
thelancet.com/journals/lance…
The AspECT trial in @TheLancet showed that a chemoprevention strategy of aspirin + high dose #PPI offered the best event-free survival in patients with Barrett's
thelancet.com/journals/lance…
6/
Acute treatment of peptic ulcers has been covered in a previous thread on #UGIB
Acute treatment of peptic ulcers has been covered in a previous thread on #UGIB
https://twitter.com/RashidLui/status/1383817746010435592?s=20
7/
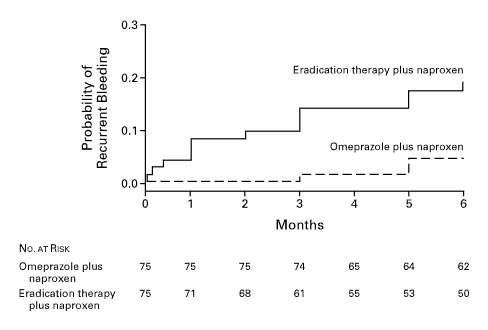
As for prophylaxis, our Dean Prof @FrancisKLChan @CUHKMedicine led a RCT in @NEJM of pts with Hx of #UGIB + H pylori infection + low dose aspirin or NSAIDs, showing that prophylaxis with PPI is better than eradication alone in preventing recurrent bleeding for NSAIDs
As for prophylaxis, our Dean Prof @FrancisKLChan @CUHKMedicine led a RCT in @NEJM of pts with Hx of #UGIB + H pylori infection + low dose aspirin or NSAIDs, showing that prophylaxis with PPI is better than eradication alone in preventing recurrent bleeding for NSAIDs
8/
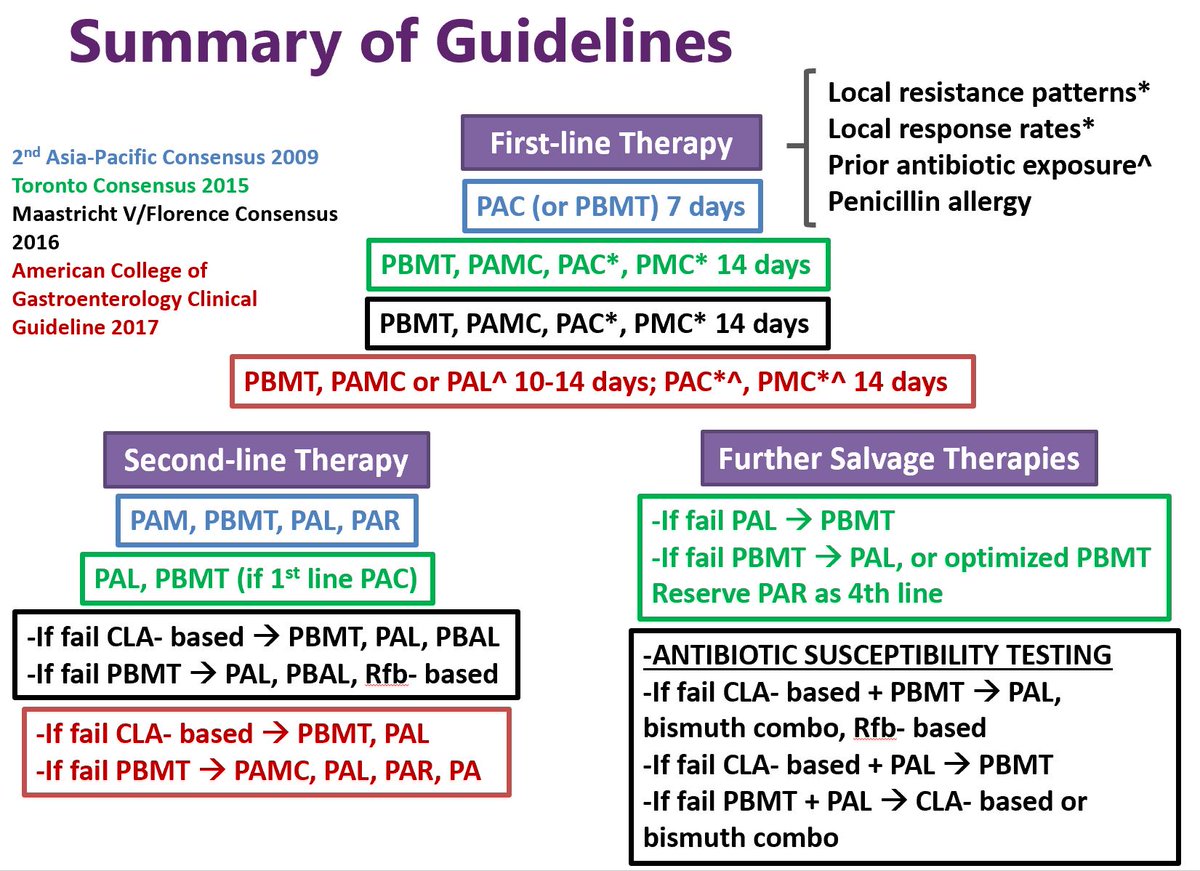
How about H pylori infection?
From the latest Maastricht V/Florence, Toronto & AP consensus, most if not all eradication regimens contain PPIs
gut.bmj.com/content/66/1/6
sciencedirect.com/science/articl…
onlinelibrary.wiley.com/doi/full/10.11…
How about H pylori infection?
From the latest Maastricht V/Florence, Toronto & AP consensus, most if not all eradication regimens contain PPIs
gut.bmj.com/content/66/1/6
sciencedirect.com/science/articl…
onlinelibrary.wiley.com/doi/full/10.11…
9/
PPIs also work for certain conditions to relief symptoms such as reflux in the absence of esophagitis +/- dyspepsia
This great tweet on the NNT for esophageal symptoms highlights that the stronger the indication, the more effective PPIs are
PPIs also work for certain conditions to relief symptoms such as reflux in the absence of esophagitis +/- dyspepsia
This great tweet on the NNT for esophageal symptoms highlights that the stronger the indication, the more effective PPIs are
https://twitter.com/EsophagusDoc/status/1388141322632974342?s=20
10/
So PPIs are great, but are they safe?
Being one of the most frequently prescribed 💊around the🌏, my take is that PPIs are largely safe
The problem actually stems from its relative safety. Many a time they are prescribed far too carefree and liberally
A discussion below:
So PPIs are great, but are they safe?
Being one of the most frequently prescribed 💊around the🌏, my take is that PPIs are largely safe
The problem actually stems from its relative safety. Many a time they are prescribed far too carefree and liberally
A discussion below:
11/
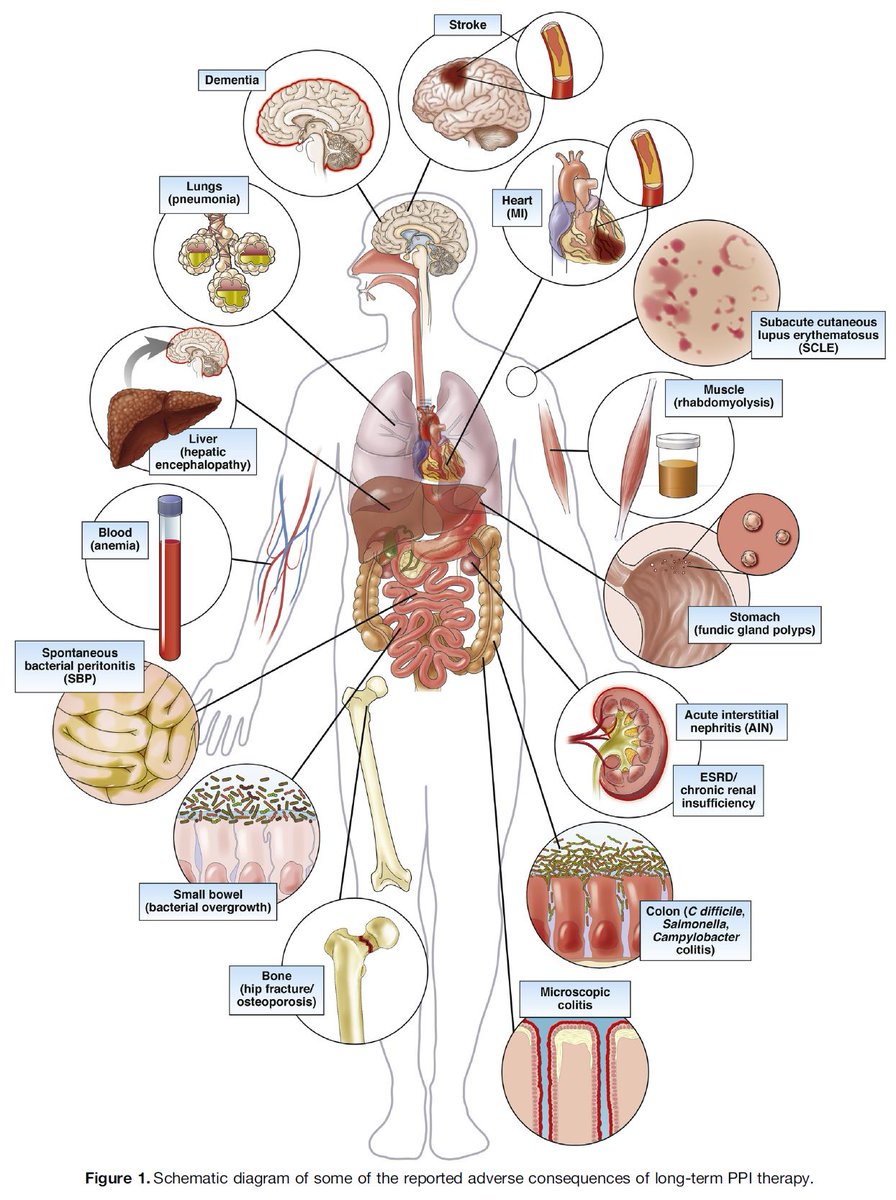
These are some of the reported adverse events associated with long term PPI use with their proposed mechanisms from a great review by Vaezi et al. @AGA_Gastro @AmerGastroAssn
pubmed.ncbi.nlm.nih.gov/28528705/

These are some of the reported adverse events associated with long term PPI use with their proposed mechanisms from a great review by Vaezi et al. @AGA_Gastro @AmerGastroAssn
pubmed.ncbi.nlm.nih.gov/28528705/

12/
This is all very scary, but what are the effect sizes?
Another excellent review by @UofT_GI_Head in @AmJGastro @AmCollegeGastro summarizes some of the recent estimates
- Enteric infections OR 2.55
- Other reported associations effect size < 2
pubmed.ncbi.nlm.nih.gov/29557943/
This is all very scary, but what are the effect sizes?
Another excellent review by @UofT_GI_Head in @AmJGastro @AmCollegeGastro summarizes some of the recent estimates
- Enteric infections OR 2.55
- Other reported associations effect size < 2
pubmed.ncbi.nlm.nih.gov/29557943/

13/
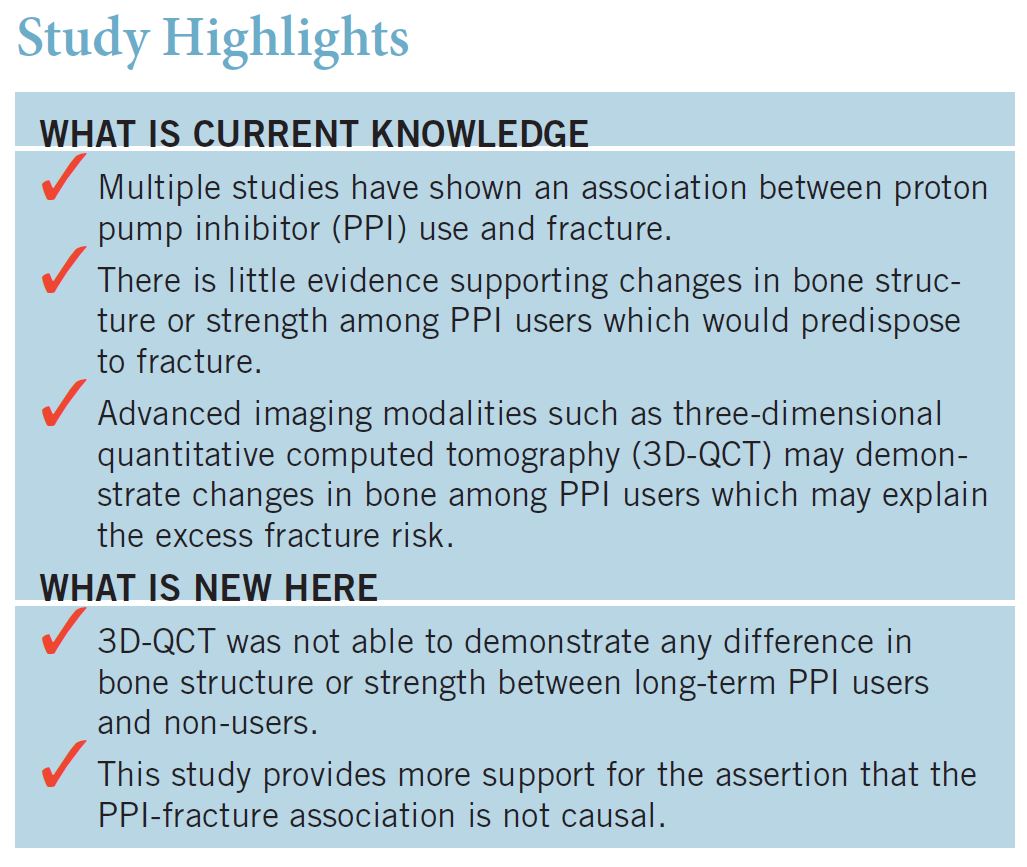
@UofT_GI_Head also did a robust study that refuted the causal association between PPI use and fractures with no differences shown using BMD, markers of bone metabolism or measures of bone strength for PPI users
pubmed.ncbi.nlm.nih.gov/27845341/
@UofT_GI_Head also did a robust study that refuted the causal association between PPI use and fractures with no differences shown using BMD, markers of bone metabolism or measures of bone strength for PPI users
pubmed.ncbi.nlm.nih.gov/27845341/
14/
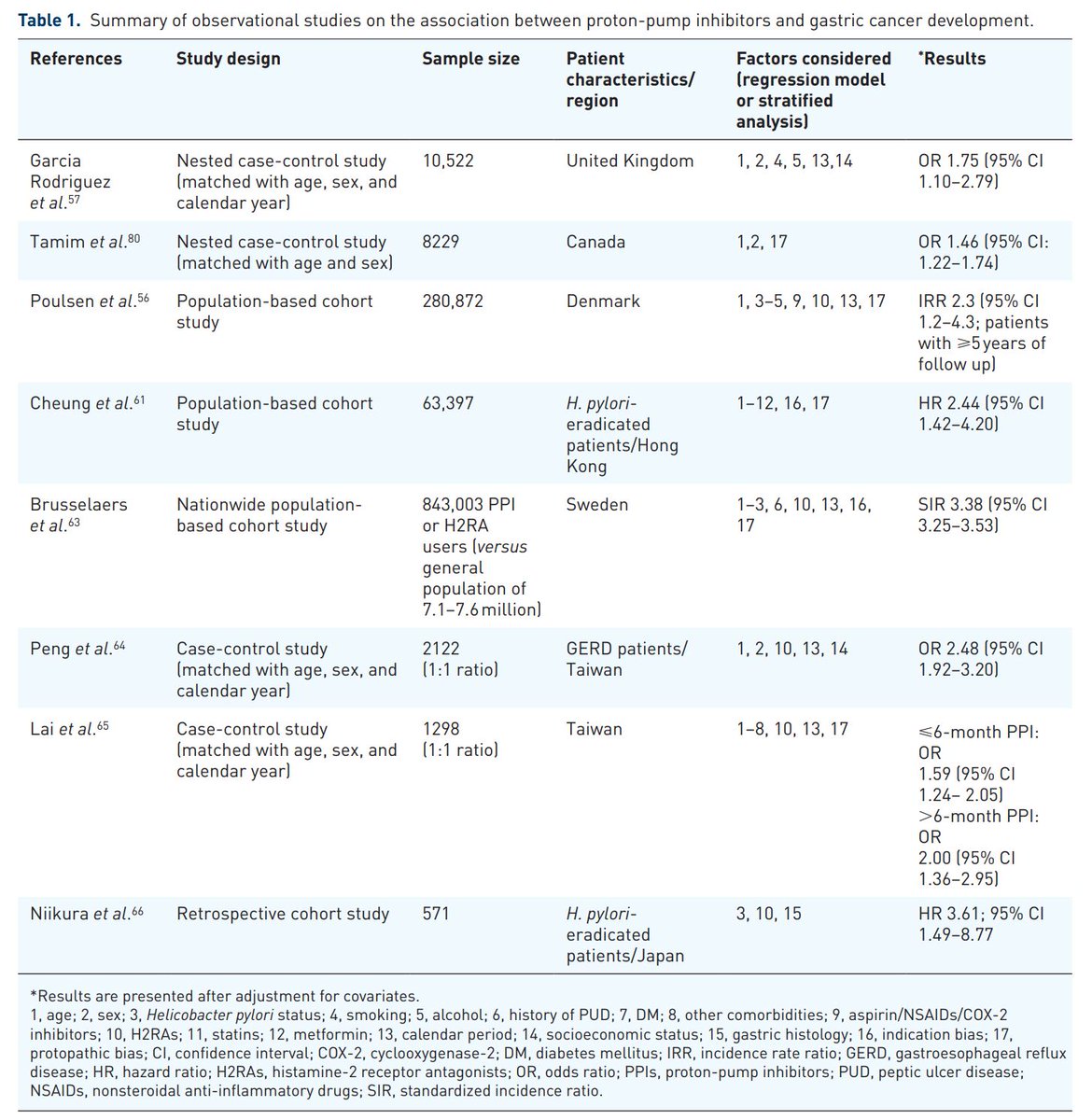
Recently, several observational studies have reported a⬆️risk of stomach cancer in long term PPI users, summarized expertly here:
📌likely limited to pts with current or past Hx of HP
📌probably already had underlying precancerous lesions
pubmed.ncbi.nlm.nih.gov/30886648/
Recently, several observational studies have reported a⬆️risk of stomach cancer in long term PPI users, summarized expertly here:
📌likely limited to pts with current or past Hx of HP
📌probably already had underlying precancerous lesions
pubmed.ncbi.nlm.nih.gov/30886648/
15/
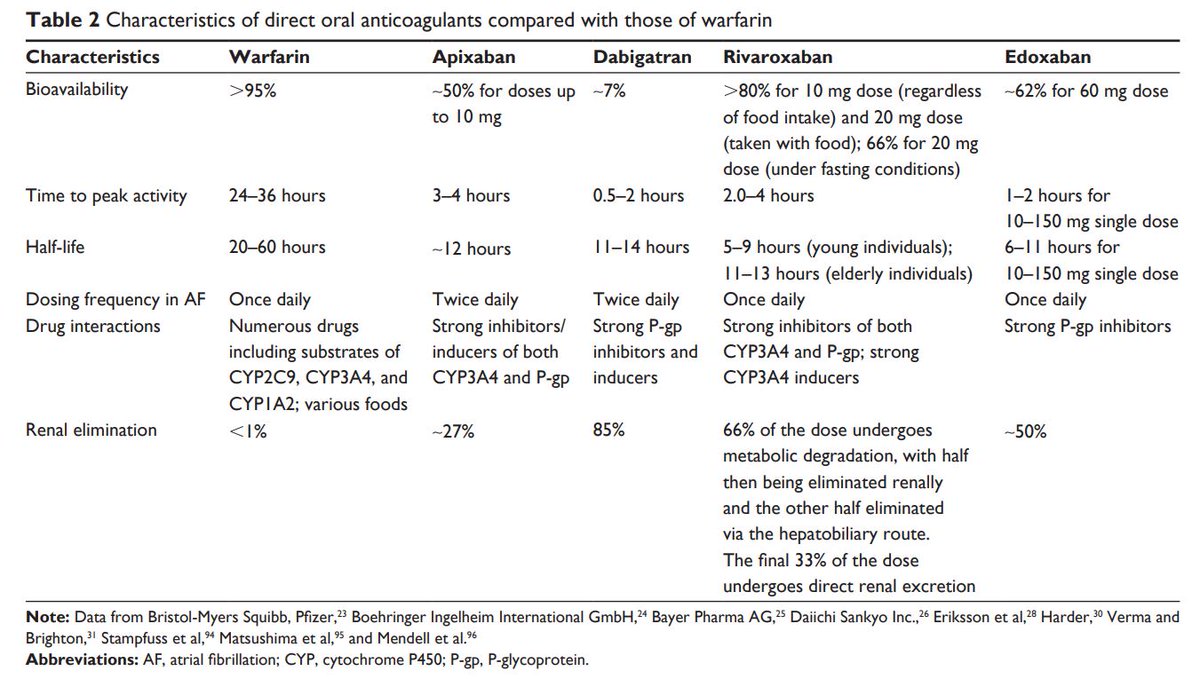
Last but not least, the potential for drug-drug interactions (DDI)
Clopidogrel (prodrug)➡️cytochrome P450 2C19➡️active metabolite
But PPIs may interfere with this which led to FDA drug label change for clopidogrel
(dex)lansoprazole & pantoprazole have less effect on this
Last but not least, the potential for drug-drug interactions (DDI)
Clopidogrel (prodrug)➡️cytochrome P450 2C19➡️active metabolite
But PPIs may interfere with this which led to FDA drug label change for clopidogrel
(dex)lansoprazole & pantoprazole have less effect on this
16/
A brief recap:
✅PPIs are great, effective and largely safe!
⚠️Though there are some safety signals
- Infections: enteric, C. difficile, pneumonia
- GI: fundic gland polyps, ⬆️CA stomach
- Micronutrient ⬇️
- Dementia
- Renal failure
- Drug-drug interactions with clopidogrel
A brief recap:
✅PPIs are great, effective and largely safe!
⚠️Though there are some safety signals
- Infections: enteric, C. difficile, pneumonia
- GI: fundic gland polyps, ⬆️CA stomach
- Micronutrient ⬇️
- Dementia
- Renal failure
- Drug-drug interactions with clopidogrel
17/
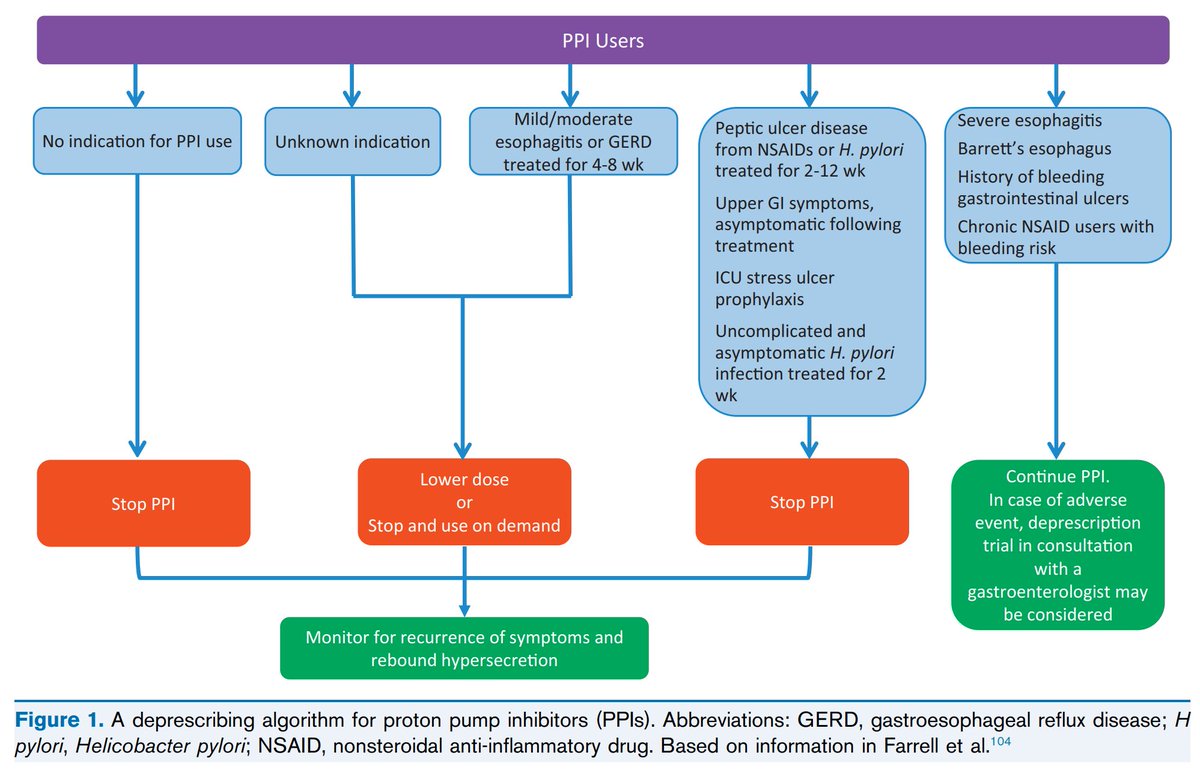
We should stop PPIs if not indicated/helping!
🦪from @UofT_GI_Head on deprescribing PPIs:
🔭look out for rebound gastric acid hypersecretion
🧠mindful of rebound symptoms
🗓️take PPIs every other day for 2 weeks, 2x/week for 2 weeks, then stop
pubmed.ncbi.nlm.nih.gov/29557943/
We should stop PPIs if not indicated/helping!
🦪from @UofT_GI_Head on deprescribing PPIs:
🔭look out for rebound gastric acid hypersecretion
🧠mindful of rebound symptoms
🗓️take PPIs every other day for 2 weeks, 2x/week for 2 weeks, then stop
pubmed.ncbi.nlm.nih.gov/29557943/
18/
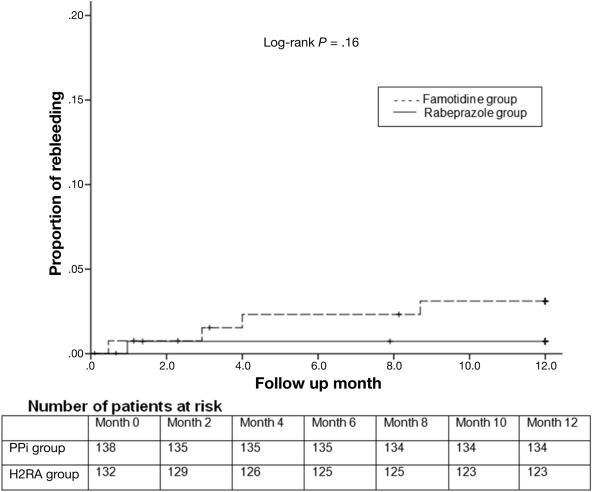
In some circumstances H2RA can perform quite well too
Though pts on low-dose aspirin (LDA) + PPI had a slightly lower proportion of recurrent bleeding or ulcer compared with H2RA this was not statistically significant in this study
🤔Reasonable to switch to LDA + H2RA?
In some circumstances H2RA can perform quite well too
Though pts on low-dose aspirin (LDA) + PPI had a slightly lower proportion of recurrent bleeding or ulcer compared with H2RA this was not statistically significant in this study
🤔Reasonable to switch to LDA + H2RA?
19/
To conclude, good practice when prescribing PPIs:
- Discuss on indications and potential SEs
- ⚖️risks and benefits
- Consider🔁acid suppressants
- ⬇️possible dose to control symptoms
- 🛑Deprescribe PPIs, not just abruptly stop them
P.S great algorithm by @grepmeded
To conclude, good practice when prescribing PPIs:
- Discuss on indications and potential SEs
- ⚖️risks and benefits
- Consider🔁acid suppressants
- ⬇️possible dose to control symptoms
- 🛑Deprescribe PPIs, not just abruptly stop them
P.S great algorithm by @grepmeded
20/
I had a great time preparing this and I hope you enjoyed this thread too! Don't be shy to share/re-tweet😉!
I had a great time preparing this and I hope you enjoyed this thread too! Don't be shy to share/re-tweet😉!
21/
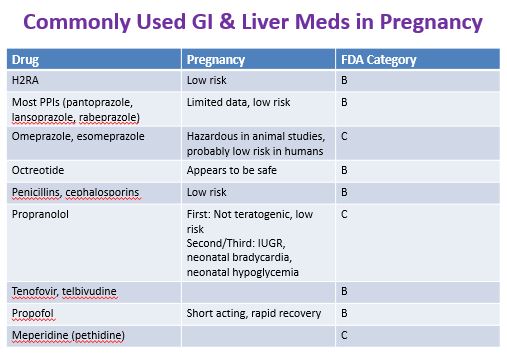
Easter egg #1
A selection of PPIs are safe even in pregnancy
Bearing in mind this is referring to usual approved dosages such as for GERD and not, for example infusional regimens used in UGIB
Easter egg #1
A selection of PPIs are safe even in pregnancy
Bearing in mind this is referring to usual approved dosages such as for GERD and not, for example infusional regimens used in UGIB
• • •
Missing some Tweet in this thread? You can try to
force a refresh