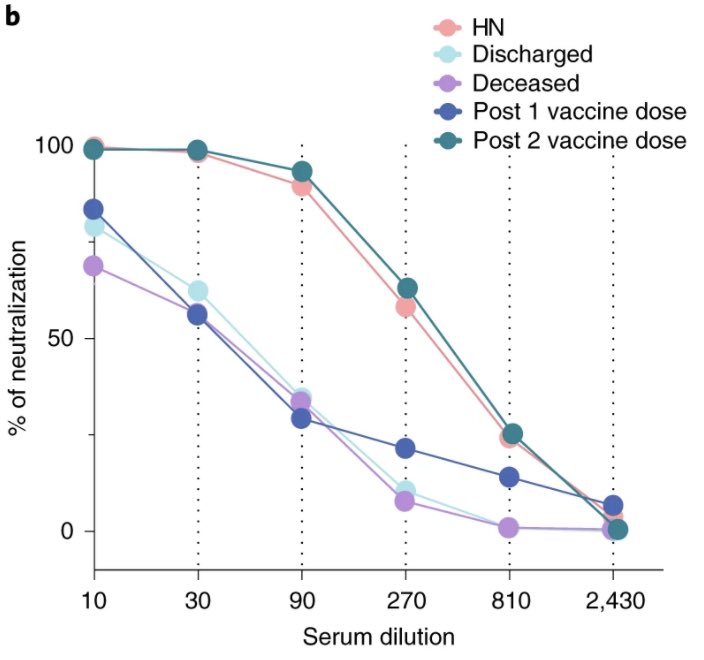
So wonderful to see this work published! Timing is everything when it comes to immune control of COVID. Neutralizing antibody production is delayed in lethal COVID. By the brilliant @carolilucas @sneakyvirus1 & #YaleIMPACT team 💪🏼(1/n)
https://twitter.com/NatureMedicine/status/1389975204684775431
For explanation about this study, please read this thread (2/n) 👇🏽
https://twitter.com/VirusesImmunity/status/1342898928497418240?s=20
One additional piece of data to highlight - mRNA vax 1st shot (28 days) induces NAb comparable to hospitalized patients. Post 2nd shot vax (7 days) induces ⬆️ ⬆️ levels of NAb comparable to high neutralizers (HN). Thanks to @InciYildirim11 @SaadOmer3 #VaccinesWork (end) 
• • •
Missing some Tweet in this thread? You can try to
force a refresh