Should vaccinated people stop wearing masks?
Happy to contribute to article @B_resnick w @MonicaGandhi9 @AbraarKaran @DocJeffD @DrJeanneM
Short thread w/ my perspective on how to navigate CDC guidance on masks post-vaccination.
vox.com/science-and-he…
Happy to contribute to article @B_resnick w @MonicaGandhi9 @AbraarKaran @DocJeffD @DrJeanneM
Short thread w/ my perspective on how to navigate CDC guidance on masks post-vaccination.
vox.com/science-and-he…
1st: Protection from vaccination is NOT 100% (no surprise to anyone that follows me to hear this)
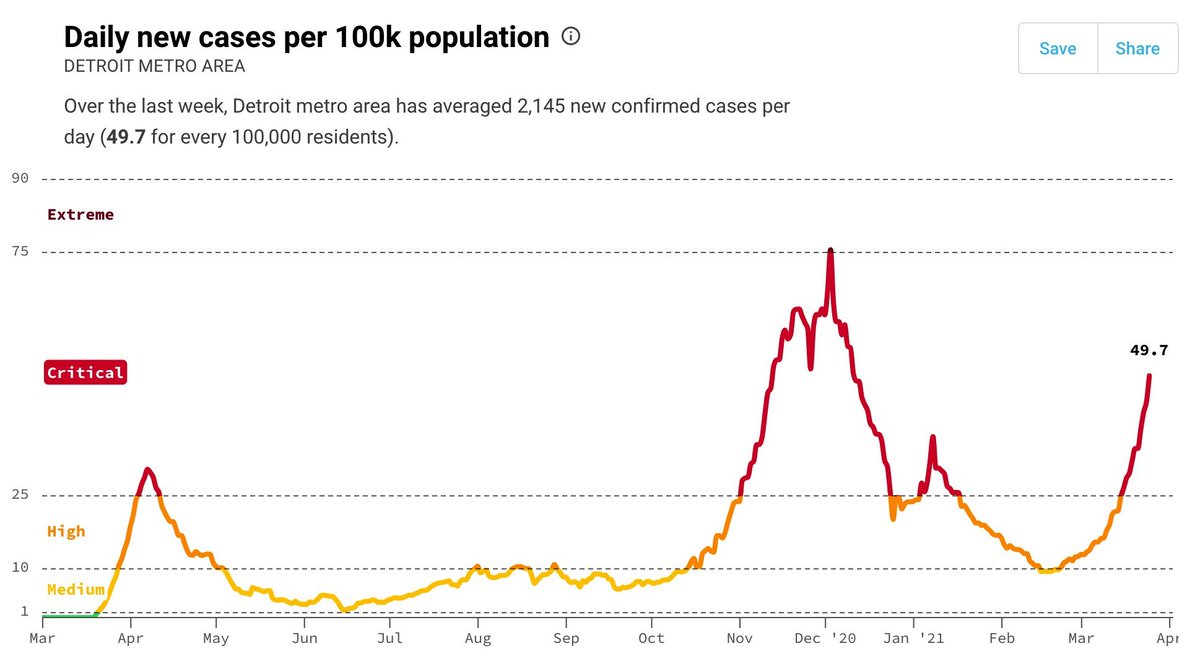
So, despite being vaccinated, I'm still going to wear a mask in what I consider high(er) risk situations - indoors w/ dozens of households, unless community transmission is VERY low.
So, despite being vaccinated, I'm still going to wear a mask in what I consider high(er) risk situations - indoors w/ dozens of households, unless community transmission is VERY low.
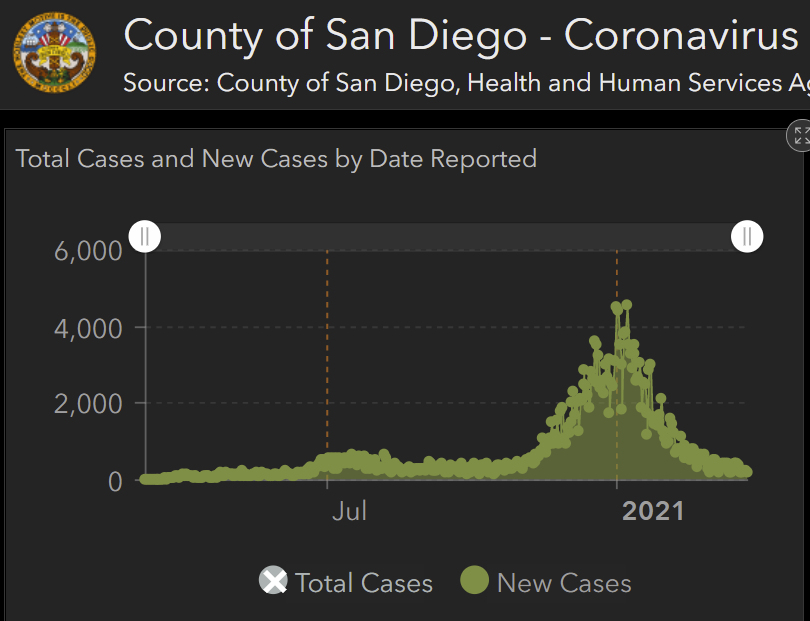
What is very low? My perspective: CA (where I live) has tiers based on daily cases/100K. Lowest tier is <2/100K. If we assume there are 5 infections/case & people are infectious for 10d, this translates to 1/1K. Pretty low. If everyone is vaccinated, risk ~10x+ lower so <1/10K.
So if everyone at indoor event was vaccinated in a county w/ <2 cases/day/100K, then if there were 100 people at event, prob of 1+ infected person would be <1%. I'd prefer prob to be <0.1%. So I'd unmask at 10 person dinner but not 100+ person dance party. @joshuasweitz
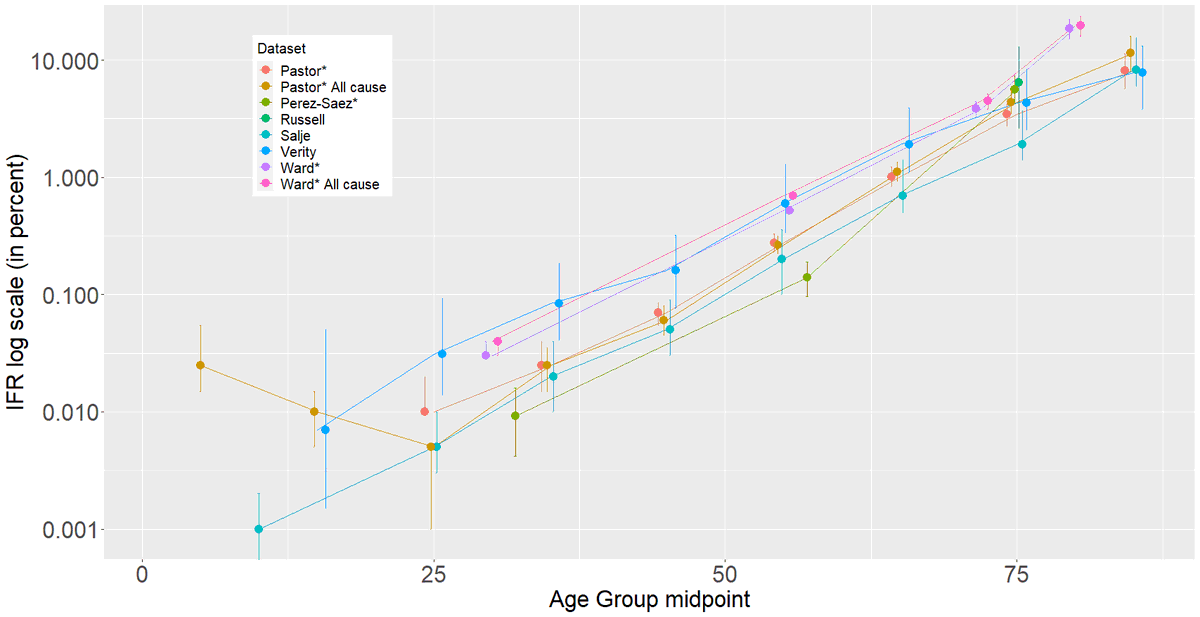
I am ~50 yr old, no major pre-existing conditions. If I were older or at-risk, my risk tolerance would go down. If younger, or more risk-tolerant (ride motorcycles @ 100+mph, into base-jumping), then maybe 100+ person vaccinated dance party is ok.
No hard rule, but an idea of how to think about it. @Bob_Wachter has a similar approach (
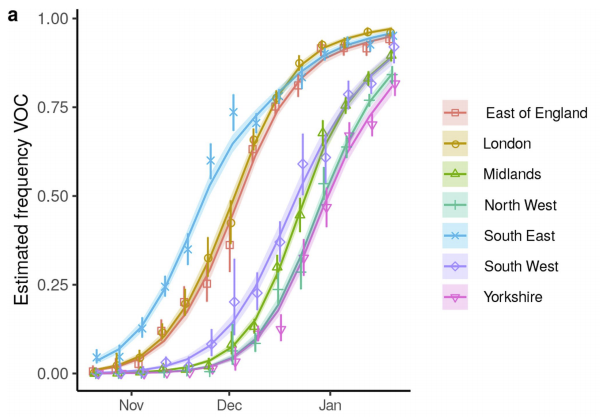
https://twitter.com/Bob_Wachter/status/1394464848503656451), but uses % of asymptomatic people testing positive in SF to assess risk. If only all of US had data like this (like UK does!). There is this: nytimes.com/interactive/20…
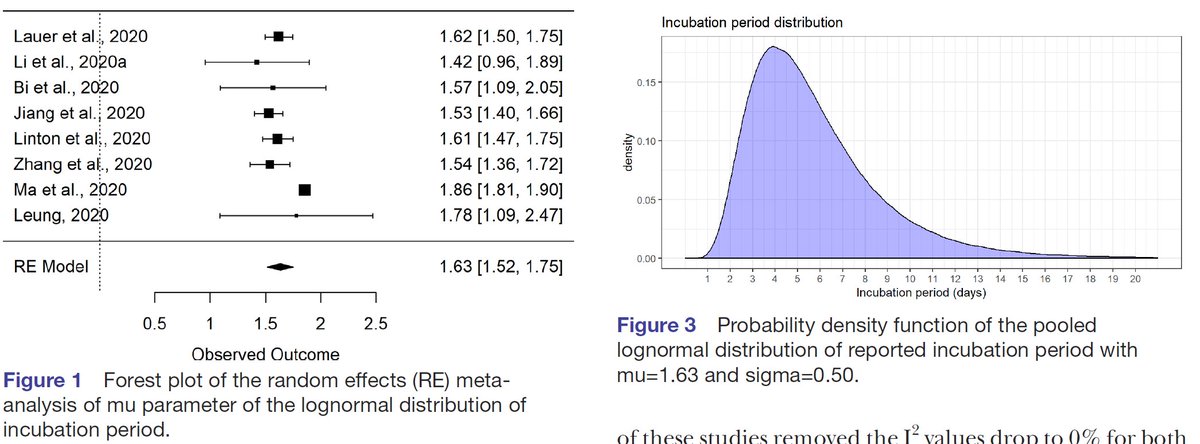
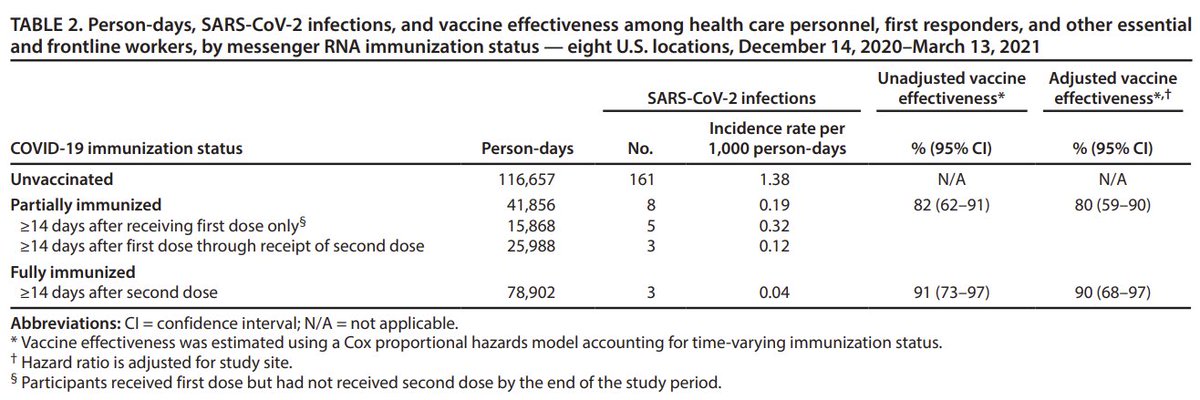
2nd, I live w/ another person so I also have to think of them. Full mRNA vaccination reduces risk of infection + transmission by ~85-95% (
https://twitter.com/DiseaseEcology/status/1365382623036534784). Again, not 100%. So, in addition to protecting myself, I'll mask in high(er) risk situations (see above).
As above, adjust your risk tolerance to include chance that your household member might get sick if exposed to virus from you. If they are unvaccinated, older, or at-risk for severe disease, adjust accordingly.
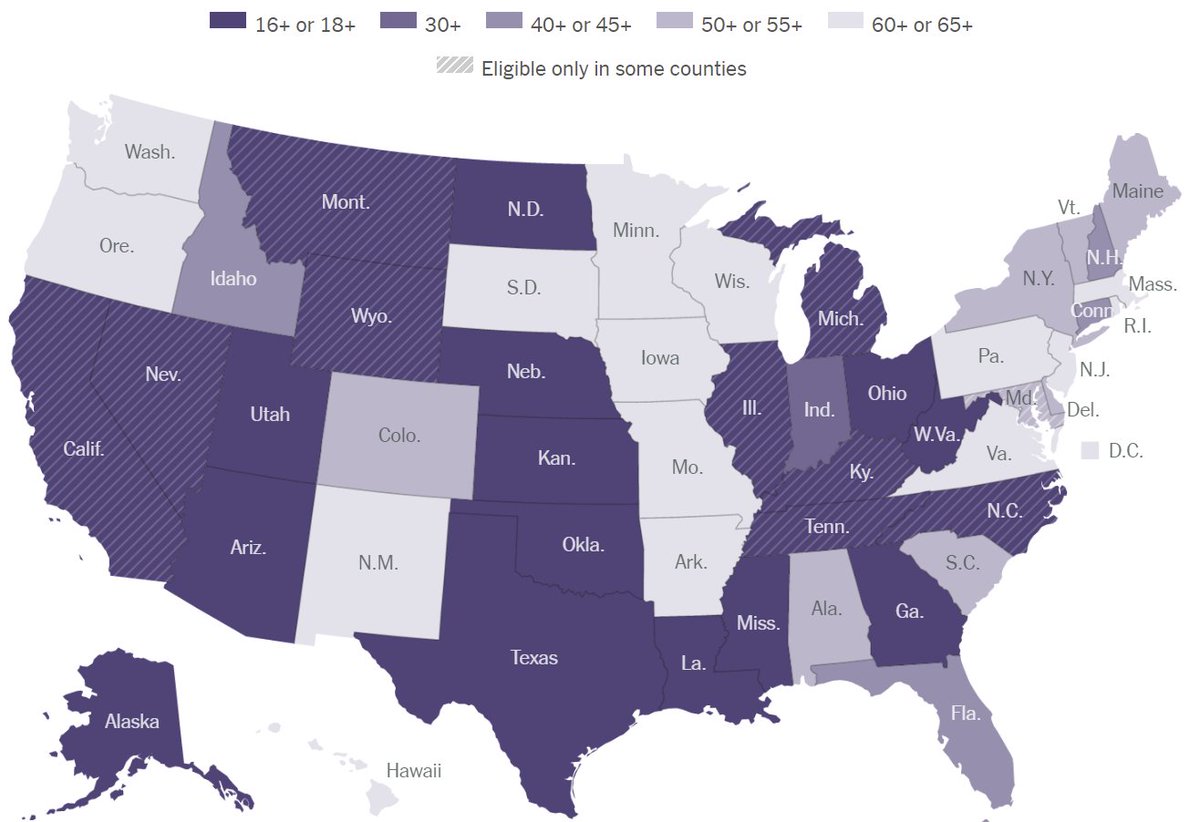
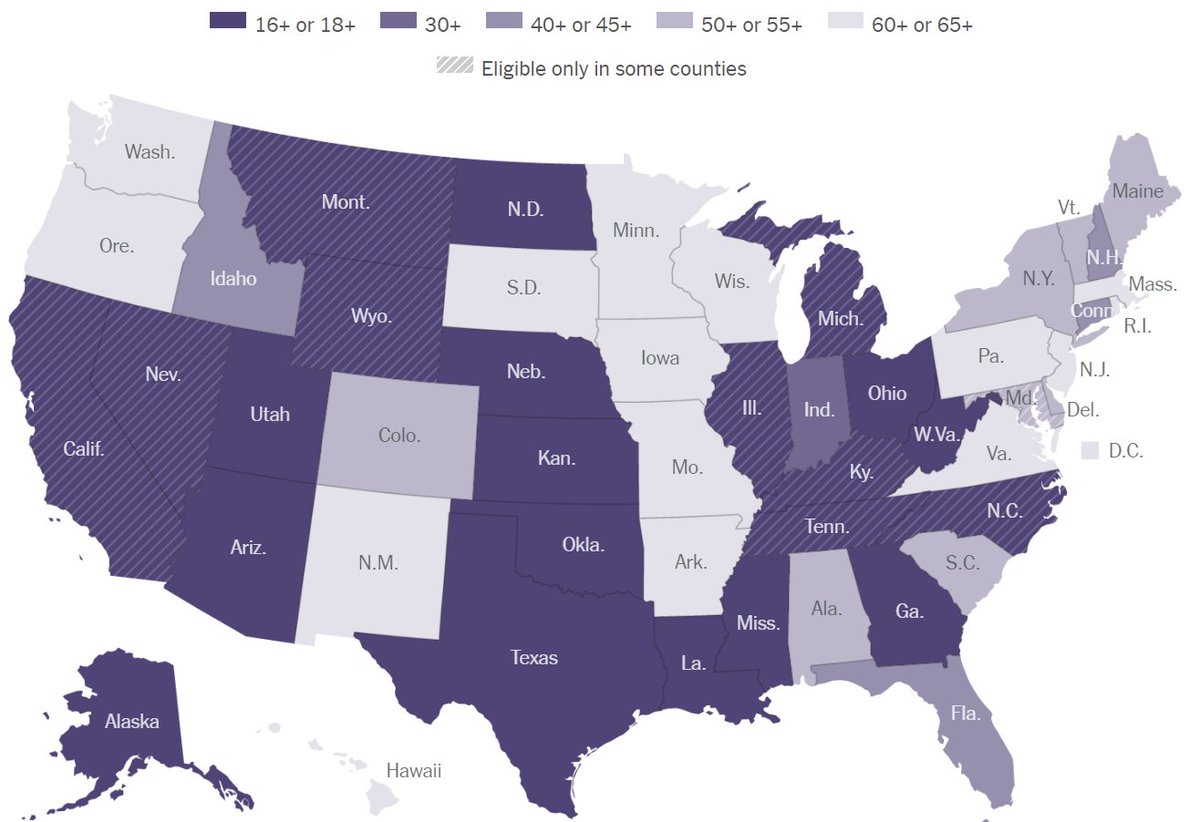
Thus, I'd have preferred CDC guidance on masks post-vaccination to be more honest & include nuance (right @zeynep?): "Post-vaccination, you don't need a mask outdoors, or indoors in lower risk settings: (small gatherings in low-medium risk areas: nytimes.com/interactive/20…). (cont)
In higher risk indoor settings (e.g. large gatherings in moderate or higher risk areas nytimes.com/interactive/20…), please continue to wear a mask, especially if you or your household members are older or at risk for severe disease."
Finally, if incentivizing vaccination was one of they key reasons for loosening mask requirements, then why not make the explicit link b/w vaccination & masks: "The more people are vaccinated, the faster cases will fall, making everyone safer, and eliminating the need for masks."
• • •
Missing some Tweet in this thread? You can try to
force a refresh