Happening now! 1/
https://twitter.com/ahandvanish/status/1404467563795566602
On those who participated in the survey on the clinical case definition - Patient AND Researcher is a new category (requested by @Dr2NisreenAlwan and yours truly) :)
2/
2/

@Dr2NisreenAlwan up first! Doctors need to do better and avoid generating stigma. She shares excellent data showing that those without lab confirmation don't get enough time off or adequate rest, resulting in worsened #LongCOVID as measured by ability to care for themself 4/ 



@BrodinPetter talks about #LongCOVID in children and three possible explanations: persistent virus, autoimmunity, or an autoinflammatory response 5/ 

Dr. Anna Funk: few differences between pos and negative-tested child patients w/r/t number of symptoms 6/ 

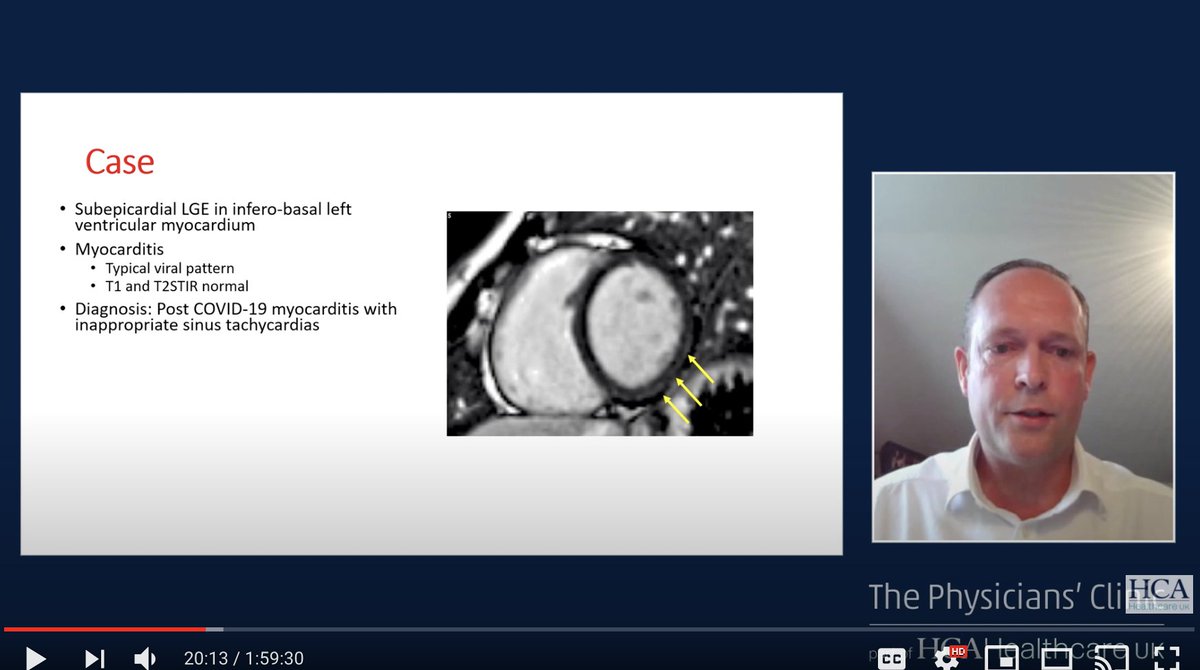
Dr. Jonigk and Dr. Ackermann on vascular injury. There are ongoing vascular alterations and endothelial dysfunction! 7/ 





Missed 2 talks but @VirusesImmunity is up next!
Three hypotheses for #LongCOVID:
1. Viral reservoir (would not be picked up by PCR)
2. Autoreactive lymphocytes
3. Tissue damage, including in vascular
(Not mutually exclusive!) 8/
Three hypotheses for #LongCOVID:
1. Viral reservoir (would not be picked up by PCR)
2. Autoreactive lymphocytes
3. Tissue damage, including in vascular
(Not mutually exclusive!) 8/

@VirusesImmunity There is evidence for all of these hypotheses. Here is a screenshot showing that in 5 of 14 patients, COVID antigens were found in intestinal tissue.
She and her colleagues have looked at autoantibodies in severe patients but are expanding to #LongCOVID 9/
She and her colleagues have looked at autoantibodies in severe patients but are expanding to #LongCOVID 9/

@VirusesImmunity Major point! Patients with autoantibodies to B cells had reduced B cell number and function.
"[Moderate] patients failed to mount an antibody response....not only do autoantibodies interfere with B cells, but they also interfere with their function." 10/
"[Moderate] patients failed to mount an antibody response....not only do autoantibodies interfere with B cells, but they also interfere with their function." 10/

@VirusesImmunity Vaccines can both improve & worsen #LongCOVID patients & this could be a clue to the pathophysiology.
By the way, this study (which @patientled gave the patient perspective on) is still recruiting for non-vaccinated Long COVID patients within driving distance of New Haven! 11/
By the way, this study (which @patientled gave the patient perspective on) is still recruiting for non-vaccinated Long COVID patients within driving distance of New Haven! 11/

We're in the working groups now (I'm in the pathophysiology one).
Exciting comment from Dr. Nancy Klimas @ngklimas:
12/
Exciting comment from Dr. Nancy Klimas @ngklimas:
12/

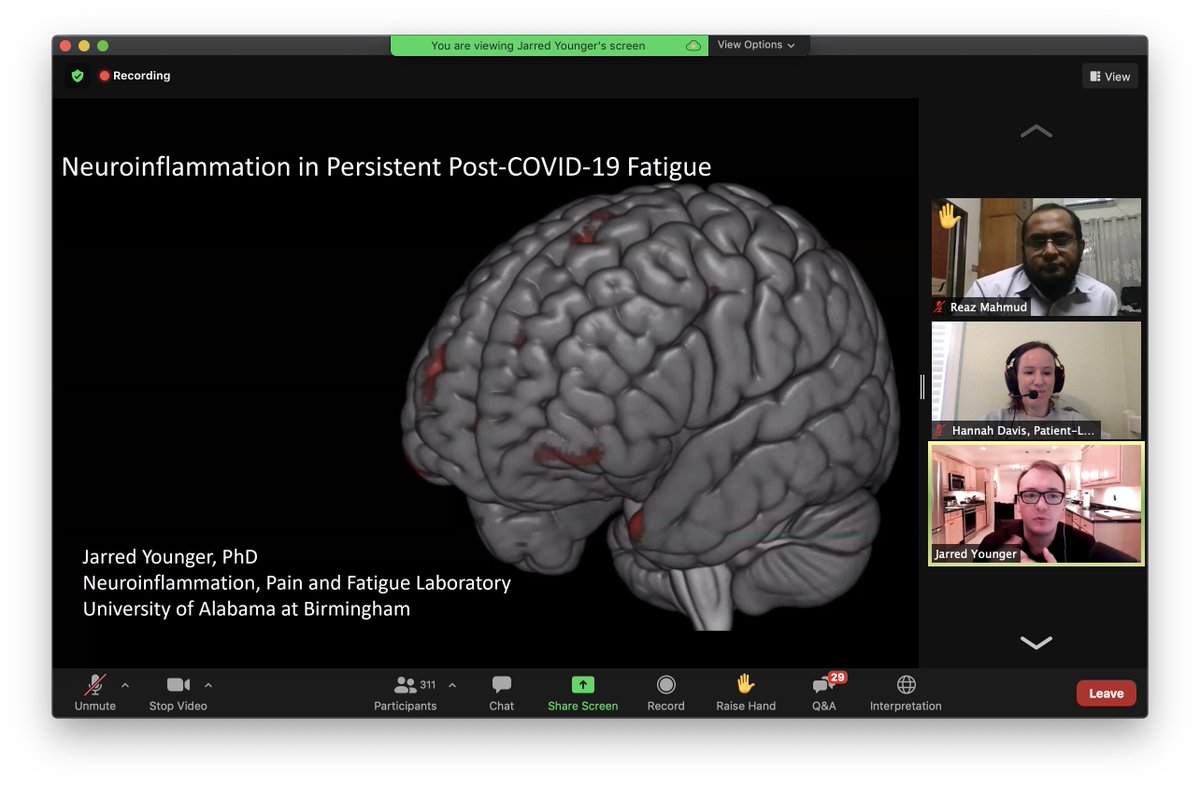
Sooooooo excited to hear Dr. Jarred Younger here on neuroinflammation AND neuroimaging techniques.
Microglia activation causes an inflammatory state. He is talking about several neuro markers including elevated lactate in the brain and elevated brain temperature!
13/


Microglia activation causes an inflammatory state. He is talking about several neuro markers including elevated lactate in the brain and elevated brain temperature!
13/


Phew, wrapping up. Now on to the working group summaries.
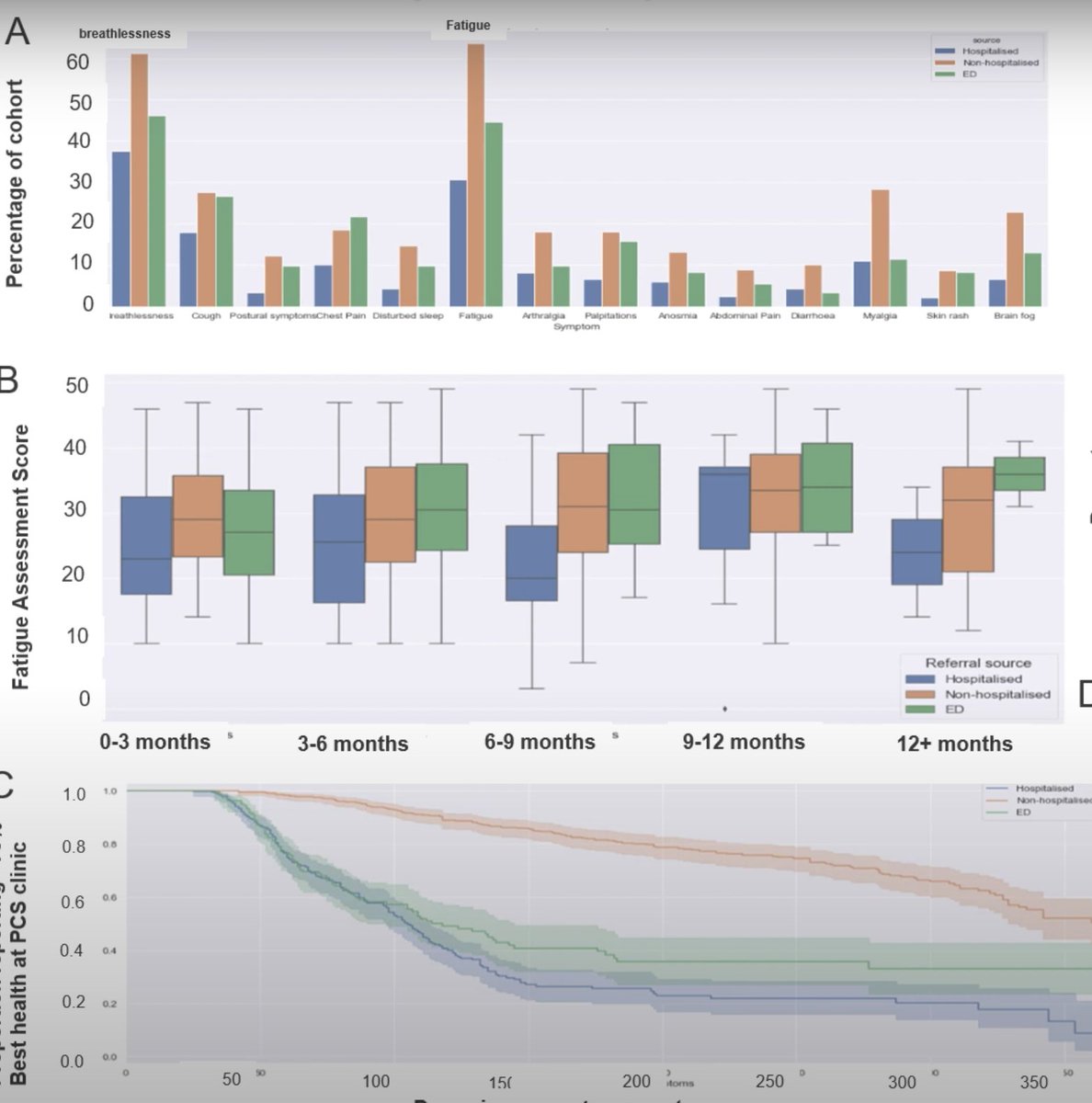
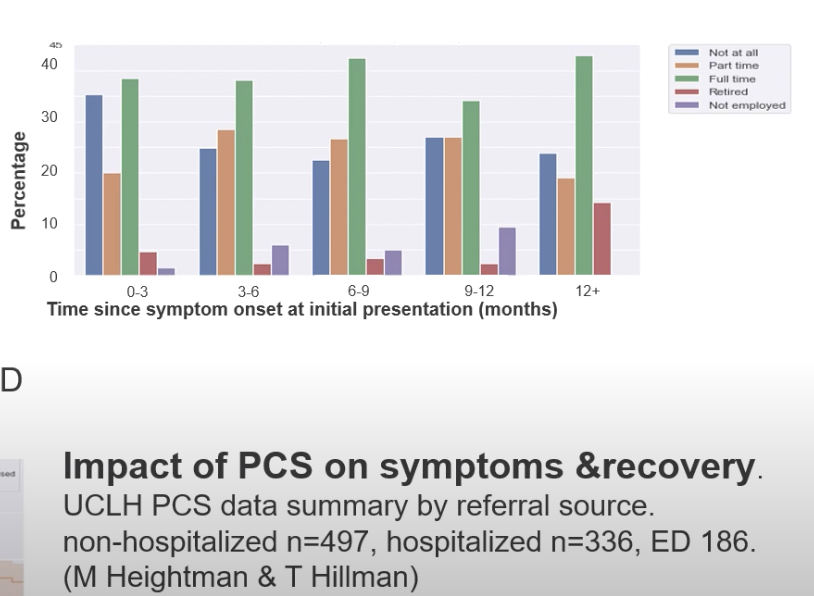
Care models working group:
-they make the very important point that even though #LongCOVID is more probable in hospitalized patients, the vast majority and count of LC patients are non-hospitalized
15/
Care models working group:
-they make the very important point that even though #LongCOVID is more probable in hospitalized patients, the vast majority and count of LC patients are non-hospitalized
15/
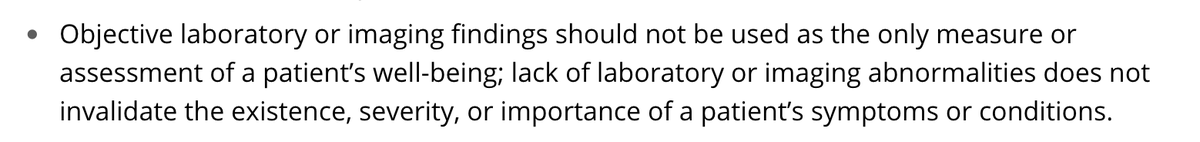
Care Models working group:
-Services must be driven by patient-led perspectives
-need advocates to listen to listen to lived experiencee
-can't rely on physiological normal parameters (my side note - we haven't even figured out tests yet)
16/
-Services must be driven by patient-led perspectives
-need advocates to listen to listen to lived experiencee
-can't rely on physiological normal parameters (my side note - we haven't even figured out tests yet)
16/
-post infectious diseases/research, which are historically underfunded, need to be paid attention
-overwhelmingly a huge need especially in non-hospitalized patients
-urgent need for an acceptable level of holistic care
-need upskilling (medical provider ed) & bundled care
17/
-overwhelmingly a huge need especially in non-hospitalized patients
-urgent need for an acceptable level of holistic care
-need upskilling (medical provider ed) & bundled care
17/
-access to care pathways is vital especially to not exacerbate inequalities
-pathways need to be complex (multiple specialities, bundling services together)
#LongCOVID
18/
-pathways need to be complex (multiple specialities, bundling services together)
#LongCOVID
18/
-Many non-hospitalized patients weren't admitted to hospitals because of hospital capacity alone and we shouldn't be calling all non-hospitalized patients "mild"
19/
19/
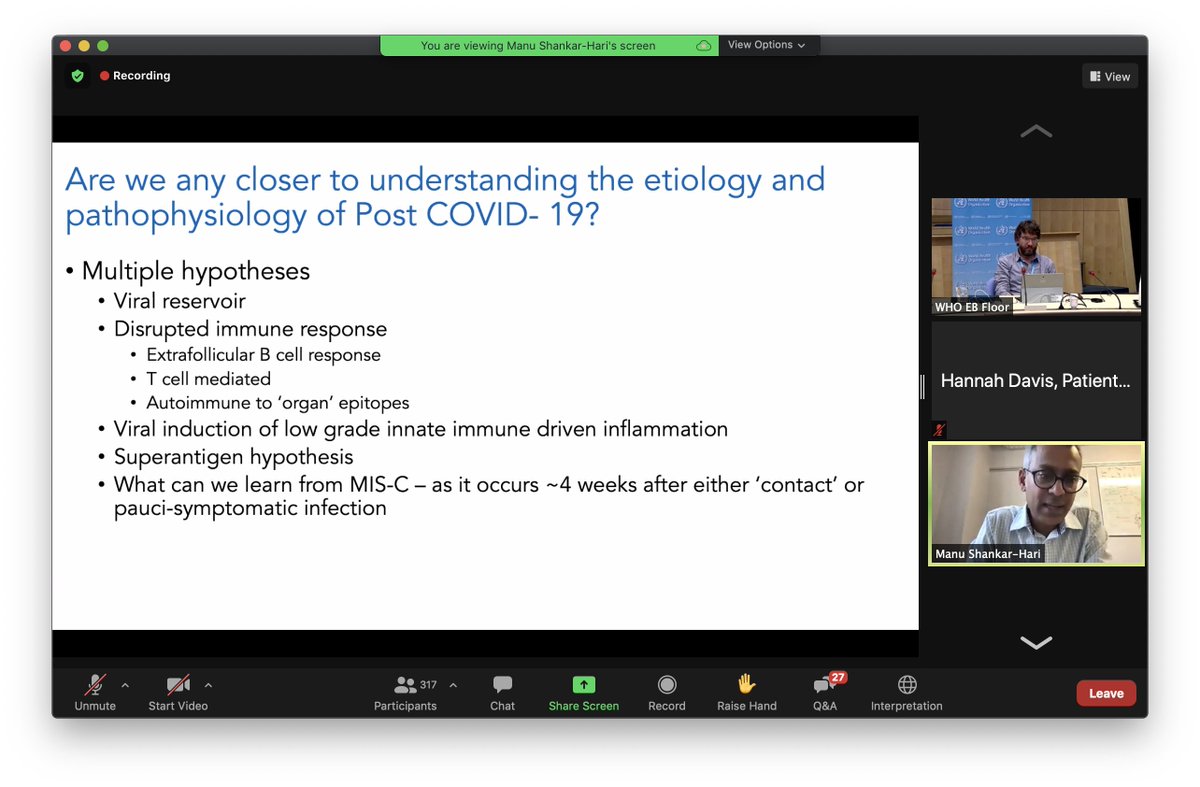
Pathophysiology working group:
-not sure we are any closer to pathophysiology, but many possible theories (including many not listed here, like neuroinflammation etc)
I missed a few slides here but will revisit when the recording is out
20/
-not sure we are any closer to pathophysiology, but many possible theories (including many not listed here, like neuroinflammation etc)
I missed a few slides here but will revisit when the recording is out
20/
Wrapping up from WHO's Mike Ryan:
In the US 18-49 year olds are the largest symptomatic group. With 91 million symptomatic cases - even a rare condition with these numbers is common. We need a societal approach to this.
[14% of 91 million is 13million people w' #LongCOVID]
21/
In the US 18-49 year olds are the largest symptomatic group. With 91 million symptomatic cases - even a rare condition with these numbers is common. We need a societal approach to this.
[14% of 91 million is 13million people w' #LongCOVID]
21/
"There is a decay curve in society's concern. Sometimes people are made to feel like they should shut up & move on. We owe it to the people who are suffering to give them the best science possible. There is a danger in the moment like this that people stop talking about this" 22/
we need to keep this conversation going and keep it going in public, with policymakers.
We can't leave anyone behind. It's not just about vaccines, it's about leaving nobody behind FOREVER. And that takes a commitment."
#LongCOVID
23/
We can't leave anyone behind. It's not just about vaccines, it's about leaving nobody behind FOREVER. And that takes a commitment."
#LongCOVID
23/
• • •
Missing some Tweet in this thread? You can try to
force a refresh