Proud to have been a Subject Matter Expert to the POTUS Health Equity Task Force!
They're presenting today on what they learned about #LongCOVID (hhs.gov/live) & their presentation is so full of good recommendations that I can't even keep up.
1/
They're presenting today on what they learned about #LongCOVID (hhs.gov/live) & their presentation is so full of good recommendations that I can't even keep up.
1/

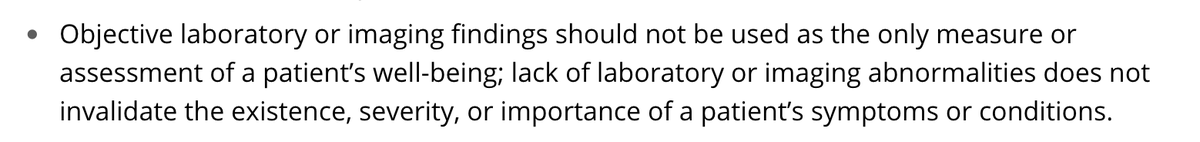
I'm thrilled at their takeaways, including 1) lab confirmation of COVID can't be required for care, 2) creating a federal advisory committee including LC patients, ME experts, & disability advocates, 3) help patients navigate the disability system & expediting claims, & others 2/
Excellent public comments from Michael Sieverts on how biases in PCR and antibody testing will trickle their way into research. Super important as research plans for #LongCOVID are currently being decided....
3/
3/
Some examples of bias:
1) PCR: positive results are related to how early you get tested (false negative rates increase every day from day 3 of symptoms) so PCR-negative patients are less likely to have good access to healthcare
2) Antibody tests:
4/
1) PCR: positive results are related to how early you get tested (false negative rates increase every day from day 3 of symptoms) so PCR-negative patients are less likely to have good access to healthcare
2) Antibody tests:
https://twitter.com/ahandvanish/status/1387140392794079236
4/
• • •
Missing some Tweet in this thread? You can try to
force a refresh