
ATTENTION: Alberta Parents, Teachers, Workers
Don’t hold your breath waiting for HEPA filters to be installed in schools & workplaces this summer
The @AHS_media Scientific Advisory Group Co-Chair doesn’t think there’s enough evidence.
Important addendum to this thread.
1/20🧵
Don’t hold your breath waiting for HEPA filters to be installed in schools & workplaces this summer
The @AHS_media Scientific Advisory Group Co-Chair doesn’t think there’s enough evidence.
Important addendum to this thread.
1/20🧵
https://twitter.com/CPita3/status/1415143764461559810
There has been a multi-day debate occurring amongst @AntibioticDoc and many engineers and Aerosol scientists, regarding whether there is sufficient evidence to use HEPA filters to mitigate against Airborne Transmission of SARS2.
Here's the latest:
2/20
Here's the latest:
2/20
https://twitter.com/AntibioticDoc/status/1416443248021671939?s=20
First, HEPA filters work.
Both the @CDCgov and @WHO acknowledge that SARS2 is transmitted via BOTH short and long range *Inhalation of virus containing Aerosols*.
We know HEPAs remove those aerosols from the air, so they can't be inhaled.
3/20



Both the @CDCgov and @WHO acknowledge that SARS2 is transmitted via BOTH short and long range *Inhalation of virus containing Aerosols*.
We know HEPAs remove those aerosols from the air, so they can't be inhaled.
3/20
https://twitter.com/HuffmanLabDU/status/1359893167105970178?s=20



.@DavidElfstrom points out, the professional bodies overseeing HVAC, filtering, IAQ (even for hospitals!), are the local engineering regulatory bodies + ASHRAE.
@ashraenews, @APEGA_AB have both been unequivocal re. Airborne Transmission & filtration.
4/20

@ashraenews, @APEGA_AB have both been unequivocal re. Airborne Transmission & filtration.
4/20
https://twitter.com/DavidElfstrom/status/1414645718124535818?s=20

However, it is evident from the following tweets, that @AntibioticDoc, the Co-Chair of the @AHS_media Scientific Advisory Group, doesn't think there's enough evidence to justify the cost of HEPA filters in schools.
5/20



5/20
https://twitter.com/AntibioticDoc/status/1416590830718963715?s=20
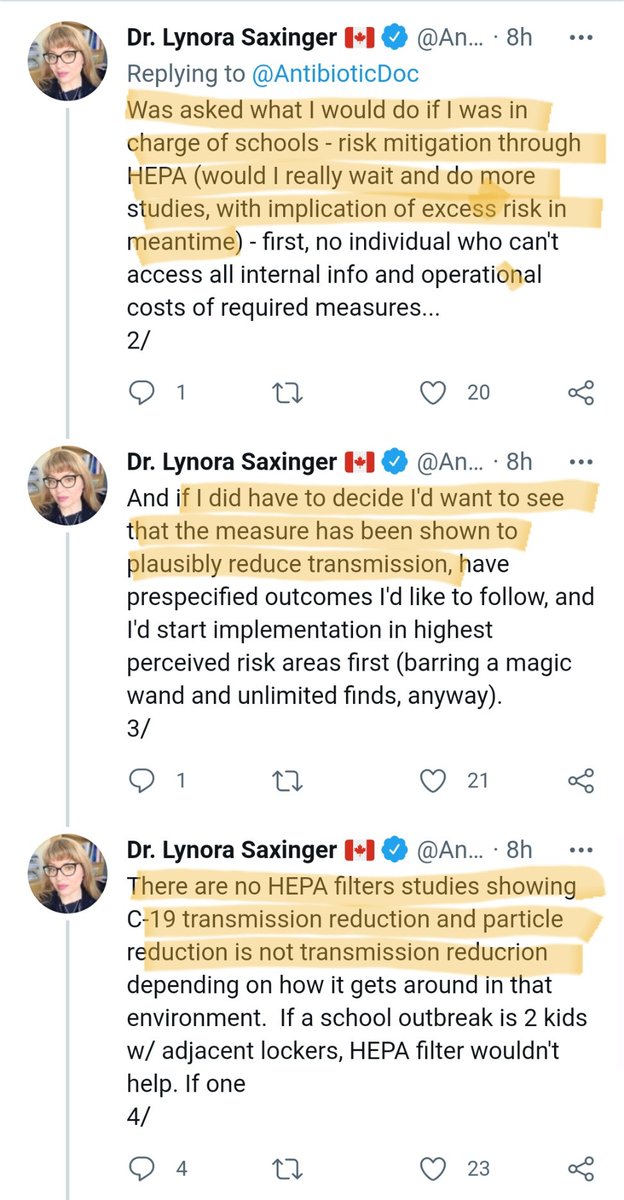


The last tweet is stunning.
"Just because there's evidence of Airborne Transmission, doesn't mean we should mitigate against it during vaccine rollout"
"Just because there's evidence of Airborne, doesn't mean HEPAs are the answer for schools"
6/20
"Just because there's evidence of Airborne Transmission, doesn't mean we should mitigate against it during vaccine rollout"
"Just because there's evidence of Airborne, doesn't mean HEPAs are the answer for schools"
6/20

Ok - "So What? Who cares what an Alberta ID thinks about this? Agree to disagree!"
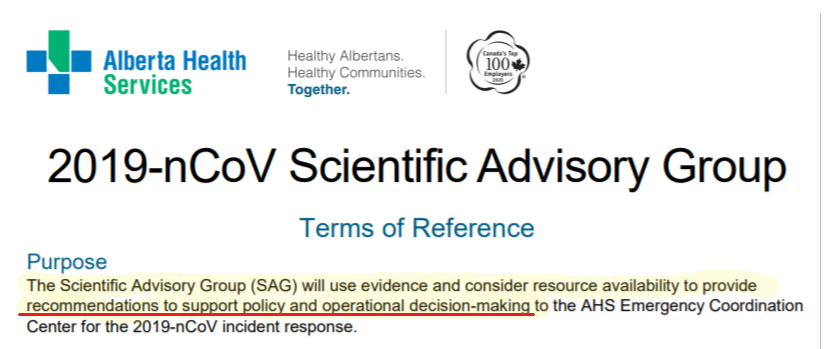
The reason so many of us care, is because @AntibioticDoc is the Co-Chair of the @AHS_media Scientific Advisory Group for SARS2.
Read this document to understand the influence of this group.
7/20
The reason so many of us care, is because @AntibioticDoc is the Co-Chair of the @AHS_media Scientific Advisory Group for SARS2.
Read this document to understand the influence of this group.
7/20

This group reviews/summarizes the evidence, and then provides policy/guidance documents and recommendations to Alberta Health for "operational decision-making".
They are quite literally the scientific gatekeepers for Alberta re. SARS2 policy.
8/20

They are quite literally the scientific gatekeepers for Alberta re. SARS2 policy.
8/20

So it's quite notable that the Co-Chair of this group is stating their isn't sufficient evidence to justify the purchase of HEPA filters in schools.
The main concern, appears to be regarding introduction of "air currents" caused by the filtered air outflow from the HEPA.
9/20
The main concern, appears to be regarding introduction of "air currents" caused by the filtered air outflow from the HEPA.
9/20

This is a common fear from ID docs, which is steeped in #DropletDogma, and ignorant of fluid dynamics.
The belief is that SARS2 is spread by droplets, which would naturally stay close to a person, unless a HEPA filter or fan is introduced, then it would blow them around.
10/20
The belief is that SARS2 is spread by droplets, which would naturally stay close to a person, unless a HEPA filter or fan is introduced, then it would blow them around.
10/20
First, Aerosols will naturally and randomly disperse throughout a room, without any external fan.
Without adequate ventilation and filtration, the infectious aerosols will build-up in the room like a cloud of smoke.
11/20
Without adequate ventilation and filtration, the infectious aerosols will build-up in the room like a cloud of smoke.
11/20

Second, I fail to see how natural ventilation (opening windows and doors) is better for this perceived harm, than a HEPA.
Natural ventilation will also induce air currents - but they will be much more unpredictable. Will depend on window installation, Delta T, and wind.
12/20
Natural ventilation will also induce air currents - but they will be much more unpredictable. Will depend on window installation, Delta T, and wind.
12/20
By this logic, the safest place, would be a perfectly sealed room, with no mechanical ventilation, fans or open windows. All the droplets would magically drop to the floor.
This is wrong - dangerously so. This would result in a hotbox of COVID aerosols. Think smoke.
13/20
This is wrong - dangerously so. This would result in a hotbox of COVID aerosols. Think smoke.
13/20

HEPAs have an intake for the infectious air, and an exhaust for the clean air (most exhaust straight up). The flow patterns are predictable, and can be considered when installed by professionals. The same is not true with windows- you don't know which way the air will flow.
14/20
14/20
The other concern that's been raised is cost.
@CorsIAQ has done the math - they are cheap, and have advantages far beyond mitigation of SARS2 transmission.
They are certainly cheaper than retrofitting entire HVAC systems.
15/20

@CorsIAQ has done the math - they are cheap, and have advantages far beyond mitigation of SARS2 transmission.
They are certainly cheaper than retrofitting entire HVAC systems.
15/20
https://twitter.com/CorsIAQ/status/1416295154755854338?s=20

Alberta can afford to install HEPA filters in every classroom. The Federal Government transferred $250 Million to Alberta, for the purposes of supporting a safe return to school. This is what that money was for.
16/20
alberta.ca/covid-19-guida…
16/20
alberta.ca/covid-19-guida…

How has that $250 Million been spent to date?
Nobody seems to know. But if the current Alberta School Safety measures are any indication, probably a whole lotta Hygiene Theatre.
17/20
Nobody seems to know. But if the current Alberta School Safety measures are any indication, probably a whole lotta Hygiene Theatre.
17/20

In summary, Alberta has $250M to facilitate a safe return to school in Sept. The chance they will spend any of that on Airborne Mitigations, like HEPA filters, is slim to none, given that the Scientific Advisory Group states there isn’t enough evidence to justify the cost.
18/20
18/20
This is a pretty distressing situation for Alberta. The emperor has no clothes.
Talk to your local schools/school boards directly. Point them to mechanical engineering/HVAC experts like @marwa_zaatari.
Ask them to #UnleashTheEngineers
19/20
Talk to your local schools/school boards directly. Point them to mechanical engineering/HVAC experts like @marwa_zaatari.
Ask them to #UnleashTheEngineers
19/20
https://twitter.com/marwa_zaatari/status/1351279531806621696?s=20
Here's a guide from @masks4canada re. selecting, sizing and installing HEPA filters.
When in doubt, consult the experts - there is an abundance of people trained in HVAC, Occ Hygiene, Indoor Air Quality and Aerosols.
We need to listen to them.
20/20
When in doubt, consult the experts - there is an abundance of people trained in HVAC, Occ Hygiene, Indoor Air Quality and Aerosols.
We need to listen to them.
20/20
https://twitter.com/KashPrime/status/1400086561987956738?s=20
Exhbit A for why this is a HUGE problem:
https://twitter.com/ClarissaC2/status/1416888587388215298?s=19
• • •
Missing some Tweet in this thread? You can try to
force a refresh






