Reflections on a cricothyrotomy:
I wanted to share my personal first experience performing this high-acuity and rare procedure, in the hopes that others will learn from it.
Consider this part reflection, part tweetorial
upload.wikimedia.org/wikipedia/comm…
I wanted to share my personal first experience performing this high-acuity and rare procedure, in the hopes that others will learn from it.
Consider this part reflection, part tweetorial
upload.wikimedia.org/wikipedia/comm…

A team member called me to say “We need you at the bedside NOW”, without further details, but with a higher sense of urgency than I’m used to from this person, so I ran to the bedside.
In fact, shortly after arriving my watch asked me if I was starting to exercise
In fact, shortly after arriving my watch asked me if I was starting to exercise
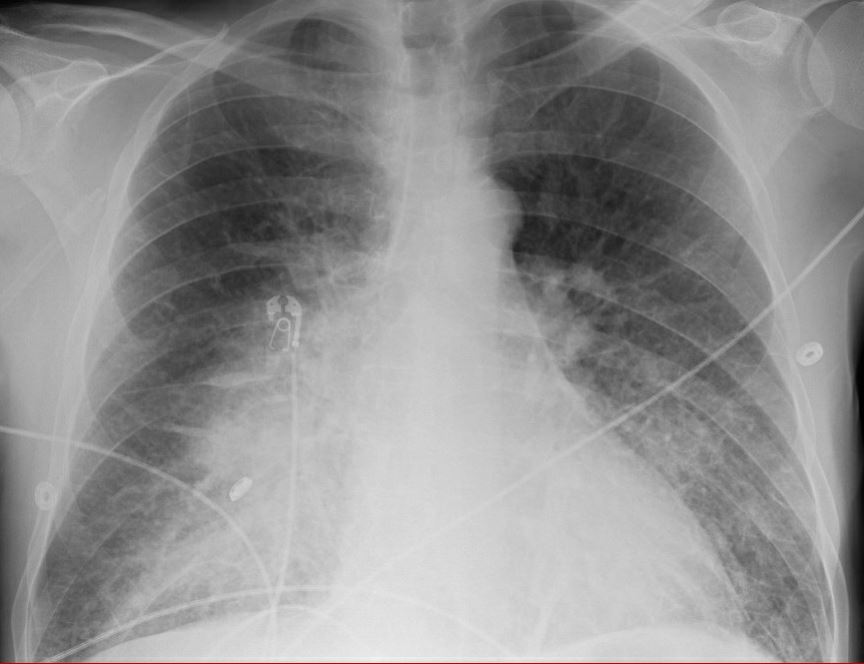
Intentionally obfuscating details about the patient, suffice it to say there was a major arterial bleed into the oropharynx which developed without warning and lead to prompt cardiac arrest.
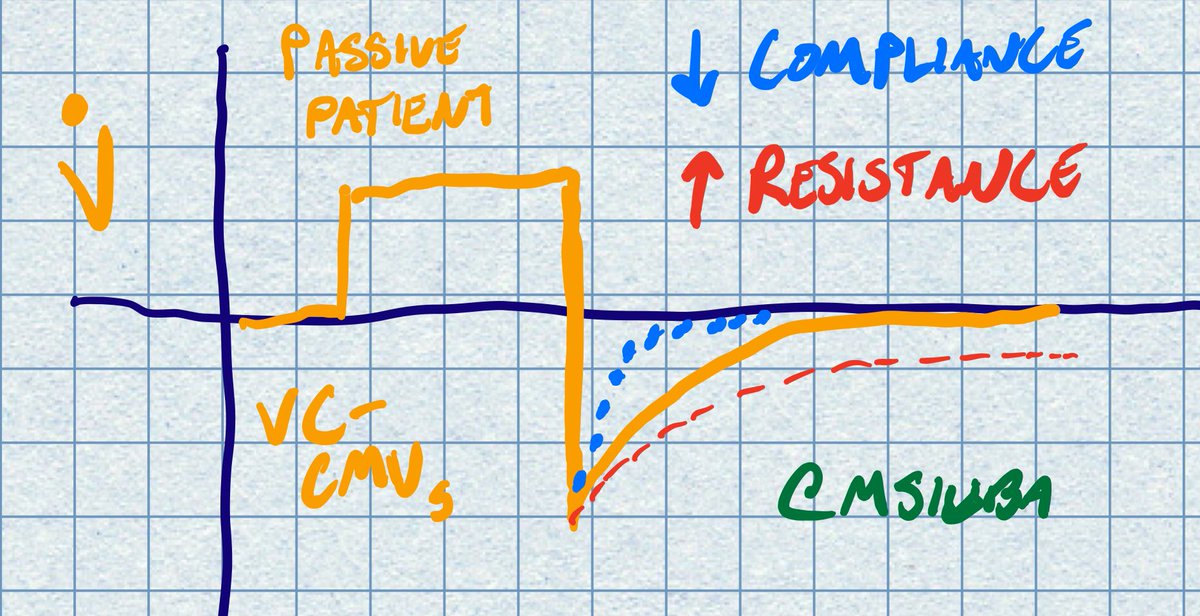
Fellow quickly prepped to intubate while CPR was ongoing. Due to neck stiffness, DL was not possible, and VL was attempted.
Given the bleeding, we applied liberal suctioning and stayed “high and dry” with the blade so it did not become soiled.
More here: criticalcarenow.com/hyperangulated…
Given the bleeding, we applied liberal suctioning and stayed “high and dry” with the blade so it did not become soiled.
More here: criticalcarenow.com/hyperangulated…
It was frankly impossible to identify any anatomy. While blood could be suctioned to relative clearing of the airway, there were clots etc which obscured identification of even the epiglottis.
A second attempt was planned, at which point I asked for the cric kit
A second attempt was planned, at which point I asked for the cric kit
Thanks to prior mental rehearsal (in past situations), I was mentally prepared to cut if needed. I had a moment to gather myself, slow my breathing and get out of “exercise” mode on my watch.
During the 2nd attempt, no improvement in view was made.
During the 2nd attempt, no improvement in view was made.
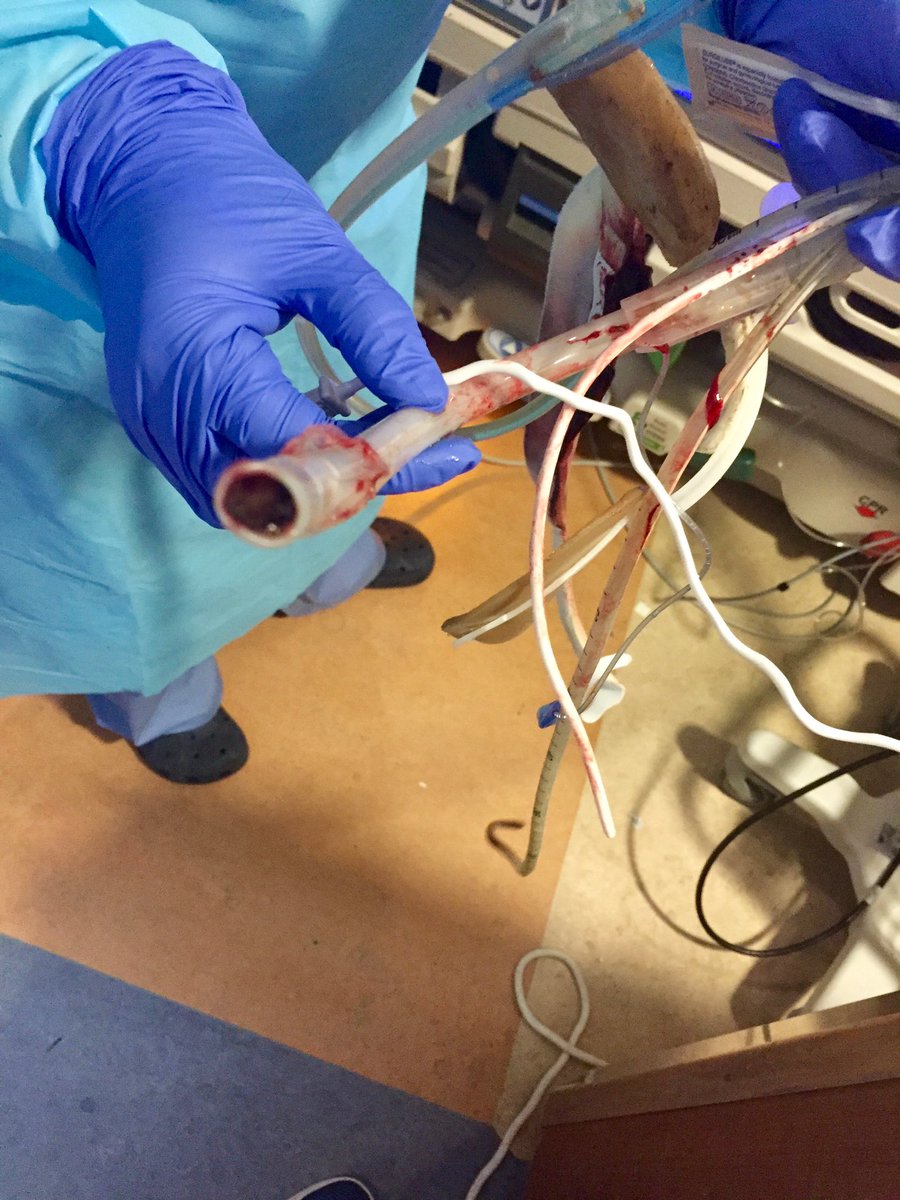
The neck was prepped, and I gathered a 10 blade, bougie, and 6.0 ETT alongside the patient’s right (I’m RHD). One more look into airway by diff airway team, no luck.
I performed the procedure near exactly the same as in this video from #AIMEairway
I performed the procedure near exactly the same as in this video from #AIMEairway
Retrospectively, the ‘hard’ parts (decision to cut, identifying the anatomy, making the right incision) were easier. Bougie glid in easily.
Unanticipated difficulty was passing ETT. I don’t think I made the initial incision into the CTM wide enough. Had to overcome high resist
Unanticipated difficulty was passing ETT. I don’t think I made the initial incision into the CTM wide enough. Had to overcome high resist
For reference, see again this video around the 24 sec mark, and how wide she makes the CTM incision after the twist
I’m quite sure I was holding my breath while waiting for the ETCO2 to register confirmation, but it finally did.
In a sad case of “successful procedure, poor outcome”, hemostasis could not be achieved.
In a sad case of “successful procedure, poor outcome”, hemostasis could not be achieved.
My learning points from this case: 1/x
- Again, dilating the CTM sufficiently wide would have made tube passage easier, a lesson for the next time
- Again, dilating the CTM sufficiently wide would have made tube passage easier, a lesson for the next time
2/
- It’s difficult to gauge appropriate tube depth when you’re down so low. In the future I might opt for a tracheostomy tube instead to ensure proper depth, and also make it easier to secure
- It’s difficult to gauge appropriate tube depth when you’re down so low. In the future I might opt for a tracheostomy tube instead to ensure proper depth, and also make it easier to secure
3/
- While it was easier to conclude FONA was needed in this case, I’m glad I didn’t delay
- A few sessions of simulation followed by hundreds (thousands?) of mental rehearsals set me up for success
- Next time this is needed, I won’t hesitate
- While it was easier to conclude FONA was needed in this case, I’m glad I didn’t delay
- A few sessions of simulation followed by hundreds (thousands?) of mental rehearsals set me up for success
- Next time this is needed, I won’t hesitate
4/4
- Finally, having the gumption to do this would not have been possible without all the #FOAMed on the topic I’ve read over the past decade. There’s plenty to criticize on this site, but the learning opportunities are invaluable.
Thanks for reading!
- Finally, having the gumption to do this would not have been possible without all the #FOAMed on the topic I’ve read over the past decade. There’s plenty to criticize on this site, but the learning opportunities are invaluable.
Thanks for reading!
• • •
Missing some Tweet in this thread? You can try to
force a refresh