The #COVBARRIER RCT now published @LancetRespirMed & it looks like we have a new COVID tx: Baricitinib
-n=1525 hospitalized COVID pts not on IMV
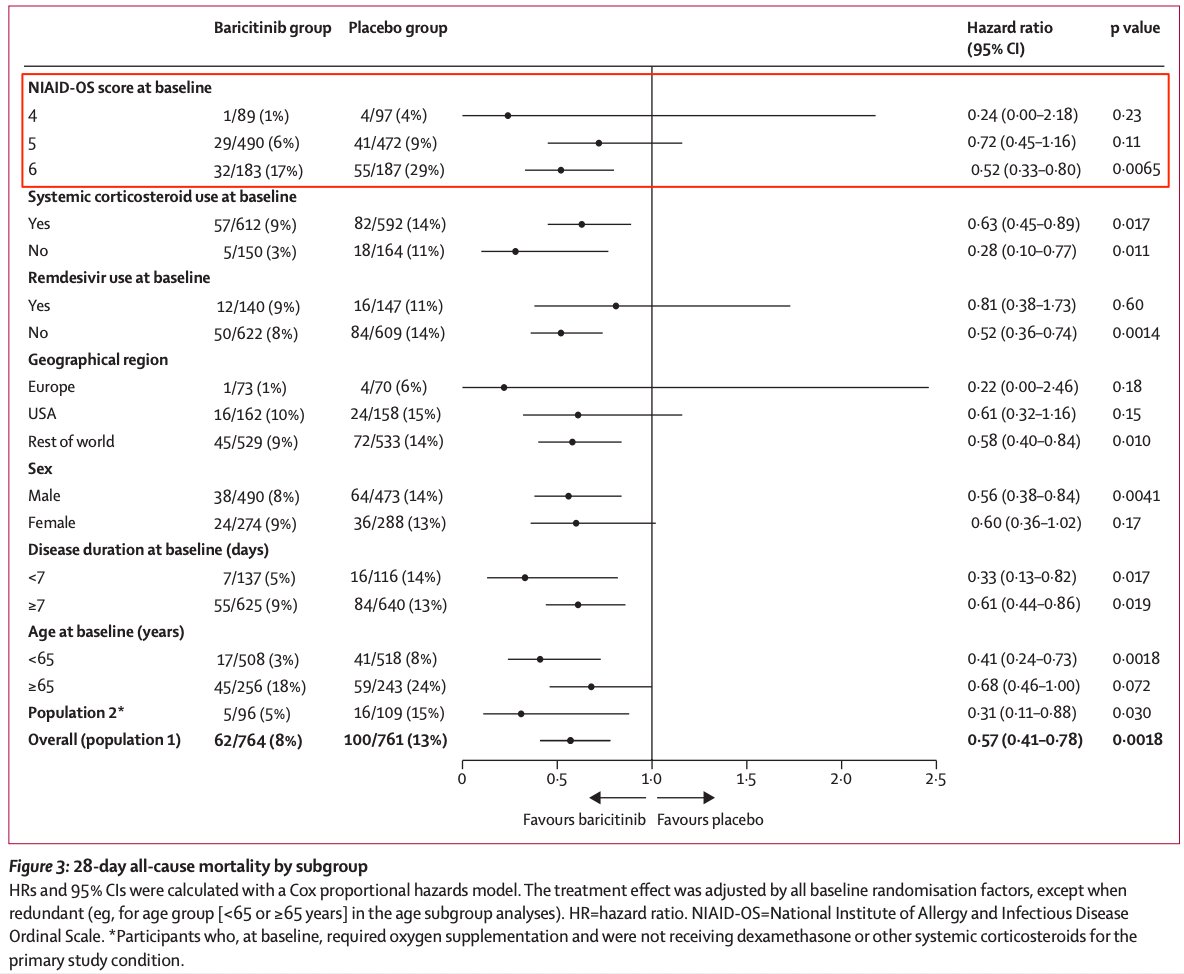
-lower mortality w/ Bari compared to placebo (10% vs 15%) (NNT = 20) & larger benefit in sicker pts!
-bit.ly/3yDmJ9r
1/



-n=1525 hospitalized COVID pts not on IMV
-lower mortality w/ Bari compared to placebo (10% vs 15%) (NNT = 20) & larger benefit in sicker pts!
-bit.ly/3yDmJ9r
1/



COV-BARRIER was a 101 site, double blind RCT performed in 11 countries.
It enrolled hospitalized COVID patients who were hypoxemic (but not on IMV) and had evidence of inflammation.
It had many exclusion criteria including monoclonals, immunesuppression. This is a🔑 point.
2/

It enrolled hospitalized COVID patients who were hypoxemic (but not on IMV) and had evidence of inflammation.
It had many exclusion criteria including monoclonals, immunesuppression. This is a🔑 point.
2/


The intervention was 4mg of baricitinib, an orally available JAK1/2 inhibitor, dosed once daily for 14 days or until hospital d/c. (It can be crushed and given by FT).
Bari is an FDA approved treatment for RA. It costs ~$50-75 per pill (thus a 14 day course is ~$700-1000).
3/
Bari is an FDA approved treatment for RA. It costs ~$50-75 per pill (thus a 14 day course is ~$700-1000).
3/

The studies primary endpoint was a composite of progression to HFNC, NIPPV, IMV, ECMO, or death.
Mortality (both 28 and 60 day) was a secondary endpoint.
They had pre-planned subgroup analyses by illness severity, age (>65 vs <65) and by concomitant meds (steroids).
4/
Mortality (both 28 and 60 day) was a secondary endpoint.
They had pre-planned subgroup analyses by illness severity, age (>65 vs <65) and by concomitant meds (steroids).
4/
Like many COVID RCTs the initial assumptions used in their power calculations were a bit off.
They initially powered for 400 people but increased to 1400; this probably reflects improvements in tx (widespread use of steroids). A common issue with COVID RCTs & a good problem..
5/
They initially powered for 400 people but increased to 1400; this probably reflects improvements in tx (widespread use of steroids). A common issue with COVID RCTs & a good problem..
5/
The study enrolled 1525 people: n=764 to Bari, n=761 to placebo
The patients were slightly younger (2/3 under 65 yo) but otherwise fairly typical of those hospitalized w/ COVID.
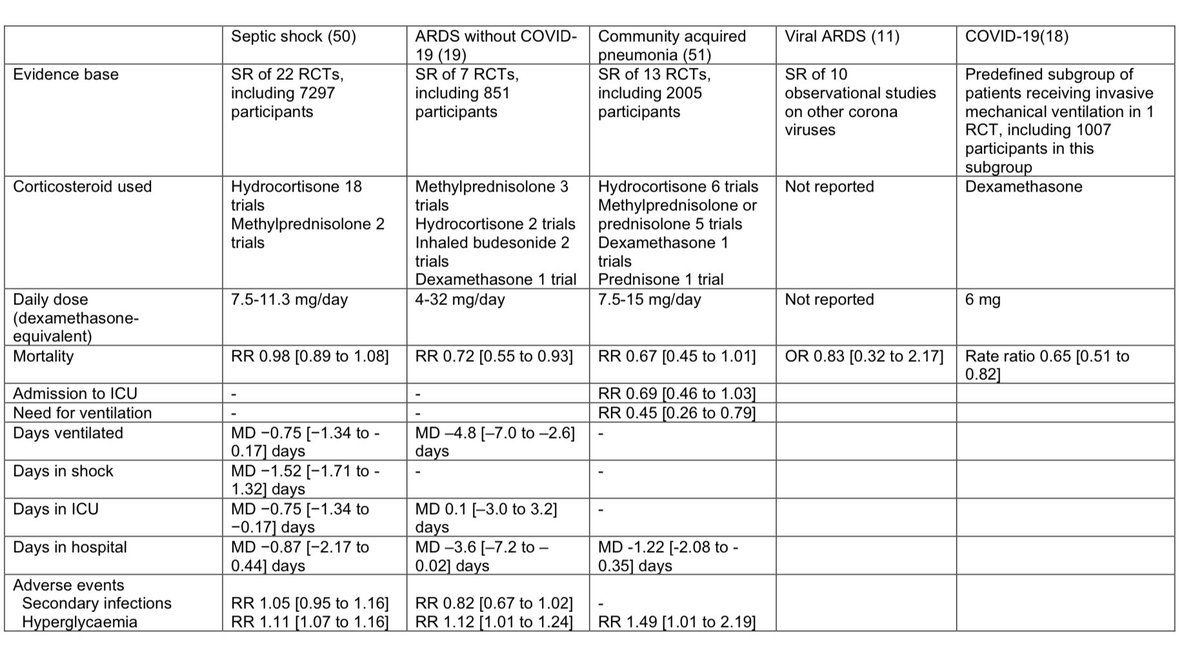
Most patients (>90%) were treated with dexamethasone. Only a minority received remdesivir (<20%).
6/


The patients were slightly younger (2/3 under 65 yo) but otherwise fairly typical of those hospitalized w/ COVID.
Most patients (>90%) were treated with dexamethasone. Only a minority received remdesivir (<20%).
6/



The results were... interesting
There was a large & significant reduction in mortality 🟥 (a secondary endpoint) but no difference in the primary composite endpoint 🟨 or in other secondary endpoints like ventilator free days or hospital LOS 🟩.
What do we make of this?
7/

There was a large & significant reduction in mortality 🟥 (a secondary endpoint) but no difference in the primary composite endpoint 🟨 or in other secondary endpoints like ventilator free days or hospital LOS 🟩.
What do we make of this?
7/


The issue with composite endpoints is that both requiring HFNC and dying are treated the same as events, despite the fact that is vastly preferable to have HFNC.
We've seen this issue before in other COVID studies.
One remedy is to use "win ratio"
8/
We've seen this issue before in other COVID studies.
One remedy is to use "win ratio"
https://twitter.com/nickmmark/status/1402124767432372224?s=20
8/
Remember that mortality is a "hard" endpoint even if 2° Composite endpoints are often 1° because the PI didn't think they could power to detect a mortality Δ
My friend @WesElyMD (who happens to be the study PI) explains this in a GREAT 🧵(go read it!)
9/
My friend @WesElyMD (who happens to be the study PI) explains this in a GREAT 🧵(go read it!)
https://twitter.com/WesElyMD/status/1433084748835049478?s=20
9/
In terms of safety, the rate of AEs and SAEs was similar or *lower* in the intervention compared to placebo.
Despite concerns about immunosuppression there were fewer infxns with Bari. There was also no increase in VTEs (another JAKi tofacitinib has a black box warning)
10/

Despite concerns about immunosuppression there were fewer infxns with Bari. There was also no increase in VTEs (another JAKi tofacitinib has a black box warning)
10/


My clinical 🥡:
- In hospitalized COVID pts on O2, Baricitinib 4mg daily improves survival (in addition to steroids)
- Bari appears safe & well tolerated at this dose
- Its cheaper and more widely available than Toci (there's a Toci shortage)
- I use Bari to treat my pts
11/11
- In hospitalized COVID pts on O2, Baricitinib 4mg daily improves survival (in addition to steroids)
- Bari appears safe & well tolerated at this dose
- Its cheaper and more widely available than Toci (there's a Toci shortage)
- I use Bari to treat my pts
11/11
Also thanks to the eagle eyed folks who caught a math error in my first tweet.
I deleted the tweet (and reposted with correct NNT) because there’s no edit functionality & I didn’t want to cause confusion. Thanks!
I deleted the tweet (and reposted with correct NNT) because there’s no edit functionality & I didn’t want to cause confusion. Thanks!
• • •
Missing some Tweet in this thread? You can try to
force a refresh