What is driving current peaks in SARS-CoV-2 cases & what does this mean for the fall & winter?
Although a peak might seem to indicate that we're headed for fewer cases until a new variant arises, unfortunately that's not the case & a surge is both likely & avoidable.
A thread.
Although a peak might seem to indicate that we're headed for fewer cases until a new variant arises, unfortunately that's not the case & a surge is both likely & avoidable.
A thread.

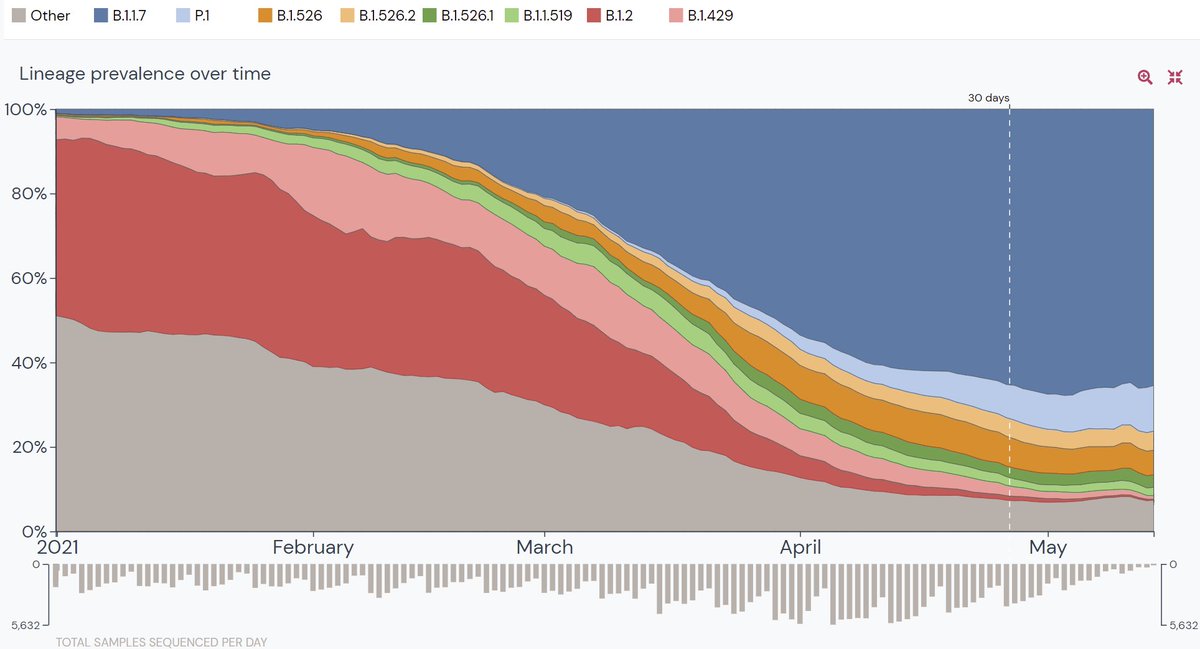
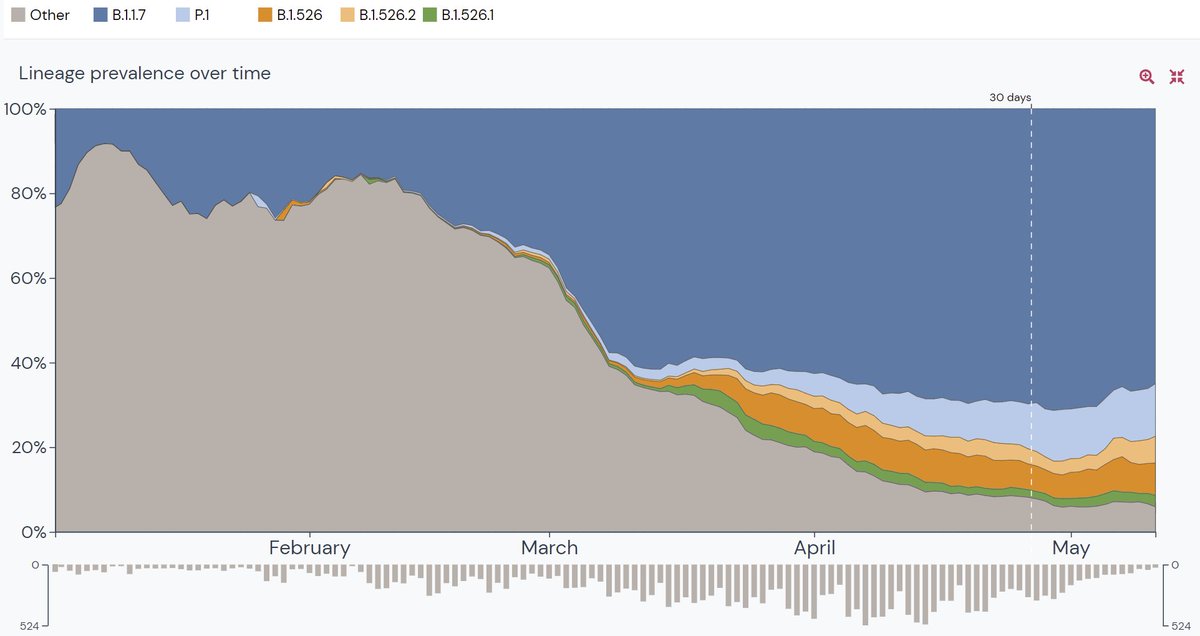
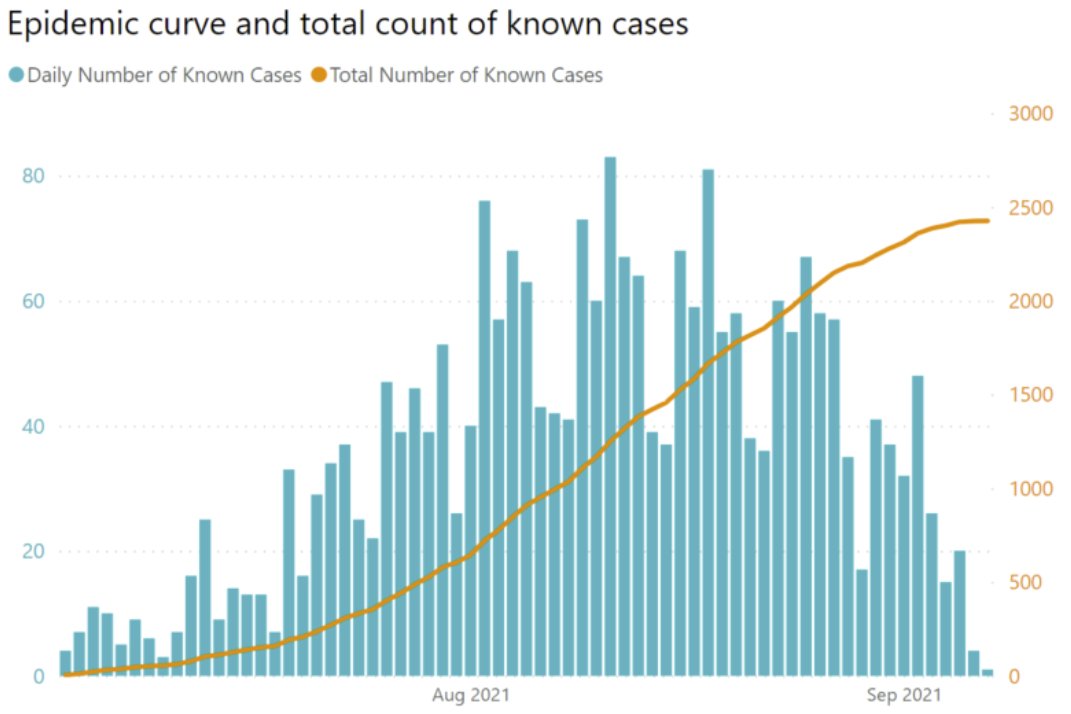
One possibility is in nice thread @trvrb suggesting US Delta surge is peaking now b/c 5% more of US pop infected, driving Rt down to 1 (which occurs at peak).
https://twitter.com/trvrb/status/1435249759766212610
However, as @trvrb notes in addendum (
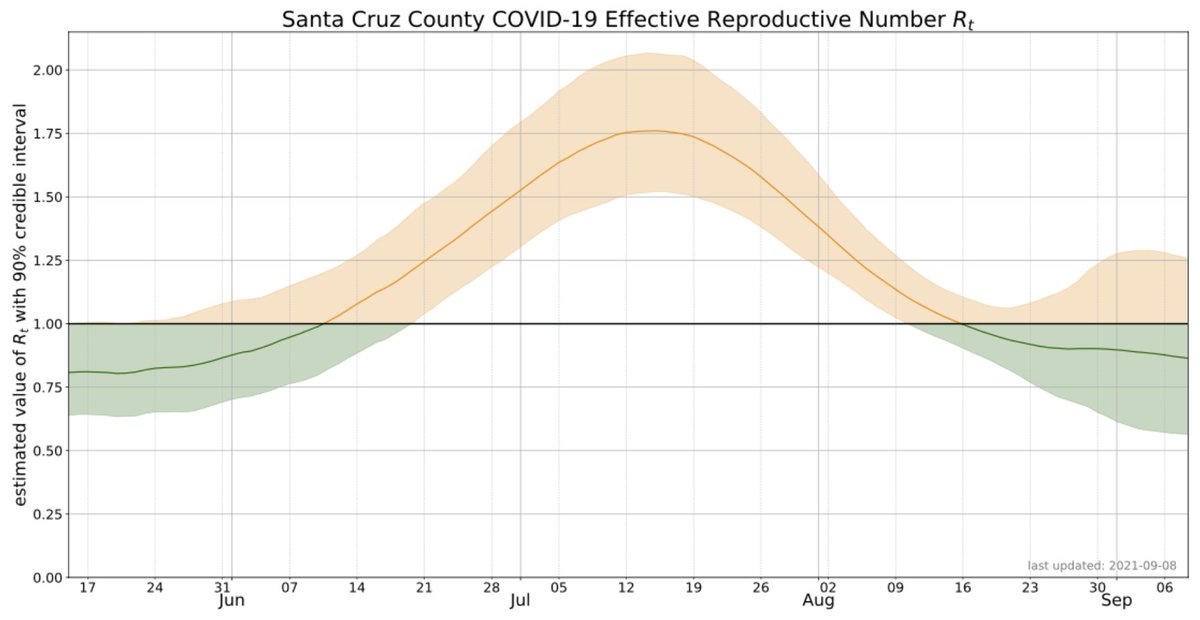
https://twitter.com/trvrb/status/1435267529325248517), Rt at peak is 1 b/c of combination of behavior (which drives R0) and fraction susceptible (Rt = R0*S/N).
Here's the challenge: in most social networks (the appropriate unit for transmission) we're not at herd immunity threshold (HIT) even when we combine vaccination + immunity from infection. How do I know we're not near HIT and what does that mean for Fall/Winter?
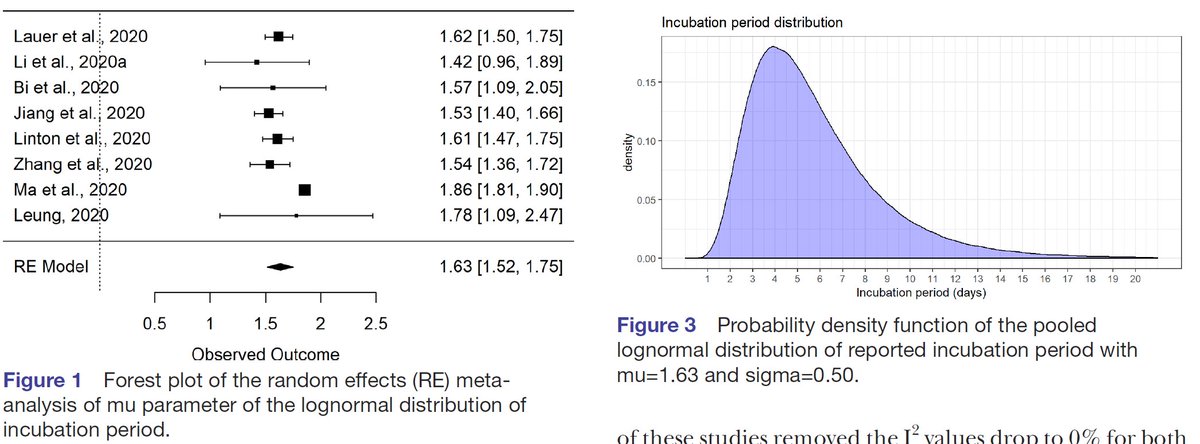
I know we're not near HIT b/c rise in cases July/Aug was too fast (e.g. local CA data suggest Rt =1.75) santacruzhealth.org/HSAHome/HSADiv…). To get Rt to 0.9, we'd need ~50% of remaining susceptibles to be infected & surge clearly was too small for that. 

More generally, as most now, know HIT = 1-1/R0. R0 for delta with 2019 behavior is likely 5-9. If we use R0=7, HIT = 86%. Although some social networks might have immunity this high due to vaccination or infection, protection vs. infection & transmission isn't 100% from either.
I'm not aware of rigorous estimates of protection vs. infection & transmission for Delta for vaccination & previous non-Delta infection (please link if they exist), but crude estimates suggest that protection might be as low as ~60% (
https://twitter.com/DiseaseEcology/status/1425492401271894018) & are unlikely >80%.
If we use an optimistic 70%, then Rt w/ 2019 behavior & w/ 100% (!) of people with immunity would be:
Rt = (1-100%*0.7)*7 = 2.1
This means that to get Rt below 1 we need avoid 2019 behavior or we need super-immunity (e.g. vaccination + infection) or some combination.
Rt = (1-100%*0.7)*7 = 2.1
This means that to get Rt below 1 we need avoid 2019 behavior or we need super-immunity (e.g. vaccination + infection) or some combination.
This is why epidemiologists have been saying that we can no longer reach HIT just by vaccination. It means we need either behavioral changes to reduce contact rates or immunity that provides protection higher than vaccines or previous infection w/ non-Delta variant.
For Fall/Winter 2021-2, if we increase risky contacts back towards 2019 levels (as we did in 2020), infections will surge again until enough people have more protective immunity. Put another way, Rt may be <1 now but that's only b/c some are still not partying like its 2019.
We can avoid a fall surge by reducing Rt in 3 ways:
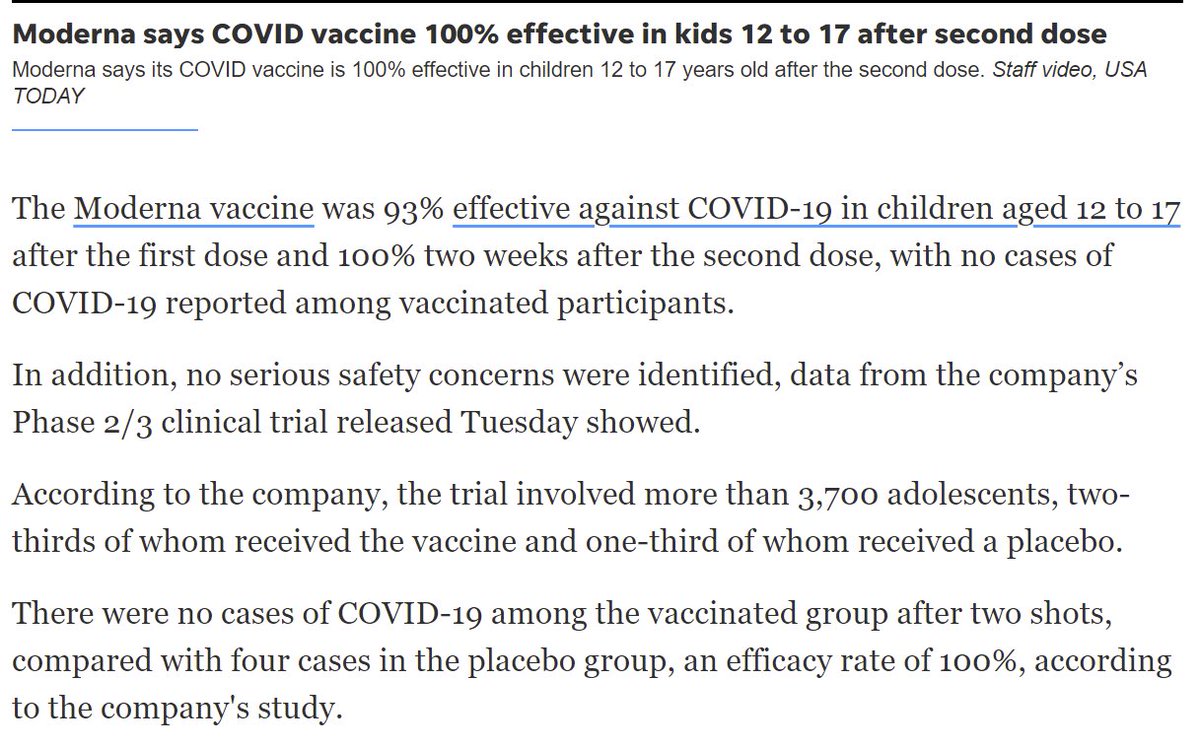
1) vaccinate the unvaccinated
2) keep risky contacts low (e.g. masks; many US states & countries are using masks to reduce Rt)
3) vaccine boosters (yes, I know that, morally, doses should instead be given to developing nations)
1) vaccinate the unvaccinated
2) keep risky contacts low (e.g. masks; many US states & countries are using masks to reduce Rt)
3) vaccine boosters (yes, I know that, morally, doses should instead be given to developing nations)
None of these are easy.
-We've been trying to vaccinate the unvaccinated w/ lotteries, $$, mandates, etc.
-Folks are tired of masks, social distancing
-Boosting 150M+ people in US would use 150M doses needed by developing nations & would be hard
-We've been trying to vaccinate the unvaccinated w/ lotteries, $$, mandates, etc.
-Folks are tired of masks, social distancing
-Boosting 150M+ people in US would use 150M doses needed by developing nations & would be hard
Thus, I bet we'll have a fall/winter surge even w/out a new virus variant (but thankfully there'll be far fewer deaths/hospitalizations/long-covid due to vaccination), but the timing and size of the surge is very tough to predict because it depends on HUMAN BEHAVIOR.
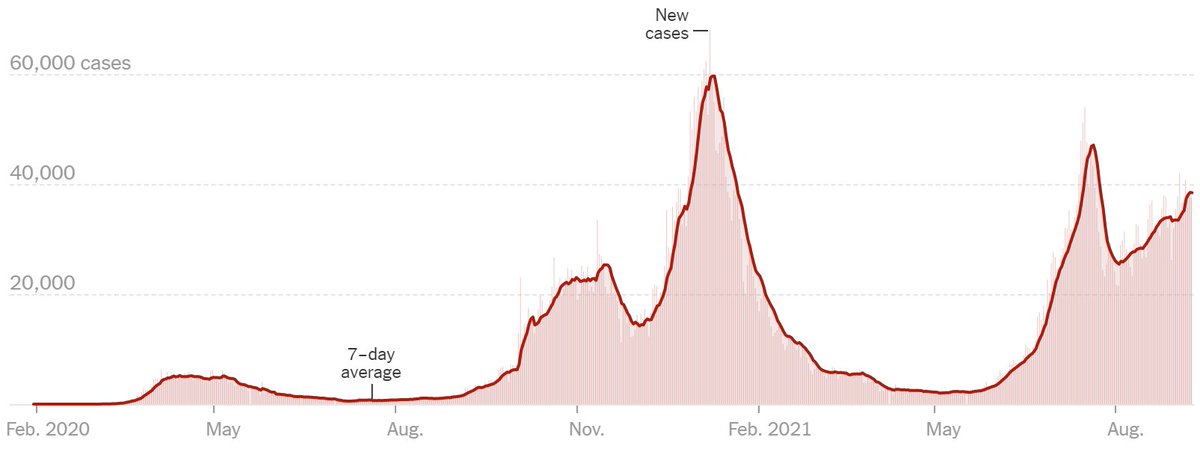
IMO, human behavior has been the hardest thing to understand/predict during the pandemic. Many surges in 2020-1 have stopped long before reaching HIT, due to changes in human behavior. (exhibit A: Fig of UK Covid cases) 
Given the variability in transmission among people and settings, a shift in behavior by a small fraction of any population can have a big impact in reducing/increasing Rt (take all predictions with a giant grain of salt!).
So please, get vaccinated if you haven't yet, be a little safer than you otherwise would be until we get ample vaccine supply, and when we do get boosted (hopefully w/ an updated vaccine)!
• • •
Missing some Tweet in this thread? You can try to
force a refresh