Preliminary data from ERAS are out… looks like another record-setting year.
The average number of applications received by residency programs is up in most specialties - in some cases, by 30-40% versus 2019.
#ApplicationFever
The average number of applications received by residency programs is up in most specialties - in some cases, by 30-40% versus 2019.
#ApplicationFever

The average number of applications submitted by applicants is up, too.
Here are the current averages for each specialty (considering all applicant types - MDs, DOs, and IMGs).
Here are the current averages for each specialty (considering all applicant types - MDs, DOs, and IMGs).

MD applicants in dermatology, otolaryngology, urology, and neurosurgery now submit a mean of around 80 applications or more - and the average MD applicant in orthopedics submits nearly 100 applications. 

And here are the data for DO applicants.
In most specialties, DOs submit more applications than their MD peers. (The exceptions are a few highly competitive specialties, in which there are still programs that do not seriously consider DO applicants).
In most specialties, DOs submit more applications than their MD peers. (The exceptions are a few highly competitive specialties, in which there are still programs that do not seriously consider DO applicants).

As a reminder, the figures above show only the average *within that specialty.*
But these days, many applicants apply to more than one specialty… so the total number of applications submitted by each applicant is even higher than the figures above would suggest.
But these days, many applicants apply to more than one specialty… so the total number of applications submitted by each applicant is even higher than the figures above would suggest.
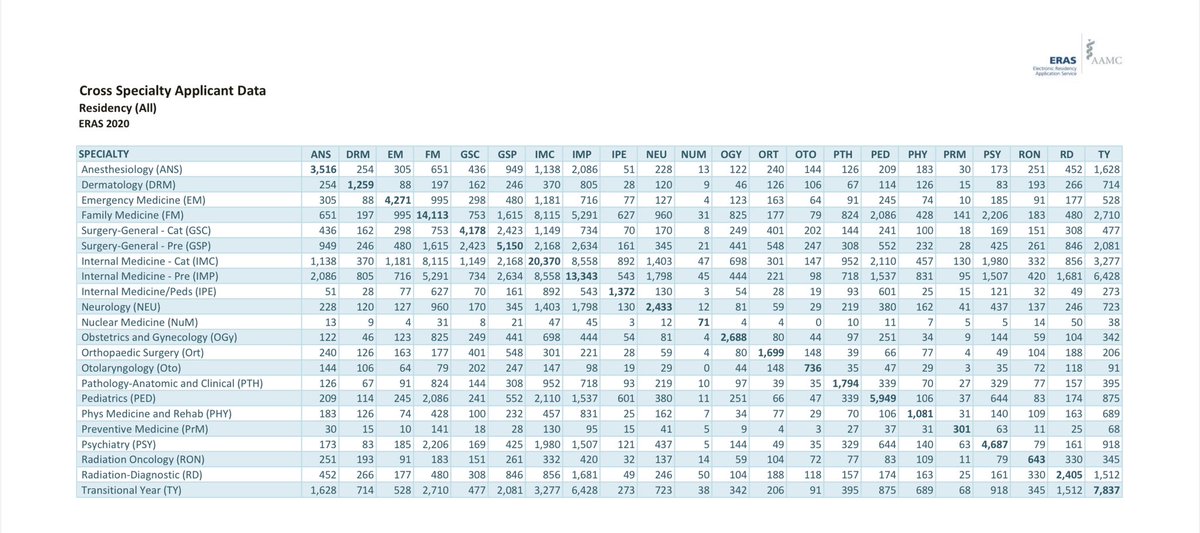
Here are the 2020 ERAS cross-specialty applicant data, which show the extent of multiple-specialty application.
e.g., 148 applicants applied to both ortho and otolaryngology programs; 126 applied in both derm and PM&R; 169 applied in both psychiatry and general surgery; etc.
e.g., 148 applicants applied to both ortho and otolaryngology programs; 126 applied in both derm and PM&R; 169 applied in both psychiatry and general surgery; etc.
Here’s how the average number of applications submitted has grown over time - doubling in little over a decade.
cureus.com/articles/47109…
cureus.com/articles/47109…

Think these trends are sustainable?
Me, neither.
Can I interest you in application caps?
thesheriffofsodium.com/2020/04/07/on-…
Me, neither.
Can I interest you in application caps?
thesheriffofsodium.com/2020/04/07/on-…
ADDENDUM:
Lots of questions about why I compared 2021 to 2019 (not 2020) in the first graphic.
Application numbers vary over the course of the season - but the start of the 2020 season was delayed. So to to make an apples-to-apples comparison, I went back a year.
Lots of questions about why I compared 2021 to 2019 (not 2020) in the first graphic.
Application numbers vary over the course of the season - but the start of the 2020 season was delayed. So to to make an apples-to-apples comparison, I went back a year.
Also - these aren’t my data. They’re from the AAMC, and they’re available to anyone who wants to splice them a different way.
aamc.org/data-reports/i…
aamc.org/data-reports/i…
• • •
Missing some Tweet in this thread? You can try to
force a refresh