*Hyperdynamic LV: Harbinger of Doom*
This clincial scenario has played out before my eyes on multiple occasions
Echo performed on a pt with undifferentiated shock
"EF > 70%...hyperdynamic.. all good."
A hyperdynamic LV is more sinister than you may think. Lets find out why..
This clincial scenario has played out before my eyes on multiple occasions
Echo performed on a pt with undifferentiated shock
"EF > 70%...hyperdynamic.. all good."
A hyperdynamic LV is more sinister than you may think. Lets find out why..
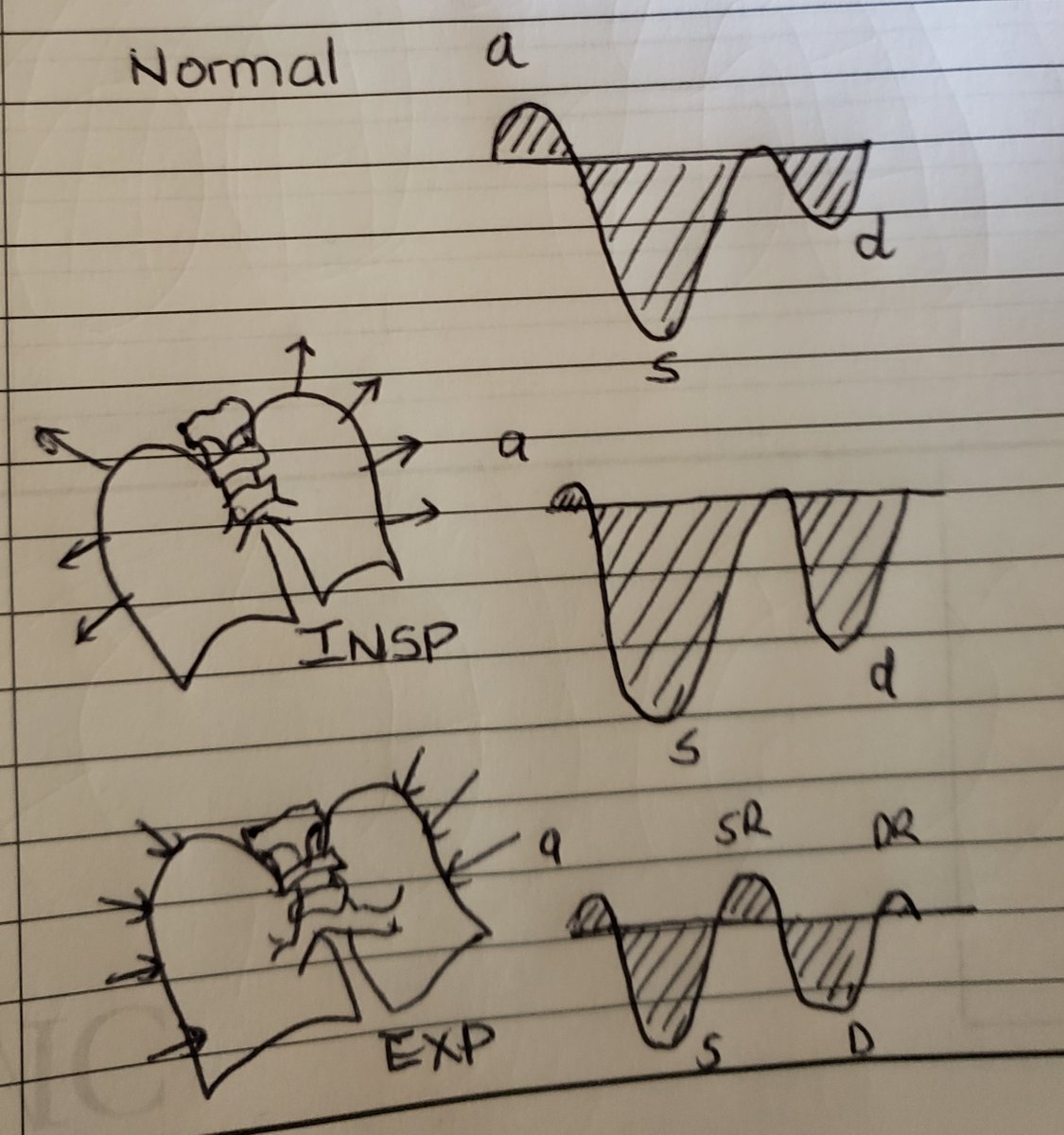
Consider why the LV would be hypercontractile and avoid the knee jerk reflex to assume that it is ONLY due to hypovolemia/hemorrhage i.e decreased RV preload/low mean systemic filling pressure . 

Start thinking in terms of LV preload.
1. RV failure
2. Mitral regurgitation
3. VSD
4. Vasodilated state
You need to actively rule out these conditions in the right clinical context.
1. RV failure
2. Mitral regurgitation
3. VSD
4. Vasodilated state
You need to actively rule out these conditions in the right clinical context.
Multiple studies in septic pts have shown worse outcomes with a hypercontractile LV. But why?
Likely,
1. Reflexive overjudicious IVFs -->organ cogestion, dysfunction and ultimate demise.
2. Reflective of profound inflamm response and vasodilation with severe infection.
Likely,
1. Reflexive overjudicious IVFs -->organ cogestion, dysfunction and ultimate demise.
2. Reflective of profound inflamm response and vasodilation with severe infection.
3. Anchor bias. We fail to rule out other causes of a hyperdynamic LV
Consider this thought experiment
1. Pt with baseline EF 30 %
2. Pt is septic and vasodilated
3. Hyperdynamic (70%) because afterload is decreased
4. As pt recovers (or vasopressors) afterload increases
5. EF will appear to worsen!
Understanding loading conditions is crucial
1. Pt with baseline EF 30 %
2. Pt is septic and vasodilated
3. Hyperdynamic (70%) because afterload is decreased
4. As pt recovers (or vasopressors) afterload increases
5. EF will appear to worsen!
Understanding loading conditions is crucial
In conclusion,
1. Hyperdynamic LV is a bad omen
2. Determine why the LV isn't "seeing" much stroke volume
3. Common causes of decreased LV preload: RV failure, MR, vasodilated states, decreased RV preload
3. EF is not the same as stroke volume. Loading conditions are crucial.
1. Hyperdynamic LV is a bad omen
2. Determine why the LV isn't "seeing" much stroke volume
3. Common causes of decreased LV preload: RV failure, MR, vasodilated states, decreased RV preload
3. EF is not the same as stroke volume. Loading conditions are crucial.
@IM_Crit_ @msiuba @NephroP @MansourKhunaizi @iceman_ex @ArgaizR @nomadic_medic @CNemehMD @ThinkingCC #FOAMed #MedTwitter #MedEd
• • •
Missing some Tweet in this thread? You can try to
force a refresh