#tweetorial 🧵
🚩Metabolism and Acute Myeloid Leukemia
(1/23)
➡️📈🔎Increased attention over the last decade on the metabolic perturbations in AML
➡️Potential therapeutic implications – with ‘druggable’ targets
🚩Metabolism and Acute Myeloid Leukemia
(1/23)
➡️📈🔎Increased attention over the last decade on the metabolic perturbations in AML
➡️Potential therapeutic implications – with ‘druggable’ targets

(2/23)
➡️🗒️📌Summary of recent concepts
🔊IT IS ALL HAPPENING IN THE MITOCHONDRIA
👉📈🏹Increase potential of targeting the mitochondria
👉🦀Anti-cancer agents specifically targeting cancer cell mitochondria are referred to as 'mitocans'
➡️🗒️📌Summary of recent concepts
🔊IT IS ALL HAPPENING IN THE MITOCHONDRIA
👉📈🏹Increase potential of targeting the mitochondria
👉🦀Anti-cancer agents specifically targeting cancer cell mitochondria are referred to as 'mitocans'
(3/23)
➡️Metabolic adaptions of AML cells
AML is a 🦀cancer derived from the myeloid lineage of blood🩸cells, characterized by overproduction of malignant cells.
➡️Metabolic adaptions of AML cells
AML is a 🦀cancer derived from the myeloid lineage of blood🩸cells, characterized by overproduction of malignant cells.

(4/23)
🧩🧩Warburg or Mitochondria respiration - Acute Myeloid leukemia❓❓
👉Many cancer cells utilize aerobic glycolysis to meet the anabolic demands of cell growth and proliferation, also known as the ‘Warburg effect"
🧩🧩Warburg or Mitochondria respiration - Acute Myeloid leukemia❓❓
👉Many cancer cells utilize aerobic glycolysis to meet the anabolic demands of cell growth and proliferation, also known as the ‘Warburg effect"

(5/23)
👉Some subsets of AML cells have been found to be disproportionately reliant on the mitochondrial function to support cell survival
👉Some subsets of AML cells have been found to be disproportionately reliant on the mitochondrial function to support cell survival

(6/23)
➡️BCL-2 inhibition🎯targets oxidative phosphorylation and selectively eradicates quiescent human leukemia stem cells.
➡️BCL-2 inhibition🎯targets oxidative phosphorylation and selectively eradicates quiescent human leukemia stem cells.

(7/23)
➡️AMPK/FIS1-Mediated Mitophagy Is Required for Self-Renewal of Human AML Stem Cells
👉Human AML LSCs display high FIS1 expression and unique mitochondrial morphology.
➡️AMPK/FIS1-Mediated Mitophagy Is Required for Self-Renewal of Human AML Stem Cells
👉Human AML LSCs display high FIS1 expression and unique mitochondrial morphology.

(8/23)
➡️Nicotinamide Metabolism Mediates Resistance to Venetoclax in🔁Relapsed Acute Myeloid Leukemia🩸Stem Cells
👉Nicotinamide metabolism is increased upon relapse in leukemia stem cells
👉🎯Targeting nicotinamide metabolism eradicates relapsed leukemia stem cells
➡️Nicotinamide Metabolism Mediates Resistance to Venetoclax in🔁Relapsed Acute Myeloid Leukemia🩸Stem Cells
👉Nicotinamide metabolism is increased upon relapse in leukemia stem cells
👉🎯Targeting nicotinamide metabolism eradicates relapsed leukemia stem cells

(9/23)
➡️🎯Targeting Glutamine Metabolism and Redox State for Leukemia Therapy 💊
👉The use of a glutaminase inhibitor (drug 1, e.g., CB-839) blocks glutamine metabolism and production of antioxidant GSH and 👇
➡️🎯Targeting Glutamine Metabolism and Redox State for Leukemia Therapy 💊
👉The use of a glutaminase inhibitor (drug 1, e.g., CB-839) blocks glutamine metabolism and production of antioxidant GSH and 👇

(10/23)
👉Makes leukemia cells vulnerable to a pro-oxidant agent (drug 2, e.g., ATO or HHT), leading to super induction of mitoROS and subsequent leukemia cell death ☠️via apoptosis.
👉Makes leukemia cells vulnerable to a pro-oxidant agent (drug 2, e.g., ATO or HHT), leading to super induction of mitoROS and subsequent leukemia cell death ☠️via apoptosis.
(11/23)
➡️Inhibition of Amino Acid Metabolism Selectively Targets🎯 Human👫Leukemia Stem Cells
👉LSCs catabolize amino acids into TCA-cycle intermediates, making LSCs⚡️highly dependent on amino acid metabolism for OXPHOS and survival
➡️Inhibition of Amino Acid Metabolism Selectively Targets🎯 Human👫Leukemia Stem Cells
👉LSCs catabolize amino acids into TCA-cycle intermediates, making LSCs⚡️highly dependent on amino acid metabolism for OXPHOS and survival

(12/23)
➡️Cysteine depletion targets leukemia stem cells through 🔽inhibition of electron transport complex II
👉Loss of SDHA glutathionylation impairs ETC II activity, thereby inhibiting oxidative phosphorylation, reducing the production of ATP, and leading to LSC death.
➡️Cysteine depletion targets leukemia stem cells through 🔽inhibition of electron transport complex II
👉Loss of SDHA glutathionylation impairs ETC II activity, thereby inhibiting oxidative phosphorylation, reducing the production of ATP, and leading to LSC death.

(13/23)
➡️Venetoclax with Azacitidine Disrupts Energy Metabolism and Targets Leukemia Stem Cells in Acute Myeloid Leukemia Patients
👉Glutathionylation, a post-translation modification, has been shown to increase ETC complex II activity.
➡️Venetoclax with Azacitidine Disrupts Energy Metabolism and Targets Leukemia Stem Cells in Acute Myeloid Leukemia Patients
👉Glutathionylation, a post-translation modification, has been shown to increase ETC complex II activity.
(14/23)
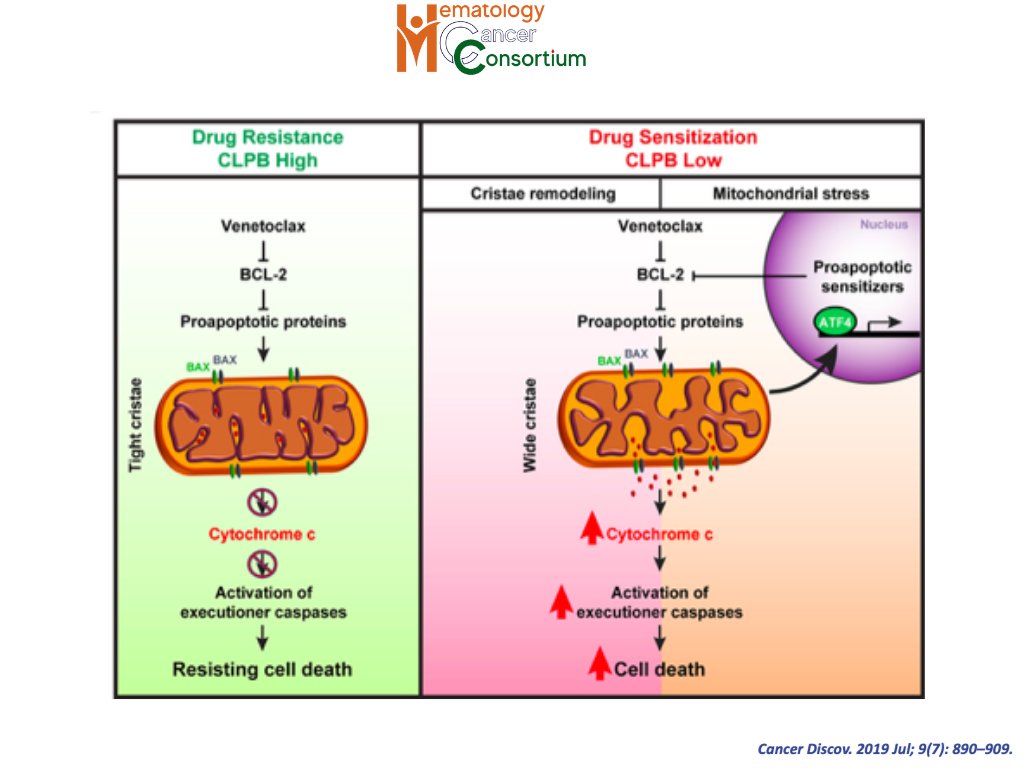
➡️Targeting mitochondrial structure sensitizes acute myeloid leukemia to Venetoclax treatment
👉🎯Targeting the mitochondrial CLPB sensitizes AML cells to Venetoclax treatment💊.
➡️Targeting mitochondrial structure sensitizes acute myeloid leukemia to Venetoclax treatment
👉🎯Targeting the mitochondrial CLPB sensitizes AML cells to Venetoclax treatment💊.
(15/23)
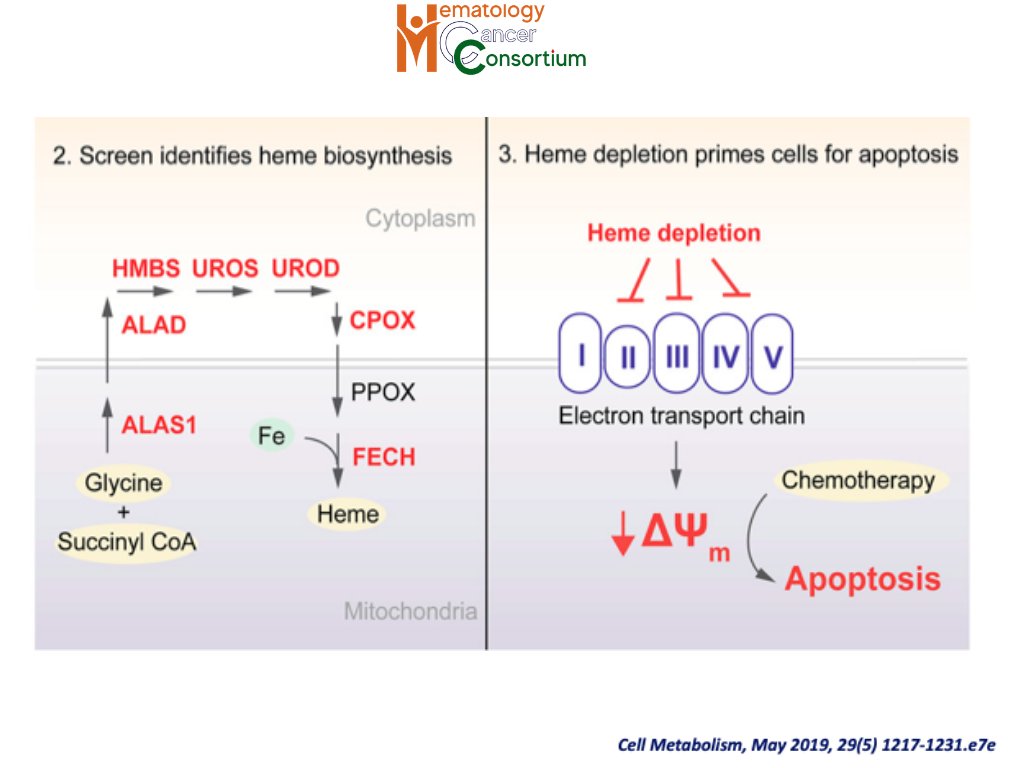
➡️Systematic Dissection of the Metabolic-Apoptotic Interface in AML🪞Reveals Heme Biosynthesis to Be a Regulator of Drug Sensitivity👇
➡️Systematic Dissection of the Metabolic-Apoptotic Interface in AML🪞Reveals Heme Biosynthesis to Be a Regulator of Drug Sensitivity👇
(16/23)
👉🔽Reduction of heme biosynthesis ⚡️potentiates apoptosis through the loss of ETC activity, resulting in baseline depolarization of the mitochondrial membrane and an 📈increased propensity to undergo apoptosis.
👉🔽Reduction of heme biosynthesis ⚡️potentiates apoptosis through the loss of ETC activity, resulting in baseline depolarization of the mitochondrial membrane and an 📈increased propensity to undergo apoptosis.
(17/23)
➡️An 🔽inhibitor of oxidative phosphorylation exploits 🦀cancer vulnerability
👉Glycolysis-deficient and AML tumour cells are sensitive to OXPHOS inhibition and 👇
➡️An 🔽inhibitor of oxidative phosphorylation exploits 🦀cancer vulnerability
👉Glycolysis-deficient and AML tumour cells are sensitive to OXPHOS inhibition and 👇

(18/23)
👉IACS-010759 (Complex-I ETC) robustly inhibited proliferation and induced apoptosis in models of brain cancer and acute myeloid leukemia (AML) reliant on OXPHOS, likely owing to a combination of energy depletion and impaired nucleotide biosynthesis.
👉IACS-010759 (Complex-I ETC) robustly inhibited proliferation and induced apoptosis in models of brain cancer and acute myeloid leukemia (AML) reliant on OXPHOS, likely owing to a combination of energy depletion and impaired nucleotide biosynthesis.
(20/23)
👉Genetic 🧬attenuation or pharmacological🔽 inhibition of VLCAD hindered mitochondrial respiration and FAO contribution to the tri-carboxylic acid cycle 🌀, resulting in 📉decreased viability, proliferation, clonogenic growth, and AML cell engraftment.
👉Genetic 🧬attenuation or pharmacological🔽 inhibition of VLCAD hindered mitochondrial respiration and FAO contribution to the tri-carboxylic acid cycle 🌀, resulting in 📉decreased viability, proliferation, clonogenic growth, and AML cell engraftment.
(21/23)
🗝️🗝️Summary
1⃣📌Substantial evidence of literature exists delineating the interaction between AML metabolism, leukemia cell survival, response to existing therapies 💊 and novel therapeutic strategies.
🗝️🗝️Summary
1⃣📌Substantial evidence of literature exists delineating the interaction between AML metabolism, leukemia cell survival, response to existing therapies 💊 and novel therapeutic strategies.
(22/23)
2⃣📌Different metabolic pathways are involved in intracellular metabolic reprogramming depending on the genetic characteristics of AML cells.
2⃣📌Different metabolic pathways are involved in intracellular metabolic reprogramming depending on the genetic characteristics of AML cells.
(23/23)
3⃣📌Metabolic pathways fuelling OXPHOS appear to be critical for AML cell survival and will potentially become therapeutic targets to improve outcomes for patients with AML.
3⃣📌Metabolic pathways fuelling OXPHOS appear to be critical for AML cell survival and will potentially become therapeutic targets to improve outcomes for patients with AML.
🛑END OF TUTORIAL!!
🙏Please RT and👍Like if you enjoyed reading this :)
🏃🏃♂️🏃♀️Follow us for more such #tweetorial
🙏Please RT and👍Like if you enjoyed reading this :)
🏃🏃♂️🏃♀️Follow us for more such #tweetorial
Ref:
1. Blood. 2019 Jul 25;134(4):389-394.
2. Nat Med. 2018 Dec; 24(12): 1859–1866.
1. Blood. 2019 Jul 25;134(4):389-394.
2. Nat Med. 2018 Dec; 24(12): 1859–1866.
#hematology #clinicalresearch #collaborativeresearch #realworldevidence #oncology #bloodcancer #leusm #MedEd #MedTwitter #tweetorial #TweetOfTheDay #AMLsm #AML
• • •
Missing some Tweet in this thread? You can try to
force a refresh