This month at #ISNTweetorial, we thought it would be fun to visit ancient Greece! Well not the whole of ancient Greece. But we did visit a particular Greek goddess. Can you guess which one? 🤔
(Image: Wikipedia)
(Image: Wikipedia)
🎥The #ISNTweetorial team proudly presents - an epic story (with all the drama of ancient Greece) - ‘The pathogenesis of chronic kidney disease - mineral bone disease’
The curtain opens to phosphorus(P). In CKD, as the kidney function declines, the ability of the kidney to excrete P ⬇️
Once the eGFR falls below 60 mL/min/1.73m2, filtration of P ⬇️ and it begins to get retained (Image: flickr)
Once the eGFR falls below 60 mL/min/1.73m2, filtration of P ⬇️ and it begins to get retained (Image: flickr)

Why do we care so much about P? Well because as the levels of P ⬆️, two things happen:
1️⃣Calcium(Ca) level ⬇️
2️⃣Active vitamin D (calcitriol) synthesis and activity ⬇️
cjasn.asnjournals.org/content/6/2/440
1️⃣Calcium(Ca) level ⬇️
2️⃣Active vitamin D (calcitriol) synthesis and activity ⬇️
cjasn.asnjournals.org/content/6/2/440

Parathyroid hormone(PTH) kicks into action to ⬇️ reabsorption of P by the proximal tubules 👍
PTH also ⬆️ bone resorption to maintain Ca level 👍
Moreover, it ⬆️ calcitriol production.
But here’s the catch ➡️
PTH also ⬆️ bone resorption to maintain Ca level 👍
Moreover, it ⬆️ calcitriol production.
But here’s the catch ➡️
In what has been described as the ‘trade-off’ hypothesis, ⬆️ PTH does help to regulate levels of P, Ca and calcitriol. But the trade off is hyperparathyroidism 😱
cjasn.asnjournals.org/content/5/9/17…
cjasn.asnjournals.org/content/5/9/17…

But the main hero 🦸of our story is not PTH, but fibroblast growth factor 23 or FGF-23. Even before low P levels are noted, FGF-23 flips the ‘off’ 🚫button on Vit D
⬇️Calcitriol levels➡️⬇️ reabsorption of P by the kidneys and ⬇️absorption of P by the intestine
⬇️Calcitriol levels➡️⬇️ reabsorption of P by the kidneys and ⬇️absorption of P by the intestine
In fact, FGF-23 enters into the story much earlier than PTH - maybe even when the eGFR is at 90 ml/min/1.73 m2!
So the actual trade off?
You guessed it - ⬇️vitamin D, which in turn leads to ⬇️ Ca (and ultimately ⬆️ P and ⬆️ PTH)
So the actual trade off?
You guessed it - ⬇️vitamin D, which in turn leads to ⬇️ Ca (and ultimately ⬆️ P and ⬆️ PTH)

And what about Vitamin D?
In CKD, there are multiple mechanisms by which active Vit D levels can⬇️
✅⬇️ 1 alpha hydroxylase activity
✅Hyperphosphatemia
✅⬆️ FGF23
(Source: Comprehensive Clinical Nephrology, 6th edition)
In CKD, there are multiple mechanisms by which active Vit D levels can⬇️
✅⬇️ 1 alpha hydroxylase activity
✅Hyperphosphatemia
✅⬆️ FGF23
(Source: Comprehensive Clinical Nephrology, 6th edition)

As calcitriol level ⬇️, PTH charges in ⚡️guns blazing to maintain it. And that does help initially🙂
Ultimately, however, this response becomes maladaptive 🙁 and the bones simply say ‘no go’ (skeletal resistance to PTH).
Ultimately, however, this response becomes maladaptive 🙁 and the bones simply say ‘no go’ (skeletal resistance to PTH).

To summarize
⬇️ eGFR → ⬆️ FGF23 → ⬇️ calcitriol → ⬇️ Ca → ⬆️ PTH
⬇️ eGFR → ⬆️ P → ⬇️ Ca and ⬇️ calcitriol → ⬆️ PTH
⬇️ eGFR → ⬇️ calcitriol → ⬆️ PTH
Too much PTH → skeletal resistance to PTH → crazy high P and low Ca → CKD-MBD
⬇️ eGFR → ⬆️ FGF23 → ⬇️ calcitriol → ⬇️ Ca → ⬆️ PTH
⬇️ eGFR → ⬆️ P → ⬇️ Ca and ⬇️ calcitriol → ⬆️ PTH
⬇️ eGFR → ⬇️ calcitriol → ⬆️ PTH
Too much PTH → skeletal resistance to PTH → crazy high P and low Ca → CKD-MBD

Now I know what you are thinking - where’s the Greek goddess in all this?🤷♀️
⚡️Introducing Clotho, Goddess of Fate⚡️
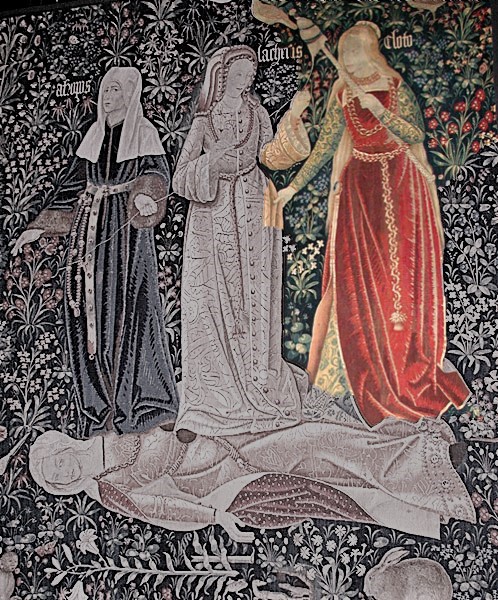
Clotho and her sisters Atropos and Lachesis constituted the Fates or the Moirai
Clotho had the power to choose who was born and who was to die
(Image:Wikipedia)
⚡️Introducing Clotho, Goddess of Fate⚡️
Clotho and her sisters Atropos and Lachesis constituted the Fates or the Moirai
Clotho had the power to choose who was born and who was to die
(Image:Wikipedia)

Interesting. But what does that have to do with CKD-MBD?
Well Klotho was the name chosen for the obligate co-receptor of FGF-23. In other words, Klotho is the patron goddess of our hero, FGF-23
kidney-international.org/article/S0085-…
Well Klotho was the name chosen for the obligate co-receptor of FGF-23. In other words, Klotho is the patron goddess of our hero, FGF-23
kidney-international.org/article/S0085-…

A ‘klotho centric’ theory argues that the klotho gene is a putative anti-ageing gene and CKD is a state of accelerated ageing
As early as CKD stage 1, the expression of klotho declines
⬇️ Klotho ➡️ ⬇️ FGF23 ➡️ ⬆️ PTH ➡️ CKD-MBD
As early as CKD stage 1, the expression of klotho declines
⬇️ Klotho ➡️ ⬇️ FGF23 ➡️ ⬆️ PTH ➡️ CKD-MBD

What we are basically trying to say is that CKD-MBD might actually be a state of 'klotho deficiency'🤯
Gives you something to think about doesn't it?
(Image: istockphoto)
Gives you something to think about doesn't it?
(Image: istockphoto)

What do you think about the Klotho theory of CKD-MBD?
That's all for today folks!
Keep watching this space for more on CKD-MBD and its management - The amazing @gag_aggarwal will be releasing a tweetorial soon!
Keep watching this space for more on CKD-MBD and its management - The amazing @gag_aggarwal will be releasing a tweetorial soon!
The ISN academy also has a wonderful resource on Ca and P homeostasis academy.theisn.org/isn/2017/wcn/2… and also on CKD-MBD academy.theisn.org/isn/#!*listing…
Think you already know all there is to know? Wait for the quiz! It’s coming soon
Lucky winners will be blessed by Clotho herself!
Ok maybe that was a joke
But you do get an e-certificate from the ISN🥇🥈🥉
Lucky winners will be blessed by Clotho herself!
Ok maybe that was a joke
But you do get an e-certificate from the ISN🥇🥈🥉
This tweetorial is brought to you by the #ISNTweetorial team @sibgokcay @gag_aggarwal @elliotktannor @aiakl2001 @Gawad_Nephro @Renaladdict @acssjr @nefrorantes @RClaure_nefro @BasuNephro @SabineKaram6 @xaviervel @sonia_rgzr @FerArceAmare @NamrataYParikh @ISNkidneycare
• • •
Missing some Tweet in this thread? You can try to
force a refresh