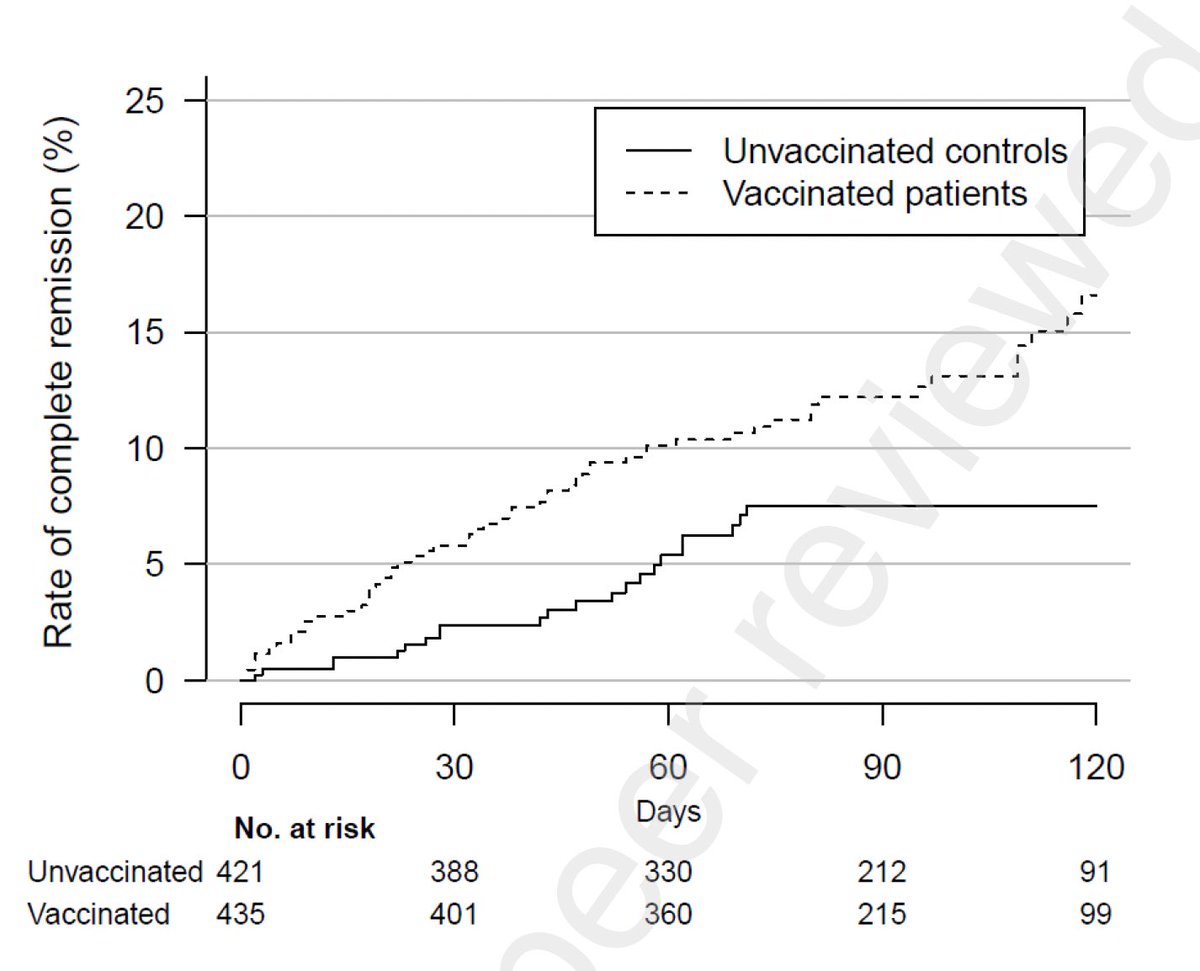
A preprint by Michael Simon et al @ArcadiaHealthIT shows that COVID vaccines given before or AFTER infection can reduce incidence of #longCOVID, based on a retrospective analysis of the health record of 240,648 COVID-19-infected people. 🧵(1/)
medrxiv.org/content/10.110…
medrxiv.org/content/10.110…
People who received at least one dose of any of the 3 COVID vaccines in the US prior to COVID diagnosis were 8.8x less likely to report >1 long COVID symptoms between 12-20 weeks after diagnosis. (2/) 

This reduction in LC risk appears high, given other studies that found 50% reduction or no reduction by prior vaccination in LC among breakthrough infection. Perhaps this depends on how one measures and defines long covid. (3/)
nature.com/articles/d4158…
nature.com/articles/d4158…
More strikingly, people who received at least one dose of any COVID vaccine AFTER COVID diagnosis also benefited. Likelihood of reporting >1 long COVID symptoms was reduced in those who received vax 0-4 wks (5.3x), 4-8 wks (3.2x) or 8-12 wks (2.2x) after COVID diagnosis. (4/) 

While more studies are needed to validate these findings, the implication is that people should get the COVID vaccine even after SARS-CoV-2 infections in order to reduce the risk of developing long COVID. Data support earlier the better. (5/)
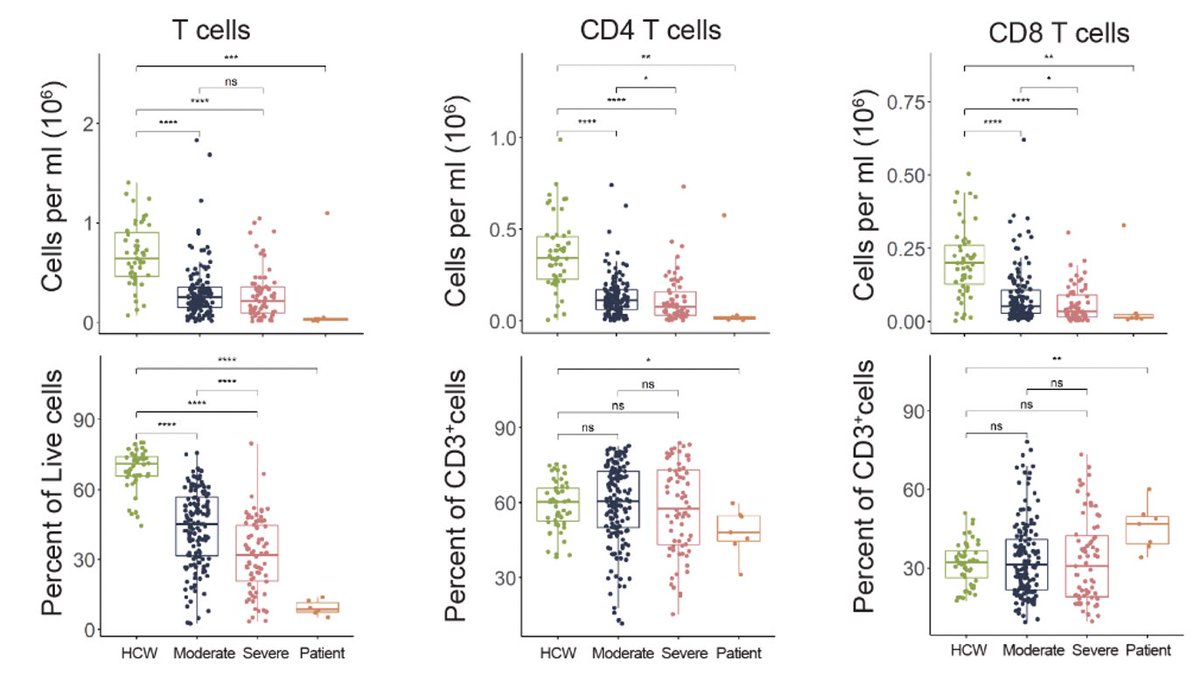
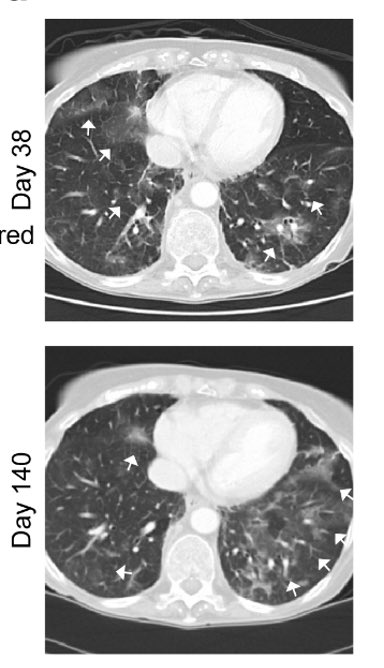
Mechanistically, post infection vaccination may encourage robust and rapid development of immune responses to the virus to 1) prevent establishment of viral reservoir or 2) reduce inflammatory damage leading to autoimmunity that may drive #longCOVID. (6/)
elemental.medium.com/how-vaccines-m…
elemental.medium.com/how-vaccines-m…
Current CDC guideline says "People with known current SARS-CoV-2 infection should defer vaccination at least until recovery from the acute illness (if symptoms were present) has been achieved and criteria to discontinue isolation have been met.” (7/)
cdc.gov/vaccines/covid…
cdc.gov/vaccines/covid…
However, CDC does not say how long people should wait before getting the vaccine after isolation is over. This study supports the vaccination of people who acquired SARS-CoV-2 within the first 4 weeks to reduce the risk for long COVID. (8/)
I’d love to know the answers re: What is the impact of the vaccine type? How do age, sex, existing conditions impact the findings? What is the impact of vax at 0-2 vs. 3-4 wks post infection on long COVID risk reduction? Do the findings hold for the Delta variant? (End)
• • •
Missing some Tweet in this thread? You can try to
force a refresh