In populations with high vaccine coverage, wouldn't we actually *expect* many infections to be breakthroughs?
What would this mean for the impact of unvaccinated-only testing programs as vacc. rates increase?
These questions frame our new preprint. 1/
medrxiv.org/content/10.110…
What would this mean for the impact of unvaccinated-only testing programs as vacc. rates increase?
These questions frame our new preprint. 1/
medrxiv.org/content/10.110…

By definition: when no one is vaccinated, 0% of infections are breakthroughs. When everyone is vaccinated, 100% of infections are breakthroughs.
So what happens in between?
Our study examines this question using a modeled population with mixed vax & prior infection status. 2/
So what happens in between?
Our study examines this question using a modeled population with mixed vax & prior infection status. 2/
Two things happen as vaccination rates increase:
1. Total infections decline—even imperfect vaccines reduce transmission.
2. The % of those infections that are breakthroughs increases, hitting 50/50 at 68% vax coverage in this scenario (35% prior inf. rate, VE≈2x mRNA). 3/
1. Total infections decline—even imperfect vaccines reduce transmission.
2. The % of those infections that are breakthroughs increases, hitting 50/50 at 68% vax coverage in this scenario (35% prior inf. rate, VE≈2x mRNA). 3/

This 50/50 tipping point was surprisingly insensitive to prior infection rates, ranging from 63-75% vax coverage.
This means we should stop being surprised when breakthroughs constitute a large % of infections…
…particularly in places (e.g. universities) w/ 80%+ vax rates. 4/
This means we should stop being surprised when breakthroughs constitute a large % of infections…
…particularly in places (e.g. universities) w/ 80%+ vax rates. 4/

Quick note that panel [a], above, gives context for [b] but is not, itself, anything new, and reinforces past work, including:
• popimmunity.biosci.gatech.edu
(@B_Lopman @joshuasweitz et al)
• medrxiv.org/content/10.110…
(@billy_gardner_ @DiseaseEcology)
• popimmunity.biosci.gatech.edu
(@B_Lopman @joshuasweitz et al)
• medrxiv.org/content/10.110…
(@billy_gardner_ @DiseaseEcology)
There's another interesting transition point — we track the *drivers* of infections in our model as well.
Under VE≈2x mRNA, when 76-82% are vaccinated, the unvaccinated community no longer drives a majority of transmission. 6/
Under VE≈2x mRNA, when 76-82% are vaccinated, the unvaccinated community no longer drives a majority of transmission. 6/

This transition point, too, must logically exist for *any* infectious disease and *any* vaccine, short of a hypothetical perfect transmission-blocking vaccine.
However, this still suggests we should reframe how we think of breakthrough transmission in highly vaxxed areas. 7/
However, this still suggests we should reframe how we think of breakthrough transmission in highly vaxxed areas. 7/
Omicron, waning, & boosting have many thinking about variation in VE, which affects the location of the transition points.
We captured VE ranges from literature estimates (for delta), w modeling (@billy_gardner_ @DiseaseEcology) for "hybrid" immunity. 8/
medrxiv.org/content/10.110…
We captured VE ranges from literature estimates (for delta), w modeling (@billy_gardner_ @DiseaseEcology) for "hybrid" immunity. 8/
medrxiv.org/content/10.110…

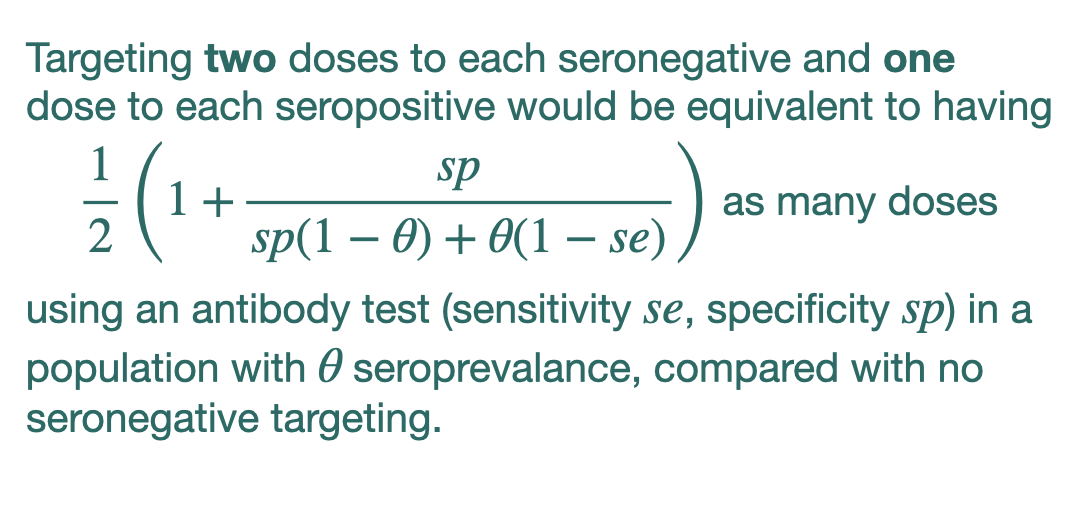
In this context, what if we test *only* the unvaccinated, given that they drive fewer infections when vaccination rates are v high?
We use models of the impact of testing w @michaelmina_lab @MilindTambe_AI et al — modified to be unvaccinated-only. 9/
science.org/doi/full/10.11…
We use models of the impact of testing w @michaelmina_lab @MilindTambe_AI et al — modified to be unvaccinated-only. 9/
science.org/doi/full/10.11…
By reducing transmission only from infected unvaccinated folks, unvaccinated-only testing programs have 2 effects:
1. They reduce R, the reproductive number.
2. They shift the 50/50 breakthrough-transmission threshold.
However, these impacts depend on testing compliance! 10/
1. They reduce R, the reproductive number.
2. They shift the 50/50 breakthrough-transmission threshold.
However, these impacts depend on testing compliance! 10/
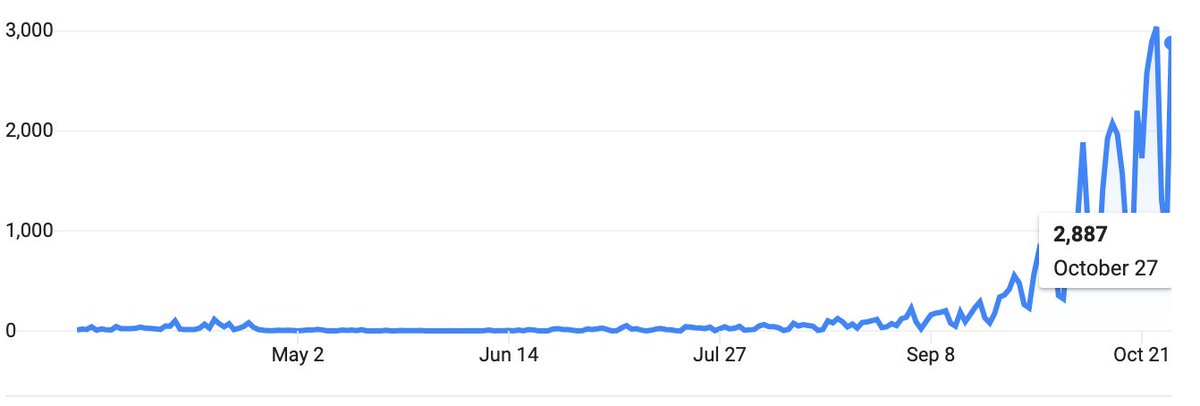
Aside: on CU's campus, mandatory weekly PCR testing compliance was ~50% for students, a result reported earlier this year in JID.
[Compliance was worse for faculty! 😂]
Many other institutions' dashboards show similar student compliance, in fact! 11/
academic.oup.com/jid/article/22…
[Compliance was worse for faculty! 😂]
Many other institutions' dashboards show similar student compliance, in fact! 11/
academic.oup.com/jid/article/22…
Weekly PCR testing of only the unvaccinated (1d TAT, delta VL kinetics*) decreases the vaccination rate ranges where we hit 50/50 breakthrough transmission (right), but affects breakthrough infections less so (left). 12/
*h/t @StephenKissler @yhgrad @NathanGrubaugh et al
*h/t @StephenKissler @yhgrad @NathanGrubaugh et al

While testing the unvaccinated therefore shifts the drivers of transmission, it also reduces R.
Ignoring risk compensation, 1 of 3 things must be true:
I. Testing drops R, yet still R>1.
II. Testing drops R to R<1.
III. R was already below 1 due to population immunity.
13/
Ignoring risk compensation, 1 of 3 things must be true:
I. Testing drops R, yet still R>1.
II. Testing drops R to R<1.
III. R was already below 1 due to population immunity.
13/
These three regions are clearly visible in simulations where we measure % reductions in total infections (vs no testing) on heatmaps.
• The R=1 (with testing) isocline separates I from II.
• The R=1 (without testing; herd immunity) isocline separates II from III.
14/
• The R=1 (with testing) isocline separates I from II.
• The R=1 (without testing; herd immunity) isocline separates II from III.
14/

In short, unvaccinated-only testing is valuable in regions I and II. It is sufficient only in II.
The size of region II—the effective testing envelope—and magnitude of impact BOTH depend strongly on test compliance.
50% compliance = lower impact, in more limited scenarios. 15/
The size of region II—the effective testing envelope—and magnitude of impact BOTH depend strongly on test compliance.
50% compliance = lower impact, in more limited scenarios. 15/
Beyond the herd immunity threshold, when vaccination & prior infection rates are high enough (region III), unvaccinated-only testing has little impact.
This also applies to *universal* testing, a recent point made by @RS_McGee @jrhomburger @CT_Bergstrom
medrxiv.org/content/10.110…
This also applies to *universal* testing, a recent point made by @RS_McGee @jrhomburger @CT_Bergstrom
medrxiv.org/content/10.110…
In sum, we show 3 key transitions as vax rates increase:
1. fewer infections overall,
2. of which a higher % will be breakthroughs,
3. driven less & less by the unvaccinated.
Especially in highly vaxxed areas, we shouldn't be surprised when most infections are breakthroughs! 17/
1. fewer infections overall,
2. of which a higher % will be breakthroughs,
3. driven less & less by the unvaccinated.
Especially in highly vaxxed areas, we shouldn't be surprised when most infections are breakthroughs! 17/
Our modeling also shows that unvaccinated-only testing is effective, but only for some combos of vax+prior infection, combos which can be predicted.
Testing is relatively ineffective if compliance is low.
Incentives for testing are critical—and, vaccination is better. 18/
Testing is relatively ineffective if compliance is low.
Incentives for testing are critical—and, vaccination is better. 18/
This is a preprint, and, as such, we're open to comments and suggestions! Thanks!
Finally, although I'm the one on the team who tweets a lot, this work was led by first authors @CaseyEMiddleton and @bubar_kate from @CUBoulder's IQ Bio PhD program. 19/19
medrxiv.org/content/10.110…
Finally, although I'm the one on the team who tweets a lot, this work was led by first authors @CaseyEMiddleton and @bubar_kate from @CUBoulder's IQ Bio PhD program. 19/19
medrxiv.org/content/10.110…
• • •
Missing some Tweet in this thread? You can try to
force a refresh