
Covid (@UCSF) Chronicles, Day 647 (!)
I haven’t done a San Francisco update for a while. Now seems like a good time, since SF – the most vaxxed big city in the U.S. – may offer lessons for the nation about how an Omicron surge is influenced by high vax (& masking) rates.(1/25)
I haven’t done a San Francisco update for a while. Now seems like a good time, since SF – the most vaxxed big city in the U.S. – may offer lessons for the nation about how an Omicron surge is influenced by high vax (& masking) rates.(1/25)
Bottom line is that some normally-scary numbers (surging cases & test positivity %) haven’t led to big jumps in hospitalizations. The big question: is it still too early to tell, or is this the hoped-for case–hospitalization dissociation at play? I’m going with the latter.(2/25)
Let’s start w/ SF before focusing @UCSFHospitals. Clearly SF is seeing a big surge in cases: ~250 cases per day (7-day daily average is 161; this lags due to the steep uptick), up from avg of 45/d in late Nov. (Figure). So about a 5-fold rise in recent weeks. Concerning. (3/25) 

Yet SF hospital numbers have barely budged: 36 (Fig). Why? My best guess: a combination of Omicron’s lower severity hitting SF’s huge wall of vaccination. In any case, thank goodness! (4/25) 

I doubt explanation is "too early" – if we were mirroring Delta’s severity we'd see a big impact on hospital #'s by now. @Farzad_MD elegantly walked through a similar argument for NYC yesterday – it's not too early to make the call, there or here.
https://twitter.com/Farzad_MD/status/1474245821935886337(5/25)
For a closer look, let’s dive into data from @UCSFHospitals. As you may recall, one of my go-to numbers is our “asymptomatic test positivity rate.” This is the rate of positive Covid tests in patients have no Covid symptoms – we have this useful number since every pt who…(6/25)
… is admitted or has an outpatient procedure – everything from cancer surgery to a heart attack to a colonoscopy – is tested for Covid. I use this number to estimate the chance that somebody sitting at a nearby table in a San Francisco restaurant has asymptomatic Covid.(7/25)
Remember that your chances of catching Covid in a given setting (restaurant, flight, etc) if a function of the characteristics of the virus (Omicron being more infectious) x protection (particularly vax status and masks) x setting (indoor, ventilation, etc) x (CRUCIALLY)…(8/25)
… the chances that a person near you actually has Covid and is infectious. As prevalence in a community goes up, the chances of you getting Covid from an encounter goes right up with it, even if nothing else has changed. So prevalence is pretty key in thinking about risk.(9/25)
Yes, I know that a % drawn from a big academic hospital isn’t perfect – many of our pts come from far away, patients are older & probably likelier to be vaxxed than avg population, etc. But it’s still a useful estimate, and following it over time is particularly helpful.(10/25)
For reference, the lowest our asymptomatic test pos. rate @UCSFHospitals ever got (pre-Delta) was ~0.2%, or ~1 in 500 patients. The rate was 0.92% on Dec 14, 10 days ago. So on that day, about one in 110 patients with no symptoms of Covid tested positive. (11/25)
And now (drumroll), over the last few days that number has been ~4.6%! (Figure; the 7-day avg, seen on the chart [2.98%], is lagging since the rate is climbing so steeply.) This implies that the chance of an asymptomatic person in SF having Covid is now nearly 1 in 20.(12/25) 

This means that, if you find yourself in a closed space in SF with 25 other people who feel fine, it’s a near certainty that one of them has Covid. And since it’s likely they have Omicron, their virus is about twice as transmissible as it would have been last month.(13/25)
AND, if you’re vaccinated and boosted you’re ~25% less well protected against infection by your vax then you were with Delta (efficacy ~70% vs. prior 95%). If you haven’t gotten boosted, your protection has fallen by at least 2/3rds. I don’t like these odds… (14/25)
… one little bit, and they have informed my decision to stop indoor restaurant dining for now and to wear an N95 or equivalent in any indoor space where I’m not confident that everyone is boosted and is asymptomatic.(15/25)
You may have noticed the other (upper) curve on the chart (Fig shown again). Ten days ago, our SYMPTOMATIC test + rate was 3.5%. These are tests of people who sought medical attention because they had symptoms consistent with Covid. Of course, all of them were "sure"…(16/25) 
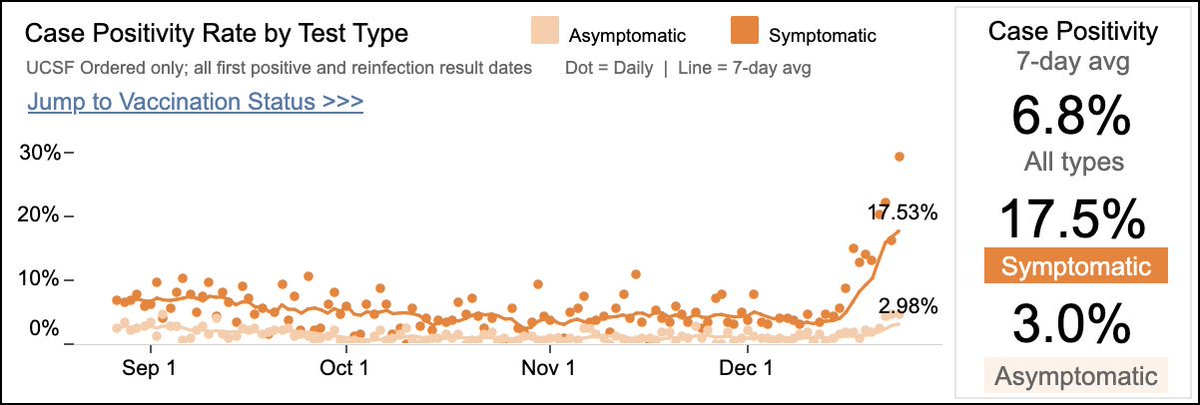
… they had Covid, but, last week, only ~1 in 30 actually did.
Well, that # has also skyrocketed, now a 7-d avg of 17.5% (this also this underestimates the true risk: recent days have been closer to 25%, or 1 in 4.) I don’t recall it ever being that high here before.(17/25)
Well, that # has also skyrocketed, now a 7-d avg of 17.5% (this also this underestimates the true risk: recent days have been closer to 25%, or 1 in 4.) I don’t recall it ever being that high here before.(17/25)
Now that I’ve scared the pants off you, let’s turn to hospitalizations @UCSFHospitals. Like SF generally, it's also quite reassuring: our hospital #'s remain very low. We currently have 10 Covid patients in our hospital, as low as we’ve been for the past few months (Fig).(18/25) 

Similar to the SF argument, if case-to-hospitalization ratios were mirroring those of Delta, I’d expect at least 2-3x those hospitalizations by now. And even more impressive: we only have 4 non-ICU patients, down from ~10 last week. When we surge, it’s usually the…(19/25)
…non-ICU floors that fill up first, with patients often deteriorating a few days later and requiring the ICU. I don’t know this for sure, but I’m guessing that some of our six current ICU patients have been there for days or weeks, and represent older (Delta) cases.(20/25)
So… is this a good news or bad news story? To me, it's mostly good news. Bad: even in highly vaccinated & careful SF, Omicron is spreading fast. While fully vaxxed and boosted people have some protection, and good masks offer more, it’s clear that – when it comes…(21/25)
…to infections – we’ve never seen anything like Omicron.
On the other hand, the big question that I’ve been asking all month – namely, is Omicron truly less severe, particularly in vaxxed patients – has now been answered, to my satisfaction at least. The answer is yes! (22/25)
On the other hand, the big question that I’ve been asking all month – namely, is Omicron truly less severe, particularly in vaxxed patients – has now been answered, to my satisfaction at least. The answer is yes! (22/25)
Our experience in SF, combined w/ several studies from other countries, is showing that Omicron leads to a milder illness, particularly in vaxxed populations. This, combined with the mercifully short surge in So. Africa, makes me far more optimistic than I was last week.(23/25)
Since some protection comes from vax status (w/ little protection from prior infection) rather than inherent properties of the virus, I’d be far less upbeat in a less vaccinated place, & far more scared if I wasn’t vaxxed and boosted. The unvaxxed are playing a risky hand.(24/25)
The disconnect between cases/test pos. and hospitalizations/severe illnesses now seems very solid, & it’s the best Covid news we’ve gotten for months. Don’t let your guard down (I’m not). But it’s possible we’ll get thru winter without being nearly as crushed as I feared.(25/end)
A few of my more astute readers have pointed out (thanks!) I got the math wrong (sorry): if crowd is 25 people & the probability of each having Covid is 4.6%, then the probability of someone having Covid is 69%, not a near certainty. Don't reach >90% chance until ~45 in crowd.
By the way, I'll be shocked if we see NO bump in hospitalizations in coming wks. UK & So. Africa data point to ~50% fall in hospitalizations compared w/ Delta. If we see huge case bump in SF, some hospitalizations are sure to follow. But seems unlikely it'll be overwhelming here.
• • •
Missing some Tweet in this thread? You can try to
force a refresh




