1) Welcome to our new #accredited #tweetorial on risk stratification to identify the patient with #T2D and #DKD most at risk for rapid progression to advanced CKD. I am Christos Argyropoulos MD, PhD (@ChristosArgyrop), Division Chief, Nephrology, @UNMHSC. 

2) This #accredited #tweetorial series on #kidneydisease #DKD through the lens of #T2D is supported by an independent educational grant from the Boehringer Ingelheim/Lilly Alliance and is intended for healthcare providers.
3) This activity is accredited for #physicians #physicianassociates #nurses #NPs #pharmacists. Past programs still eligible for credit can be found at ckd-ce.com. Faculty disclosures are at ckd-ce.com/disclosures/. FOLLOW US for regular programs by expert faculty!
4) Let's start with a case!
Your 1st clinic appointment is a 68♀️ with long standing (15 years) Type 2 Diabetes (#T2D), complicated by retinopathy and Chronic Kidney Disease (#CKD). Her most recent laboratory data were obtained 3 months & 2 weeks prior to this visit:
Your 1st clinic appointment is a 68♀️ with long standing (15 years) Type 2 Diabetes (#T2D), complicated by retinopathy and Chronic Kidney Disease (#CKD). Her most recent laboratory data were obtained 3 months & 2 weeks prior to this visit:
5)
✔️estimated Glomerular Filtration Rate (eGFR) of 45, 52 ml/min/1.73m2
✔️Urine Albumin to Creatinine Ratio, UACR of 350 & 650 mg/g.
The patient is on Lisinopril 20mg/d, Rosuvastatin 20 mg & amlodipine 10mg. She asks you about her risk for further #CKD progression:
✔️estimated Glomerular Filtration Rate (eGFR) of 45, 52 ml/min/1.73m2
✔️Urine Albumin to Creatinine Ratio, UACR of 350 & 650 mg/g.
The patient is on Lisinopril 20mg/d, Rosuvastatin 20 mg & amlodipine 10mg. She asks you about her risk for further #CKD progression:
6) Before diving in the answer, let's define the risk factors for developing #CKD in patients with #T2D.
These have been defined as susceptibility, initiation & progression factors that affect hemodynamic, metabolic, inflammatory & fibrotic pathways
🔓doi.org/10.2215/CJN.11…

These have been defined as susceptibility, initiation & progression factors that affect hemodynamic, metabolic, inflammatory & fibrotic pathways
🔓doi.org/10.2215/CJN.11…


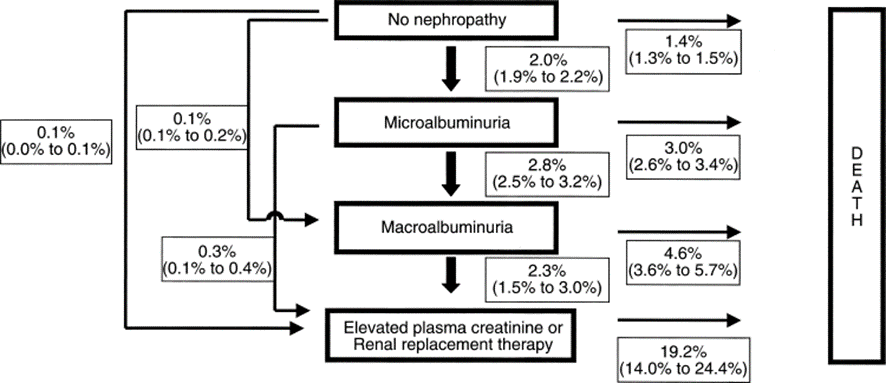
7) A conceptual model for the development of #CKD has been put forward based on observations in patients with Type 1 Diabetes. The timeline and the progression of events are less well delineated & the pattern not so clearcut in patients with #T2D 🔓doi.org/10.1016/j.kint… 



8) The #UKDPS study has informed understanding of #CKD progression in #T2D:
➡️15 yrs after diagnosis, 40% of participants developed albuminuria
➡️30% developed eGFR< 60 ml/min per 1.73 m2 or doubling of the serum creatinine
🔓pubmed.ncbi.nlm.nih.gov/16731850/
🔓pubmed.ncbi.nlm.nih.gov/12472787/
➡️15 yrs after diagnosis, 40% of participants developed albuminuria
➡️30% developed eGFR< 60 ml/min per 1.73 m2 or doubling of the serum creatinine
🔓pubmed.ncbi.nlm.nih.gov/16731850/
🔓pubmed.ncbi.nlm.nih.gov/12472787/
9) While 60% of patients did not develop albuminuria during UKDPS , once *any* albuminuria developed, rates of events (whether death or progression of #CKD) were higher than those before the development of albuminuria.
👉Albuminuria is a major risk factor in #T2D
👉Albuminuria is a major risk factor in #T2D
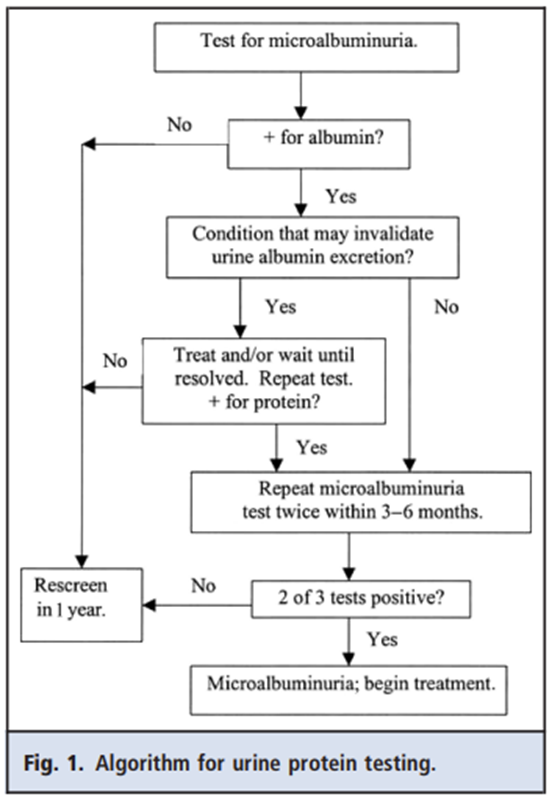
10) How should we assess albuminuria & integrate this lab test into our clinical risk assessment?
It all starts with a simple measurement!
👉Measurement of the urine albumin-to-creatinine ratio (#UACR) in an untimed urinary sample is the preferred screening strategy in #T2D
It all starts with a simple measurement!
👉Measurement of the urine albumin-to-creatinine ratio (#UACR) in an untimed urinary sample is the preferred screening strategy in #T2D
11) There are various ways to detect the presence of albuminuria & different clinical cutoffs that have been proposed to grade its severity.
The current laboratory 🔓academic.oup.com/clinchem/artic… & @goKDIGO 🔓kdigo.org/wp-content/upl… guidelines provide a handy ref for assays & cutoffs

The current laboratory 🔓academic.oup.com/clinchem/artic… & @goKDIGO 🔓kdigo.org/wp-content/upl… guidelines provide a handy ref for assays & cutoffs


12) Practice Points:
✔️ Prefer a quantitative over a dipstick test
✔️If a patient who has had previously normal values, develops UACR >30mg/g, the test should be repeated 2x over a 3-6mo period
✔️UACR 30-300mg/g ➡️moderate albuminuria
✔️UACR > 300 mg/g ➡️ severe proteinuria
✔️ Prefer a quantitative over a dipstick test
✔️If a patient who has had previously normal values, develops UACR >30mg/g, the test should be repeated 2x over a 3-6mo period
✔️UACR 30-300mg/g ➡️moderate albuminuria
✔️UACR > 300 mg/g ➡️ severe proteinuria
13) How did we come with the recommendation to examine #UACR in an untimed First Morning Void (FMV) sample? Let’s nerd out with #RENAAL, one of the two trials that made Angiotensin Receptor Blockers (#ARBs) standard of care for #CKD in #T2D 🔓nejm.org/doi/full/10.10….
14) Data from the 701 participants in RENAAL were used to probe the predictive ability of different measures of proteinuria
🔓jasn.asnjournals.org/content/21/8/1…
✔️ (U)ACR in FMV
✔️Urine Albumin Concentration in FMV
✔️24hr Urine Albumin Excretion (UAE)
✔️24hr Urine Protein Excretion (UPE)
🔓jasn.asnjournals.org/content/21/8/1…
✔️ (U)ACR in FMV
✔️Urine Albumin Concentration in FMV
✔️24hr Urine Albumin Excretion (UAE)
✔️24hr Urine Protein Excretion (UPE)
15) Key findings from this paper:
➡️ UACR (continuous and as quintiles) had the highest standardized hazard ratio for doubling serum creatinine (DSC, loss of ~50% kidney function) or End Stage Kidney (Renal) Disease #ESRD #ESKD
➡️ UACR had the highest AUC to predict #ESKD, DSC


➡️ UACR (continuous and as quintiles) had the highest standardized hazard ratio for doubling serum creatinine (DSC, loss of ~50% kidney function) or End Stage Kidney (Renal) Disease #ESRD #ESKD
➡️ UACR had the highest AUC to predict #ESKD, DSC



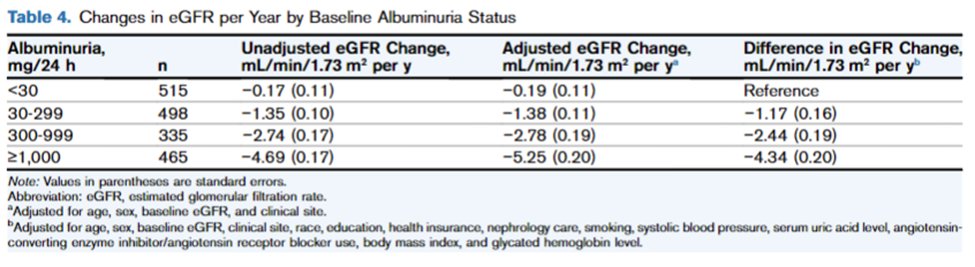
16) RENAAL is not the only study that has linked measures of proteinuria/albuminuria with #CKD progression and #ESKD in patients with depressed eGFR. Enter the CRIC (Chronic Renal Insufficiency Cohort) Study: 🔓pubmed.ncbi.nlm.nih.gov/29784612/
👉Albuminuria determined BOTH outcomes

👉Albuminuria determined BOTH outcomes


17) Using guideline & clinically relevant cutoffs of albuminuria (<30, 30-299, 300-999, >1,000mg/d):
✔️#ESKD rates were 7.4, 34.8, 78.7, 178.7 per 1,000 person-years (PYs)
✔️#CKD progression rates were 17.0, 61.4, 130.5, 295.1 per 1,000 PYs
✔️Loss of eGFR also tracked albuminuria
✔️#ESKD rates were 7.4, 34.8, 78.7, 178.7 per 1,000 person-years (PYs)
✔️#CKD progression rates were 17.0, 61.4, 130.5, 295.1 per 1,000 PYs
✔️Loss of eGFR also tracked albuminuria
18) While the previous studies examined the baseline albuminuria as predictor of risk, the more relevant scenario for clinical practice is one in which multiple measurements of eGFR & baseline albuminuria are available for dynamic risk assessment about #CKD progression.
19) ➡️In an analysis led by @NavTangri proteinuria & the latest available eGFR were significant predictors of kidney failure
🔓pubmed.ncbi.nlm.nih.gov/27693260/
➡️A certain drop of eGFR by 25% within 1yr was associated w/ #ESKD in the CKD Prognosis Consortium
🔓academic.oup.com/ndt/article/27…

🔓pubmed.ncbi.nlm.nih.gov/27693260/
➡️A certain drop of eGFR by 25% within 1yr was associated w/ #ESKD in the CKD Prognosis Consortium
🔓academic.oup.com/ndt/article/27…


20) To sum up:
✔️Albuminuria (preferably measured as a FMV UACR) is a continuous measure of risk for #CKD progression among pts w/ #T2D
✔️Risk is particularly high for UACR > 300mg/g
✔️ eGFR (& changes in eGFR) are also associated with progression risk
It is now time to …
✔️Albuminuria (preferably measured as a FMV UACR) is a continuous measure of risk for #CKD progression among pts w/ #T2D
✔️Risk is particularly high for UACR > 300mg/g
✔️ eGFR (& changes in eGFR) are also associated with progression risk
It is now time to …
21) ... return to the patient from our clinical vignette, and use the @goKDIGO guideline "heatmap" kdigo.org/wp-content/upl… to assess her risk.
Her eGFR is between 45-60 ml/min/1.73m2 & UACR > 300mg/gm, thus putting her at VERY HIGH risk for #CKD progression (X in the chart).
Her eGFR is between 45-60 ml/min/1.73m2 & UACR > 300mg/gm, thus putting her at VERY HIGH risk for #CKD progression (X in the chart).
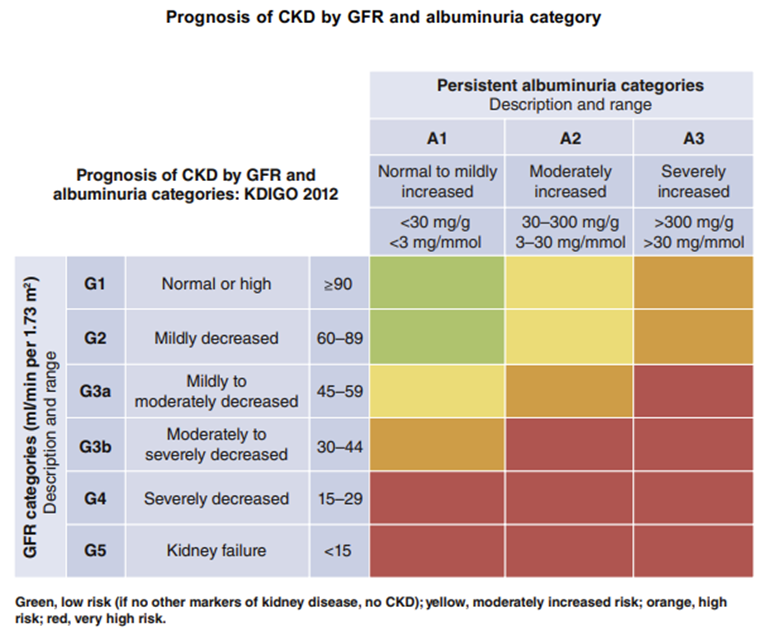
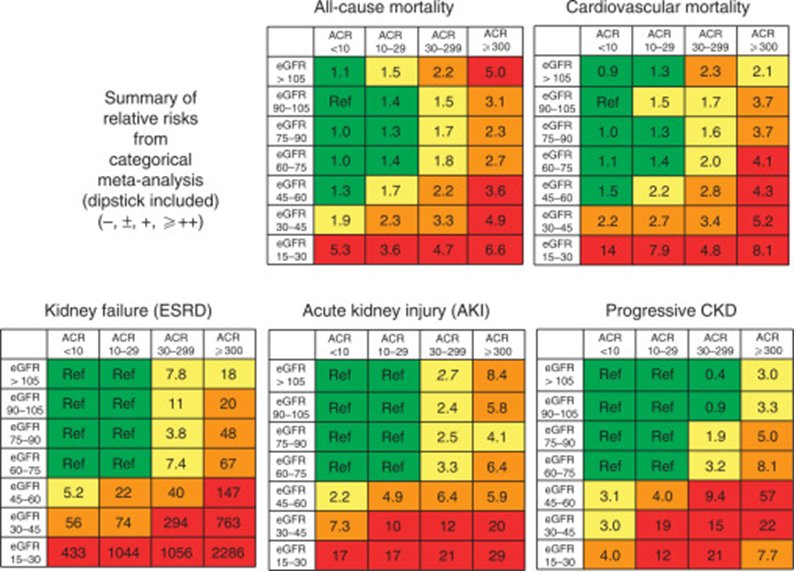
22) Similar heatmaps also apply to the other risks associated with #CKD:
✔️All-cause Death
✔️Cardiovascular Death
✔️Progression of #CKD
✔️#ESKD/#ESRD
✔️Acute Kidney Injury
🔓kidney-international.org/article/S0085-…
But nowadays we can go beyond such semiquantitative risk stratification!
✔️All-cause Death
✔️Cardiovascular Death
✔️Progression of #CKD
✔️#ESKD/#ESRD
✔️Acute Kidney Injury
🔓kidney-international.org/article/S0085-…
But nowadays we can go beyond such semiquantitative risk stratification!
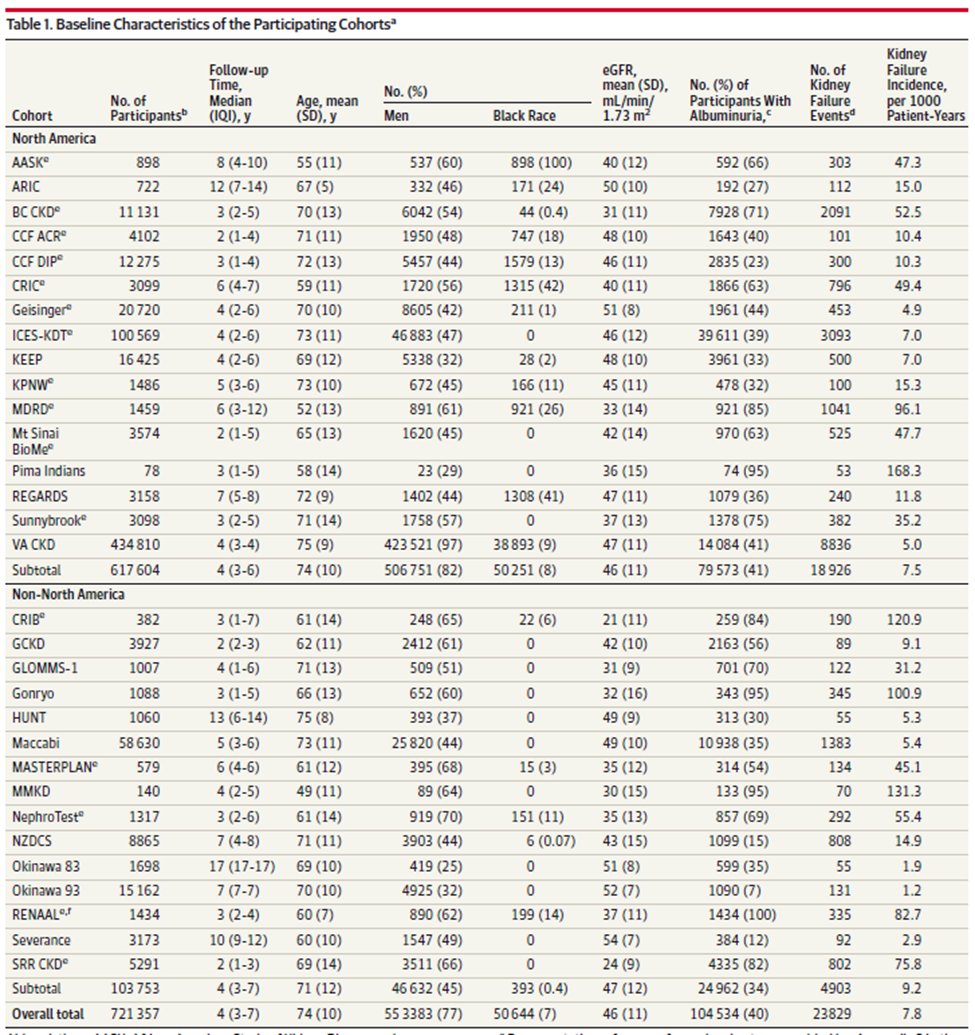
23) The Kidney Risk Failure Equation (#KRFE) were developed in patients with #CKD stages G3-5 in Canada (thanks @NavTangri) & subsequently validated in more than 700k patients from 30+ countries.
Available in smartphone apps (e.g. @QxMD) and the web kidneyfailurerisk.com
Available in smartphone apps (e.g. @QxMD) and the web kidneyfailurerisk.com
24) There are two versions of this risk calculator:
➡️4 Variable: Age, Sex, eGFR, UACR
➡️8 Variable. Which of the following is NOT one of the additional 4 variables in the 8-variable model?
➡️4 Variable: Age, Sex, eGFR, UACR
➡️8 Variable. Which of the following is NOT one of the additional 4 variables in the 8-variable model?
25) Mark your answer and return tomorrow for more on risk stratification for #CKD among pts w/ #T2D and #DKD! You're earning CE/#CME!
Nods to @poyanmehr @GarySingerMD @iheartkidneys @GoggleDocs @MedTweetorials @GlomCon @ValleAlfonso @SantosGallegoMD @MunerMohamed1 @brendonneuen
Nods to @poyanmehr @GarySingerMD @iheartkidneys @GoggleDocs @MedTweetorials @GlomCon @ValleAlfonso @SantosGallegoMD @MunerMohamed1 @brendonneuen
26) Welcome back! We're talking about risk stratification for #T2D+#DKD to➡️#CKD. I am @ChristosArgyrop & you're earning CE/#CME! 👏 @dguerrot @kdjhaveri @AtulPathak31 @lissabauer @sophia_kidney @RpratleyMD @nephondemand @NephroWorldCup @edgarvlermamd @SeguraCardio @kamleshkhunti
27) Back to yesterday's closing poll. Scroll⬆️and COMMIT if you haven't already! The 8⃣-variable version of the Kidney Risk Failure Equation (#KRFE) includes 4 Variable + Calcium, Phosphorus, Bicarbonate, & *Serum* Albumin
28) ✔️Both formulas include an adjustment for geography
✔️ 8V formula may discriminate better
🔓jamanetwork.com/journals/jama/…

✔️ 8V formula may discriminate better
🔓jamanetwork.com/journals/jama/…


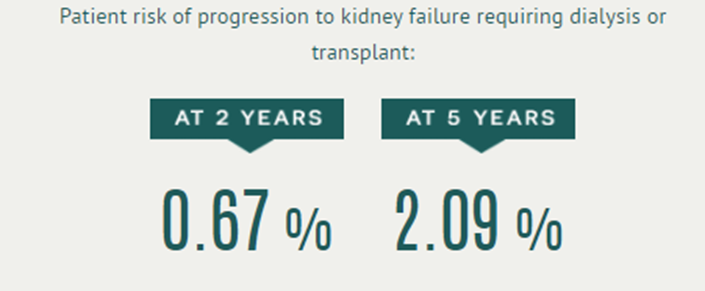
29) The KRFE quantifies the risk for our patient & allows us to discuss the next steps for managing her risk
✔️referral to Nephrology as her 5 year risk is > 3%
✔️team based care (if the 2 year risk > 10%)
✔️preparation for renal replacement (if the 2 year risk > 20%)

✔️referral to Nephrology as her 5 year risk is > 3%
✔️team based care (if the 2 year risk > 10%)
✔️preparation for renal replacement (if the 2 year risk > 20%)

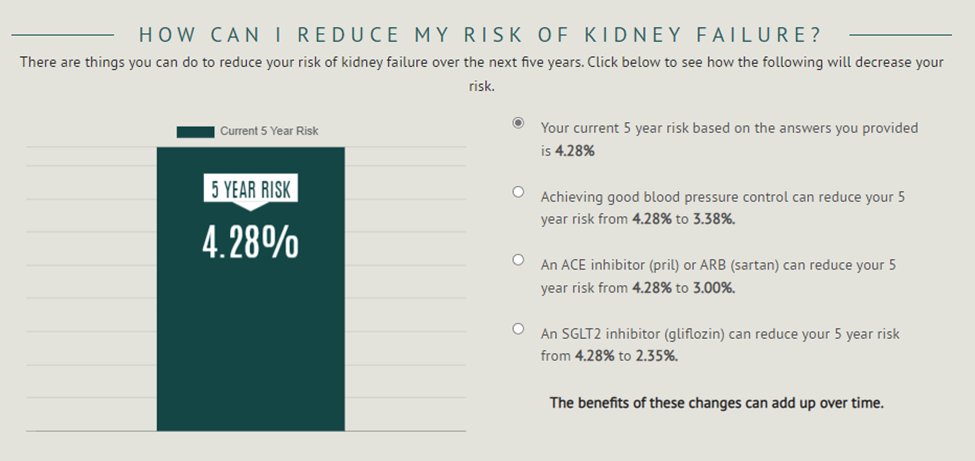
30) Having a number helps our patients understand their risks. But we can also use this number to *reduce* their risk. In this case (68👩🦳, with eGFR of 45 & UACR ~500mg/g), proteinuria is the only modifiable risk factor. If the latter were to ⬇️ 100mg/g, the KFRE yields: 
31) ⬇️albuminuria➡️ ⬇️risk. Or should the patient assume that because she is taking guideline-based therapy (an Angiotensin Converting Enzyme Inhibitor #ACEi), she is protected from #CKD progression?
Key papers 🔓pubmed.ncbi.nlm.nih.gov/23506627/
🔓pubmed.ncbi.nlm.nih.gov/15149345/
to the rescue
Key papers 🔓pubmed.ncbi.nlm.nih.gov/23506627/
🔓pubmed.ncbi.nlm.nih.gov/15149345/
to the rescue
32) What did these re-analyses of RENAAL, IDNT, OVERT show?
✔️Changes in albuminuria in the first 6mo of therapy predict long term response:
👉⬇️albuminuria by 50% ➡️⬇️#ESKD by 45%
👉risk⬇️ was continuously related to albuminuria⬇️
✔️risk highest in those with highest UACR


✔️Changes in albuminuria in the first 6mo of therapy predict long term response:
👉⬇️albuminuria by 50% ➡️⬇️#ESKD by 45%
👉risk⬇️ was continuously related to albuminuria⬇️
✔️risk highest in those with highest UACR



33) Upon reviewing the patient's chart, you find that the patient has never been prescribed > 20 mg of Lisinopril. The patient also has history of Acute Kidney Injury (#AKI) during a hospitalization for sepsis. Which of the following is true about her #CKD progression risk?
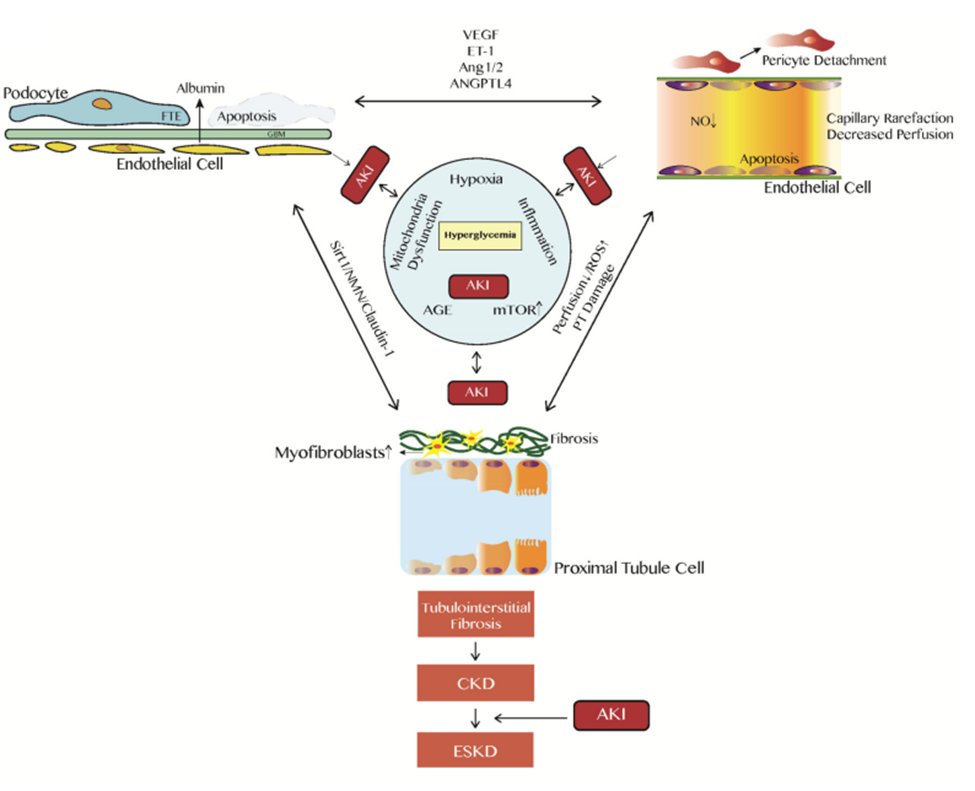
34) AKI, low eGFR & Albuminuria are ALL predictors of #CKD progression
🔓diabetesjournals.org/care/article/3…
✔️AKI⬆️risk by 247%
✔️Albuminuria⬆️risk by 423%
✔️⬇️eGFR by 10 ml/min/1.73m2⬆️risk by 22%
Maladaptive responses inside the kidney underline this nexus
🔓ncbi.nlm.nih.gov/labs/pmc/artic…
🔓diabetesjournals.org/care/article/3…
✔️AKI⬆️risk by 247%
✔️Albuminuria⬆️risk by 423%
✔️⬇️eGFR by 10 ml/min/1.73m2⬆️risk by 22%
Maladaptive responses inside the kidney underline this nexus
🔓ncbi.nlm.nih.gov/labs/pmc/artic…
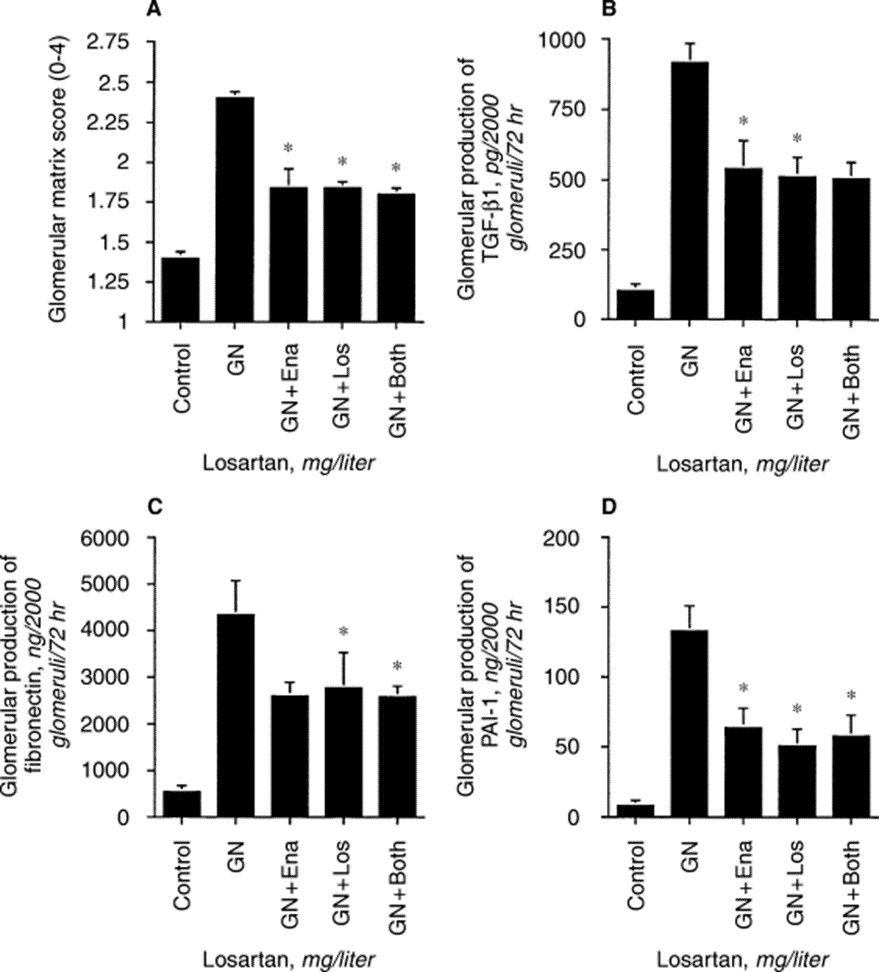
35) The dose of the background Inhibitor of the Renin Angiotensin System (#RASi) is an important predictor of #CKD progression.
The relevant preclinical observations were made >25 years ago: maximizing any RASi decreased production of fibrotic factors
🔓kidney-international.org/article/S0085-…
The relevant preclinical observations were made >25 years ago: maximizing any RASi decreased production of fibrotic factors
🔓kidney-international.org/article/S0085-…
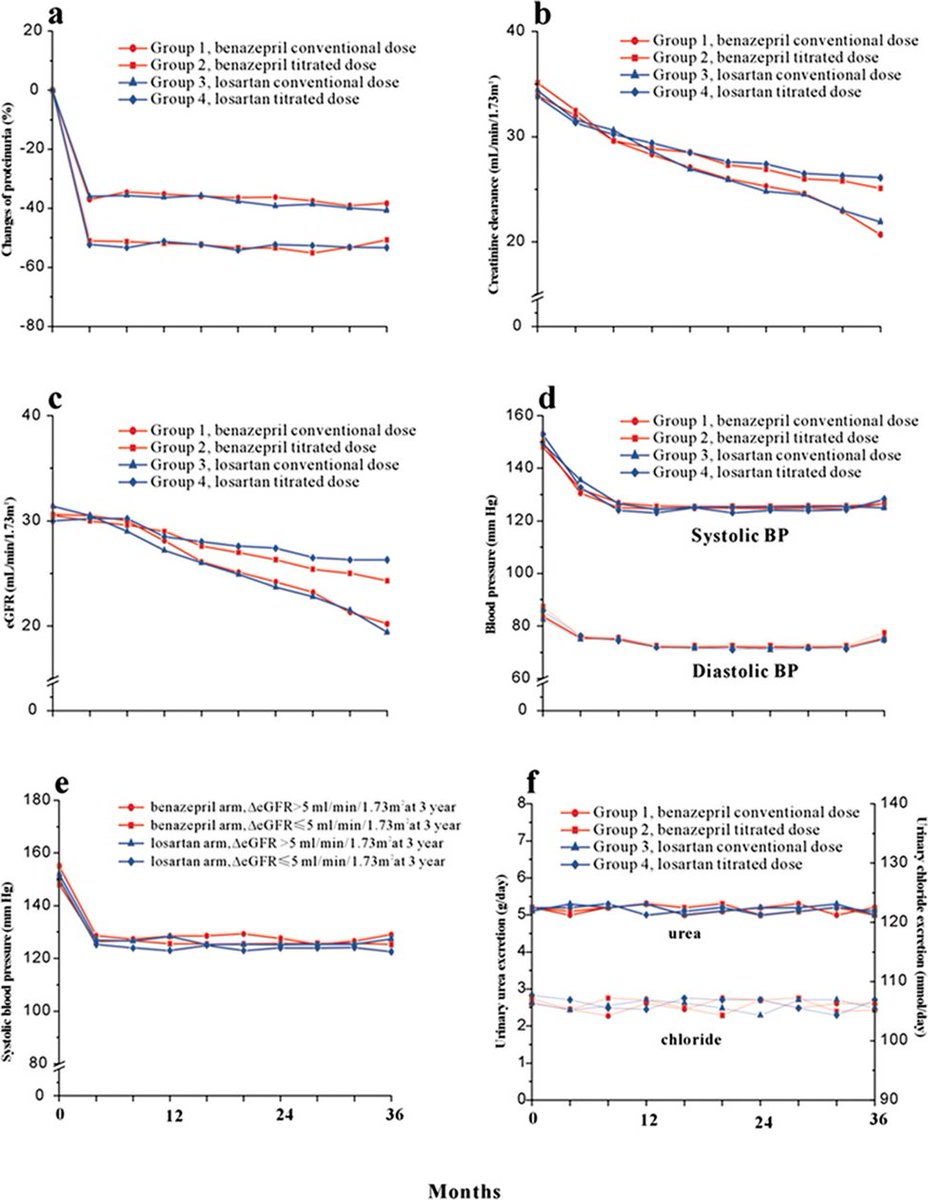
36) The Renoprotection of Optimal Antiproteinuric Doses (ROAD) study: effects of individualized maximization of ACEi or #ARB doses on #CKD progression & #ESKD.
Titration
👉risk⬇️by ~50%
👉proteinuria⬇️by ~20%
👉slower eGFR loss
👉no⬆️effect on BP
🔓jasn.asnjournals.org/content/18/6/1…


Titration
👉risk⬇️by ~50%
👉proteinuria⬇️by ~20%
👉slower eGFR loss
👉no⬆️effect on BP
🔓jasn.asnjournals.org/content/18/6/1…

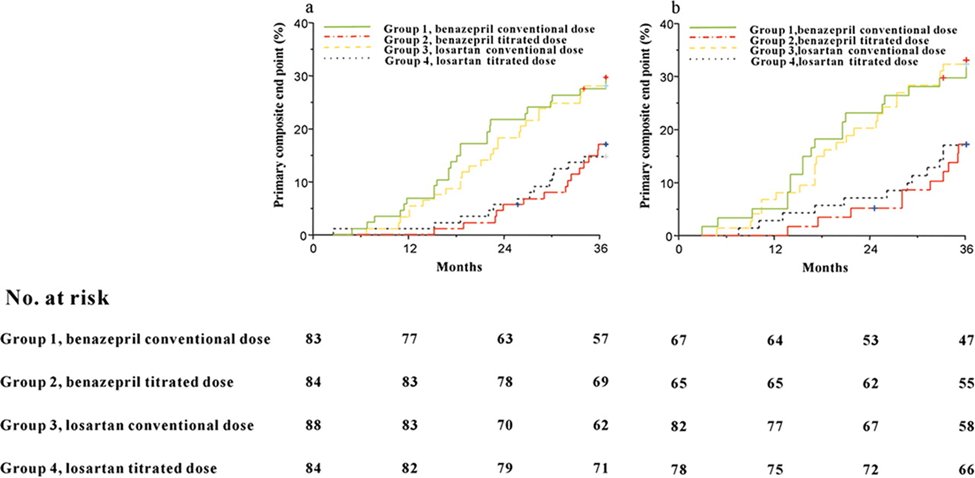
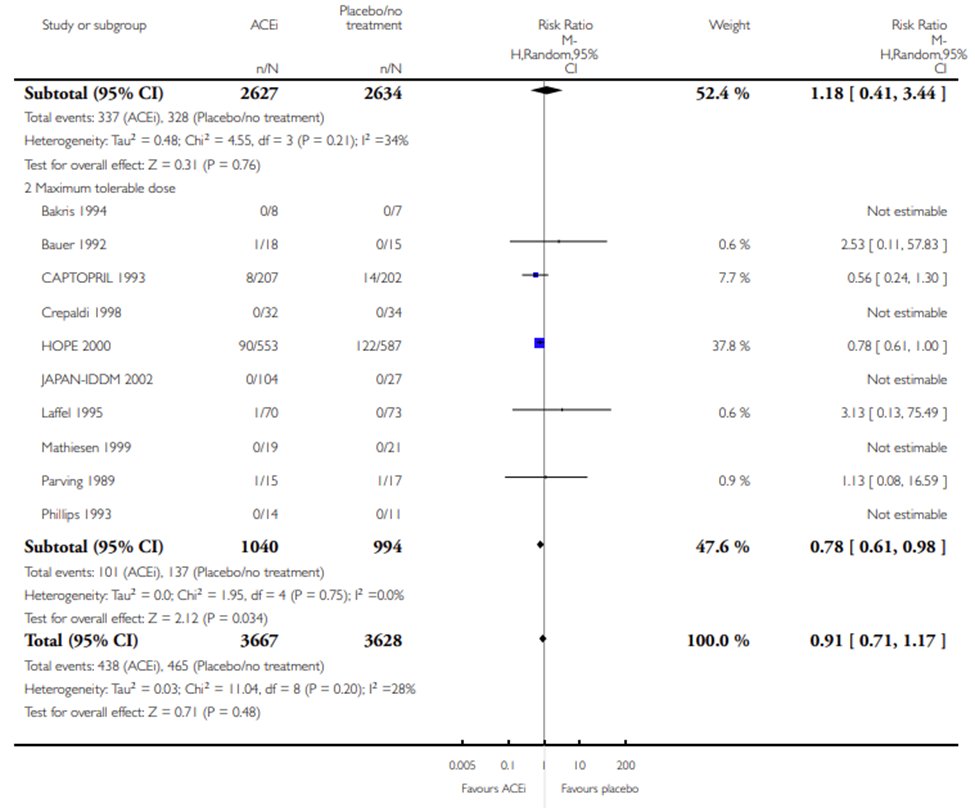
37) In meta-analyses, individualized maximization of the dose of the ACEi or ARB is associated with 22% ⬇️mortality in patients with #T2D against standard doses.
cochranelibrary.com/cdsr/doi/10.10…
cochranelibrary.com/cdsr/doi/10.10…
38) Wrapping up the case of our patient w/ #T2D, she is at high risk for #CKD progression because of:
✔️residual albuminuria
✔️low eGFR
✔️submaximal dose of lisinopril
✔️prior AKI
What if albuminuria persists after⬆️lisinopril or if the patient can't tolerate the higher dose?
✔️residual albuminuria
✔️low eGFR
✔️submaximal dose of lisinopril
✔️prior AKI
What if albuminuria persists after⬆️lisinopril or if the patient can't tolerate the higher dose?
39) Patients with residual albuminuria while maxed on an inhibitor of the Renin Angiotensin System need additional therapies to⬇️their increased #CKD progression risk.
Which class of drugs have NOT yet been approved by @US_FDA for nephroprotection for such patients?
Which class of drugs have NOT yet been approved by @US_FDA for nephroprotection for such patients?
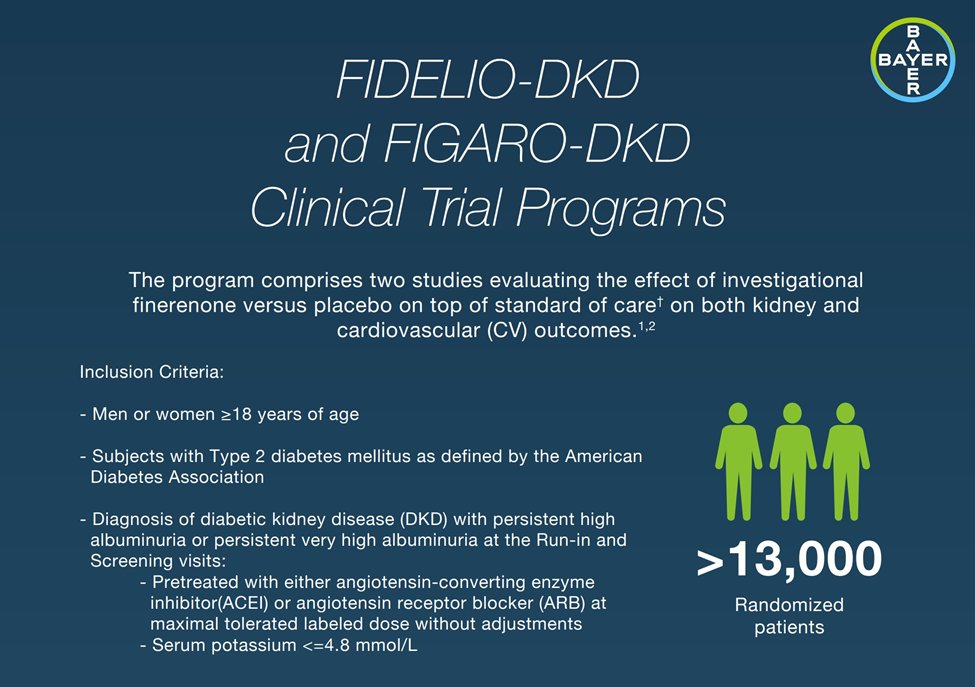
40) To date, #SGLT2i #flozins (#canagliflozin and #dapagliflozin) and novel, nonsteroidal #MRAs (#finerenone) have been approved as nephroprotective agents by enrolling patients with residual albuminuria, depressed eGFR on maximally tolerate doses of ACEis/ARBs. 




41) Despite the high baseline renal risk (pts were albuminuric on maxed ACEi/ARB), #SGLT2i & nonsteroidal #MRA materially⬇️the risk for
✔️#CKD progression
✔️#ESKD
✔️#cardiovascular mortality
✔️hospitalization for heart failure
@Nephjc for maintaining the visual abstracts!



✔️#CKD progression
✔️#ESKD
✔️#cardiovascular mortality
✔️hospitalization for heart failure
@Nephjc for maintaining the visual abstracts!




42) Take-home Points 1⃣:
💡Albuminuria (pre therapy, or residual after initiation of inhibitors of the Renin Angiotensin system) predicts risk for #CKD progression in pts w/ #T2D
✔️risk tools (KDIGO heatmap/KRFE) to visualize & quantitate risk when communicating with patients
💡Albuminuria (pre therapy, or residual after initiation of inhibitors of the Renin Angiotensin system) predicts risk for #CKD progression in pts w/ #T2D
✔️risk tools (KDIGO heatmap/KRFE) to visualize & quantitate risk when communicating with patients
43) Take-home Points 2⃣:
✔️Albuminuria (UACR in FMV) in pts before & after initiating tx w/ inhibitors of the Renin Angiotensin System
👉Patients w/ residual albuminuria after maxing RASi need further therapy to⬇️#CKD risk: #SGLT2i/#flozin & nonsteroidal MRA (finerenone)
✔️Albuminuria (UACR in FMV) in pts before & after initiating tx w/ inhibitors of the Renin Angiotensin System
👉Patients w/ residual albuminuria after maxing RASi need further therapy to⬇️#CKD risk: #SGLT2i/#flozin & nonsteroidal MRA (finerenone)
44) And with that, you just earned 0.5hr CE/#CME! #physicians #physicianassociates #nursepractitioners #nurses #pharmacists Go to ckd-ce.com/dkd5/ to claim it. I am @ChristosArgyrop. FOLLOW US here & on @cardiomet_ce for more programs by expert authors in this space!
44) And with that, you just earned 0.5hr CE/#CME! #physicians #physicianassociates #nursepractitioners #nurses #pharmacists Go to ckd-ce.com/dkd5/ to claim it. I am @ChristosArgyrop. FOLLOW US here & on @cardiomet_ce for more programs by expert authors in this space!
• • •
Missing some Tweet in this thread? You can try to
force a refresh