1/ Understanding Obesity Pathophysiology Through Outcomes:
IMO, the limitations of these surrogate measures (fMRI & PET), make outcome studies a more reliable insight for understanding obesity mechanisms.
A [thread] on outcomes for clinical interventions for obesity. 🧵
IMO, the limitations of these surrogate measures (fMRI & PET), make outcome studies a more reliable insight for understanding obesity mechanisms.
A [thread] on outcomes for clinical interventions for obesity. 🧵
https://twitter.com/TheMooreLab/status/1505419727593689090
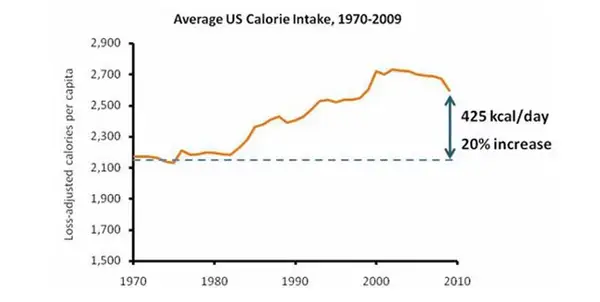
2/ Do Diets Matter? Yes and No. They matter because you have to eat, and you want to do so in a way that promotes health. But, are they reliable txs for obesity? No. Meta-analysis of long-term RCTs (avg wt loss 0-4 kg). Most intensive diet interventions result in 3-5% wt loss. 

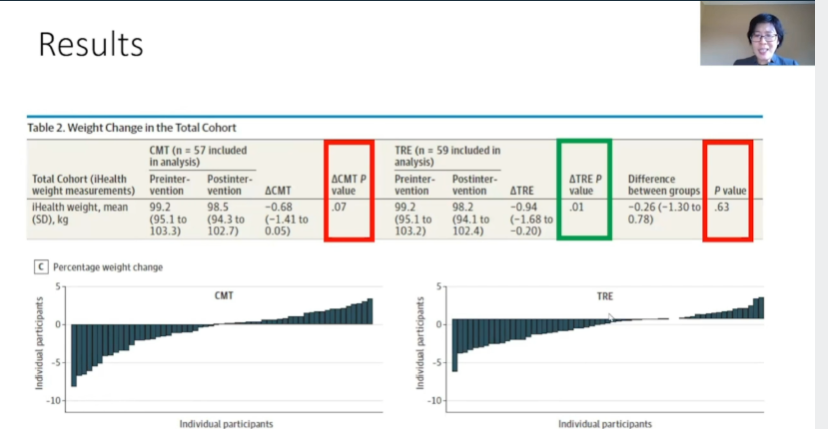
3/ But...but...what about low carb? Mind you, I am talking about population averages. There will always be a level of precision that will be difficult to capture in studies. Most intervention studies have outcomes representing a waterfall plot where results are variable. 

4/ If you compare different carb ranges, there are no clinically meaningful differences in wt outcomes. Btw, David Ludwig was an author of a MA #1 that showed LC diets result in 1.15 kg more weight loss than LF, not clinically meaningful!!!! ⬇️
1) pubmed.ncbi.nlm.nih.gov/26527511/
2)
1) pubmed.ncbi.nlm.nih.gov/26527511/
2)
5/ And if you do not believe me or the data, maybe you will listen to the Cochrane Collaboration?
"There is probably little to no difference in wt reduction..up to 2 years' f/u, when OW and OB
participants are randomised to either LC or balanced-carb weight-reducing diets."
"There is probably little to no difference in wt reduction..up to 2 years' f/u, when OW and OB
participants are randomised to either LC or balanced-carb weight-reducing diets."
6/ What about surgery? We have known for quite some time that surgery is the most effective treatment for obesity or obesity + wt-related comorbidities (see below). Long-term wt reduction and comorbidity management are superior for surgery, full stop. 

7/ Don't worry. If you want to learn more, I've done a thread on it; although honestly, surgery has celebrated many new achievements since I published the thread, and I worry it is already outdated.
https://twitter.com/MichaelAlbertMD/status/1354498420187140097?s=20&t=DtAud08UwPIg9a74K2pC8w
8/ For example, bariatric surgery is a superior weight loss intervention for improving liver outcomes and reducing CV disease in patients with pre-existing obesity and biopsy-proven NASH. A great study by
@Ali_Aminian_MD et al.
jamanetwork.com/journals/jama/…
@Ali_Aminian_MD et al.
jamanetwork.com/journals/jama/…
9/ Bariatric surgery reduces the risk of hospitalization and death from #COVID19.
@Ali_Aminian_MD's group has been on 🔥 recently. Great work, guys.
pubmed.ncbi.nlm.nih.gov/34642102/
@Ali_Aminian_MD's group has been on 🔥 recently. Great work, guys.
pubmed.ncbi.nlm.nih.gov/34642102/
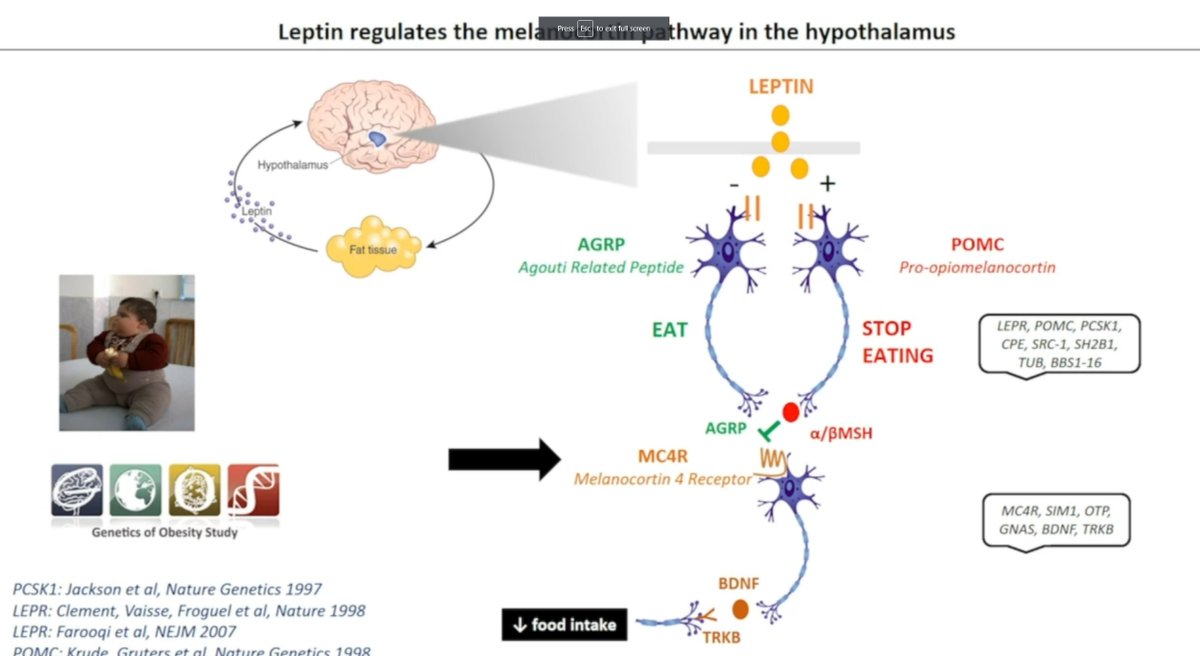
10/ If surgery reliably yields 5-10x better wt loss outcomes in ppl living with OB than diet interventions, shouldn't that tell us something? What is clear to me is that obesity is not a choice. I meet fantastic and committed ppl every day who continue to struggle with their dz.
11/ My favorite example is President Howard Taft. President Taft is the only American to serve as both the Chief Justice of the SC and President of the US. He, by every measure, was incredibly successful. However, despite his successes, he struggled w OB his whole life. 

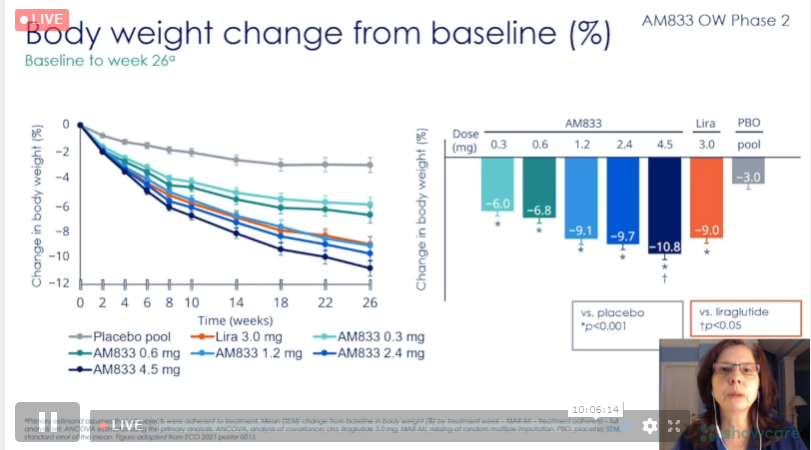
12/ But surgery does not scale at a population level, nor will everyone want it or qualify. Well, there are medications. How do they work? They modify neuronal activities in the appetite centers of the brain, making it easier to achieve sustainable wt loss and health. 

13/ Historically, medications had a lot more side effects and resulted in only 2-3x better results than diet and exercise. 

14/ But, with novel therapies like incretin-based treatments in development and the appreciation for combination approaches, I truly believe the sky is the limit. Here is my coverage of some of these novel therapies from last year: twitter.com/MichaelAlbertM Also, STEP trials!!! 

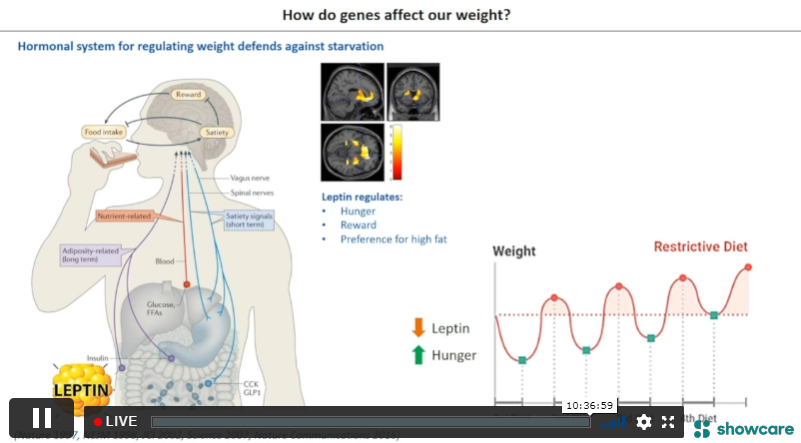
15/ So, where does that leave us? How do outcomes inform pathology and underlying mechanisms?
30+ years of research demonstrate that obesity is centered in the 🧠. This is further reinforced by outcomes that describe effective treatments as those that target neurobiology.
30+ years of research demonstrate that obesity is centered in the 🧠. This is further reinforced by outcomes that describe effective treatments as those that target neurobiology.
16/ Semaglutide reduces eating, decreases cravings & wanting, and IMPROVES SELF-EFFICACY (better control over eating beahvior and less preference for high-fat foods). Maybe it isn't one's fault after all? ncbi.nlm.nih.gov/labs/pmc/artic…
16/ If obesity was as trivial as a willpower problem, then reinforcing self-efficacy should fix it, right? Wrong. Meta-analyses of such interventions demonstrate meager results (avg -1.71 kg weight loss). pubmed.ncbi.nlm.nih.gov/29698017/
17/ 3rd wave CBT only provides a marginal improvement on existing strategies and still pales in comparison to treatments that target the neurobiology of obesity and bodyweight regulation. pubmed.ncbi.nlm.nih.gov/32181957/
18/ In summary, helping support behavior change and lifestyle, while reinforcing self-efficacy is important, but will not solve obesity. All we have to do is look at the long-term outcome data.
19/ That means telling people to vary their diets and a number of fancy ways won't make that much of a difference.
20/ This does leave open the possibility, on an individual level that some people may experience significant benefit from these strategies. Remember the waterfall? But this will be rare. 

21/ And given the discrepancy in the magnitude of these results, this should tell us something. Frankly, it's what 30+ years of obesity research have told us, it's all about the 🧠. Treatments that target these subcortical pathways and neurobiology will be more effective.
22/ That in fact, behavior is impacted by these treatments because behavior is strongly influenced by neurobiology. 🤯 [end]
Oops, Twitter messed up the link. Here it is:
https://twitter.com/MichaelAlbertMD/status/1455320751221903363?s=20&t=DtAud08UwPIg9a74K2pC8w
• • •
Missing some Tweet in this thread? You can try to
force a refresh