1) Welcome to our #accredited #tweetorial on optimal mgt of #hyperkalemia in the patient with #CKD. Earn 0.5h #CME/CE credit by following this thread. I am Sourabh Sharma MD DNB FASN 🇮🇳 @iamnephrologist & u have found the ONLY source for CE credit delivered entirely on Twitter!
2) This program is supported by educational grants from AstraZeneca and Bayer & is intended for #healthcare providers. See faculty disclosures ckd-ce.com/disclosures/. Educational credit for #physicians #physicianassociate #nurses #nursepractitioners #pharmacists 🇺🇸🇨🇦🇪🇺🇬🇧
3) Potassium was first isolated by Humphry Davy in 1807 by electrolysis (Coined word from “Potash” [Dutch]). The periodic table symbol K was derived from kali (alkali) [Arabic].
en.wikipedia.org/wiki/Potassium
#NephroNotes #NephPearls #FOAMed #MedEd @MedTweetorials #CardioTwitter
en.wikipedia.org/wiki/Potassium
#NephroNotes #NephPearls #FOAMed #MedEd @MedTweetorials #CardioTwitter

4) Re potassium #homeostasis: 98% of the body's K lies in intracellular space➡️ helping determine resting membrane potential & intracellular electronegativity.
10% of K secretion is via the colon (↑significantly in advancing CKD) 🔓kidney360.asnjournals.org/content/1/1/65 #NephroNotes
10% of K secretion is via the colon (↑significantly in advancing CKD) 🔓kidney360.asnjournals.org/content/1/1/65 #NephroNotes

5) There is debate abt the definition of hyperK (>5? >5.5?), but it is classified by serum K & ECG. Mortality risk is independent of symptoms, but not ECG findings, as bradycardia/junctional rhythm/QRS widening→Poor outcome.
🔓kidney-international.org/article/S0085-…
🔓mayoclinicproceedings.org/article/S0025-…

🔓kidney-international.org/article/S0085-…
🔓mayoclinicproceedings.org/article/S0025-…


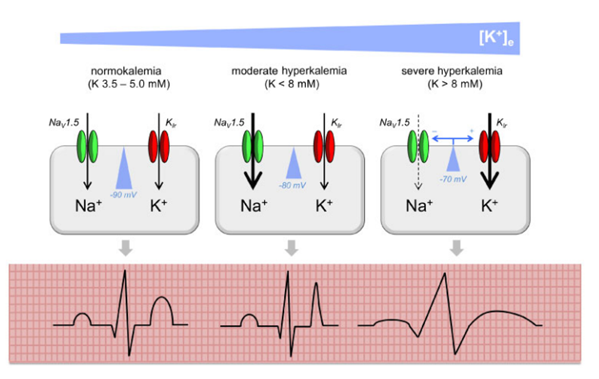
6) Arrhythmia in Hyperkalemia
Moderate HyperK: Fast Na channel activation; ↑excitability/conduction velocity: Peaked T
Severe HyperK: Fast Na channel inactivation/Inwardly rectifying K channel activation: Wide QRS/Conduction block
🔓academic.oup.com/ndt/article/34…
Moderate HyperK: Fast Na channel activation; ↑excitability/conduction velocity: Peaked T
Severe HyperK: Fast Na channel inactivation/Inwardly rectifying K channel activation: Wide QRS/Conduction block
🔓academic.oup.com/ndt/article/34…
7) There are multiple causes of #hyperkalemia:
a. Pseudohyperkalemia
b. Redistribution
c. Excess intake
d. Impaired renal K secretion
In #CKD, relative risk of hyperK approximately doubles for every⬇️in eGFR of 15 mL/min
🔓ccjm.org/content/84/12/…
#NephroNotes #NephPearls #MedEd
a. Pseudohyperkalemia
b. Redistribution
c. Excess intake
d. Impaired renal K secretion
In #CKD, relative risk of hyperK approximately doubles for every⬇️in eGFR of 15 mL/min
🔓ccjm.org/content/84/12/…
#NephroNotes #NephPearls #MedEd

8) Because it may be unexpected, we must be especially cautious of drug-induced hyperkalemia
🔓academic.oup.com/ndt/article/34…
#NephroNotes #NephPearls #FOAMed #MedEd
🔓academic.oup.com/ndt/article/34…
#NephroNotes #NephPearls #FOAMed #MedEd

9) So let's focus on #hyperkalemia in #CKD ➡️adverse outcomes, as it restricts RAASi & MRA usage. #CKD patients have multiple risk factors for hyperkalemia. For those on dialysis, long interdialytic gap ⬆️hyperkalemia chances
nature.com/articles/nrnep…
#NephroNotes #NephPearls
nature.com/articles/nrnep…
#NephroNotes #NephPearls

10) This table is a nice summary of causes and treatment of hyperkalemia across continuum of kidney function, from 🔓cjasn.asnjournals.org/content/13/1/1…
#NephroNotes #NephPearls #FOAMed #MedEd
#NephroNotes #NephPearls #FOAMed #MedEd

11) A low-K diet is generally recommended in advanced #CKD, but @goKDIGO suggests interventional trials to determine optimal recommendations, as there is no direct evidence to link dietary K & serum K, and the benefits of K can’t be ignored
🔓kidney360.asnjournals.org/content/1/1/65
#NephroNotes
🔓kidney360.asnjournals.org/content/1/1/65
#NephroNotes

12) Guidelines for use of #RAAS inhibitors are intertwined with K homeostasis. Strive for maximum tolerated RAASi therapy! Treat hyperkalemia & reinitiate RAASi after resolution, then reassess K level within 1 wk
🔓ccjm.org/content/84/12/…
🔓mayoclinicproceedings.org/article/S0025-…
#NephPearls

🔓ccjm.org/content/84/12/…
🔓mayoclinicproceedings.org/article/S0025-…
#NephPearls


13) Patient education is🔑:
@NKF recommends⬆️patient awareness of hyperK
👉Educational tools
👉Lifestyle change
👉Dietary modification
👉Campaigns
👉Involve allied healthcare professionals
Hyperkalemia is often asymptomatic; regular K monitoring needed!
🔓kidney.org/atoz/content/h…

@NKF recommends⬆️patient awareness of hyperK
👉Educational tools
👉Lifestyle change
👉Dietary modification
👉Campaigns
👉Involve allied healthcare professionals
Hyperkalemia is often asymptomatic; regular K monitoring needed!
🔓kidney.org/atoz/content/h…


14) The National Institute for Health and Care Excellence #NICE offers a systematic Treatment Approach to #hyperkalemia
👉Account for clinical priorities
👉↓variability
👉improve pt outcome
👉↓adverse events
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd

👉Account for clinical priorities
👉↓variability
👉improve pt outcome
👉↓adverse events
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd
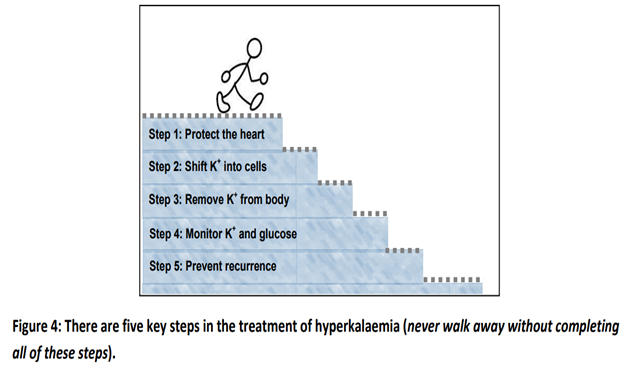

15) So when hyperK happens, how is it treated? Acutely:
👉IV calcium ↓cardiac membrane excitation (1-3 min)
👉Insulin/glucose & β agonist redistribute K to ICS (30-60 min) but not ↓total body K
👉β Agonists: short duration of effect (2-4hrs)
👉Sodium bicarbonate ↑K elimination
👉IV calcium ↓cardiac membrane excitation (1-3 min)
👉Insulin/glucose & β agonist redistribute K to ICS (30-60 min) but not ↓total body K
👉β Agonists: short duration of effect (2-4hrs)
👉Sodium bicarbonate ↑K elimination
16) #Hemodialysis increases total K elimination & is used for resistant acute hyperkalemia
🔓mayoclinicproceedings.org/article/S0025-…
#NephroNotes #NephPearls #FOAMed #MedEd
🔓mayoclinicproceedings.org/article/S0025-…
#NephroNotes #NephPearls #FOAMed #MedEd

17) So among acute treatment options, different medications have rapid, intermediate or delayed onset of action
Rapidly & intermediately acting medications are required in acute hyperkalemia management
🔓pubmed.ncbi.nlm.nih.gov/23882341/
#NephroNotes #NephPearls #FOAMed #MedEd
Rapidly & intermediately acting medications are required in acute hyperkalemia management
🔓pubmed.ncbi.nlm.nih.gov/23882341/
#NephroNotes #NephPearls #FOAMed #MedEd

18) So let's look at drug administration & safety of different emergency use medications
IV Calcium preparation
👉Calcium Chloride
👉Calcium Gluconate
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls

IV Calcium preparation
👉Calcium Chloride
👉Calcium Gluconate
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls


19) Insulin/Glucose Infusion: Consider
👉Drug administration & safety
👉Alternative glucose preparations
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd

👉Drug administration & safety
👉Alternative glucose preparations
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd


20) #Salbutamol: Drug administration & safety
Effective but more likely to produce side effects
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd
Effective but more likely to produce side effects
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd

21) So now let's look at oral potassium binders, which are more useful in chronic mgt & can help facilitate #RAASi optimization. Which of the following binders has the most rapid onset of action after oral administration?
22) Mark your best response & return TOMORROW for the correct answer and the remainder of this program! 👏to @sibgokcay @dr_nikhilshah @kdjhaveri @proychaudhuryMD @divyaa24 @arvindcanchi @priti899 @vjha126 @nephprasad @Gawad_Nephro @SmeetaSinha @Priyasinghbmc @Joe_Vassalotti
23) Welcome back! I am @iamnephrologist and we're talking about #hyperkalemia in #CKD and what to do about it! You are earning🆓CE/#CME, #physicians #physicianassistants #nursepractitioners #pharmacists #nurses. Shout-outs to @vipvargh @gudnephron @SwastiThinks @docanjuyadav 

24) We were about to start talking about the oral K binders. (BTW earn MORE CE/#CME on this topic at cardiometabolic-ce.com/category/hyper…) Yes, prune juice is a K binder, but it's not quick, & it may make a bigger mess than Na polystyrene sulfonate. So the correct answer was D. More to learn!
25) So these oral potassium binders are to be considered in chronic #hyperkalemia despite diuretic therapy/corrected metabolic acidosis. They potentially allow continuation/optimization of RAASi/ MRA
🔓mayoclinicproceedings.org/article/S0025-…
#NephroNotes #NephPearls #FOAMed #MedEd
🔓mayoclinicproceedings.org/article/S0025-…
#NephroNotes #NephPearls #FOAMed #MedEd
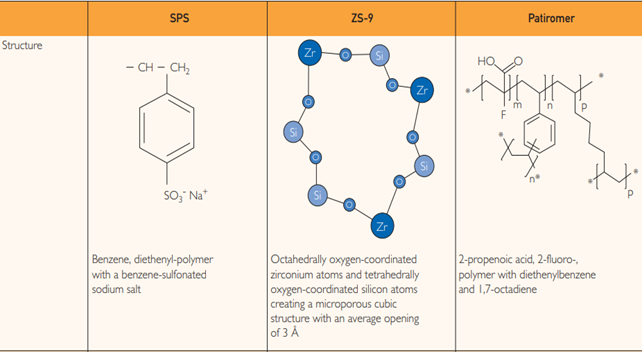
26) So in the K binder🌎, there is old and there is new.
New binders have opened new horizons for treatment & prevention of hyperkalemia
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd
New binders have opened new horizons for treatment & prevention of hyperkalemia
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd
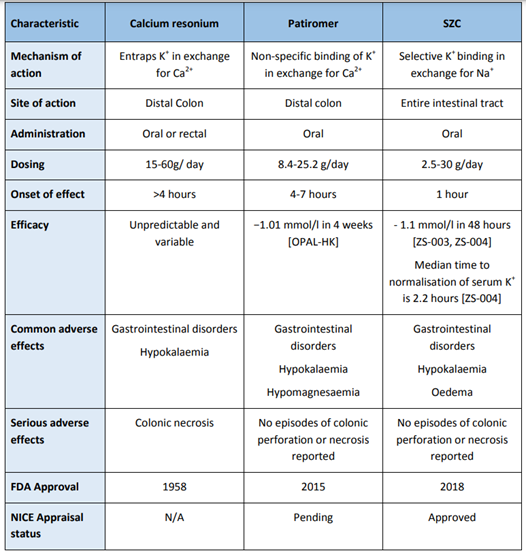
27) Start w/the old. Sodium/Calcium Polysterene Sulfonate clinical studies:
👉Limited evidence for effectiveness/safety
👉With sorbitol, can cause colonic necrosis
👉Nonselective for K, with affinity for Ca/Mg ions
👉Caution: Na & volume overload
🔓frontiersin.org/articles/10.33…
👉Limited evidence for effectiveness/safety
👉With sorbitol, can cause colonic necrosis
👉Nonselective for K, with affinity for Ca/Mg ions
👉Caution: Na & volume overload
🔓frontiersin.org/articles/10.33…

28) And then the new. First, #patiromer sorbitex calcium clinical studies:
👉Efficacy established in randomized, placebo-controlled, phase 2 and 3 trials (CKD/ HF/RAASi)
👉Onset of action~ 7 hours
👉No serious AEs
🔓frontiersin.org/articles/10.33…
#NephPearls #FOAMed #MedEd
👉Efficacy established in randomized, placebo-controlled, phase 2 and 3 trials (CKD/ HF/RAASi)
👉Onset of action~ 7 hours
👉No serious AEs
🔓frontiersin.org/articles/10.33…
#NephPearls #FOAMed #MedEd

29) Sodium Zirconium Cyclosilicate (#SZC) clinical studies:
👉Efficacy & safety established in Ph 2 & 3 trials (#CKD/#HF/#DM/#RAASi)
👉assoc'd w/ ↑Bicarbonate
👉High selectivity for K & ammonium ions
👉fast onset, starts in small bowel
👉No serious AEs
🔓frontiersin.org/articles/10.33…
👉Efficacy & safety established in Ph 2 & 3 trials (#CKD/#HF/#DM/#RAASi)
👉assoc'd w/ ↑Bicarbonate
👉High selectivity for K & ammonium ions
👉fast onset, starts in small bowel
👉No serious AEs
🔓frontiersin.org/articles/10.33…

30) Summary: Clinical trials of oral potassium binders
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd
🔓ukkidney.org/sites/renal.or…
#NephroNotes #NephPearls #FOAMed #MedEd

31) Treatment of #Hyperkalemia in #hemodialysis patients:
👉Hyperkalaemia contributes to mortality in HD (3-5% deaths)
👉K ⤴️is most common immediately post 3-day weekend break
👉Adjust dialysate K as per 🔓ukkidney.org/sites/renal.or…

👉Hyperkalaemia contributes to mortality in HD (3-5% deaths)
👉K ⤴️is most common immediately post 3-day weekend break
👉Adjust dialysate K as per 🔓ukkidney.org/sites/renal.or…


32) In summary, the treatment of hyperkalemia is likely to evolve in the coming years with the availability of novel drugs & the development of new strategies to improve safety. Clinical decisions on when to treat & how aggressively to treat require a pt-centered approach ...
33) ... guided by the clinical setting and rate of change in serum K+ level. Patients with moderate levels of hyperkalemia pose the greatest dilemma, especially when acuity is low, but warrant intervention to avoid deterioration.
34) Severe hyperkalemia risks arrhythmias & cardiac arrest, therefore prompt recognition and intervention is required. How big a problem is it? In-hospital mortality is significantly higher in patients w/ hyperkalaemia (X%) hypokalaemia (Y%) vs normokalaemia (Z%). What are X,Y,Z?
35) Per NICE guidelines, the correct answer is B, more exactly hyperkalemia (18.1%) compared to those with hypokalemia (5.0%) or normokalemia (3.9%). Pts with severe hyperK (> 6.5 mmol/l) are most at risk & in one report (🔓pubmed.ncbi.nlm.nih.gov/23171442/ ), hospital mortality was 30.7%.
36) And that's it! You made it! Go grab your CE/#CME certificate at ckd-ce.com/foundations_hy…. I am @iamnephrologist and I hope you'll FOLLOW @ckd_ce AND @cardiomet_ce for more #accredited #tweetorials from expert authors all over the 🌎🌍🌏!
• • •
Missing some Tweet in this thread? You can try to
force a refresh