
A brief thread on the #dermatologic exam for #monkeypox!
Caveat: I myself have not seen a MPX patient, but am piecing information together for my #dermtwitter and #medtwitter colleagues!
#MedEd #FOAMEd #tweetorial
PC:npr.org/sections/goats…
1/
Caveat: I myself have not seen a MPX patient, but am piecing information together for my #dermtwitter and #medtwitter colleagues!
#MedEd #FOAMEd #tweetorial
PC:npr.org/sections/goats…
1/

Since #Monkeypox seems to transition from:
Macules ➡️ Papules ➡️ Vesicles ➡️ Pustules
The primary lesion isn't enough to make the diagnosis. You're going to need the primary lesion AND time from rash onset to know what you should be expecting to see.
2/
Macules ➡️ Papules ➡️ Vesicles ➡️ Pustules
The primary lesion isn't enough to make the diagnosis. You're going to need the primary lesion AND time from rash onset to know what you should be expecting to see.
2/
The prodrome that occurs before the rash includes the typical ILI type symptoms of fever, malaise, headache, pharyngitis, and cough. Lymphadenopathy has been billed as a distinguishing feature of MPX from smallpox and Varicella.
3/
3/
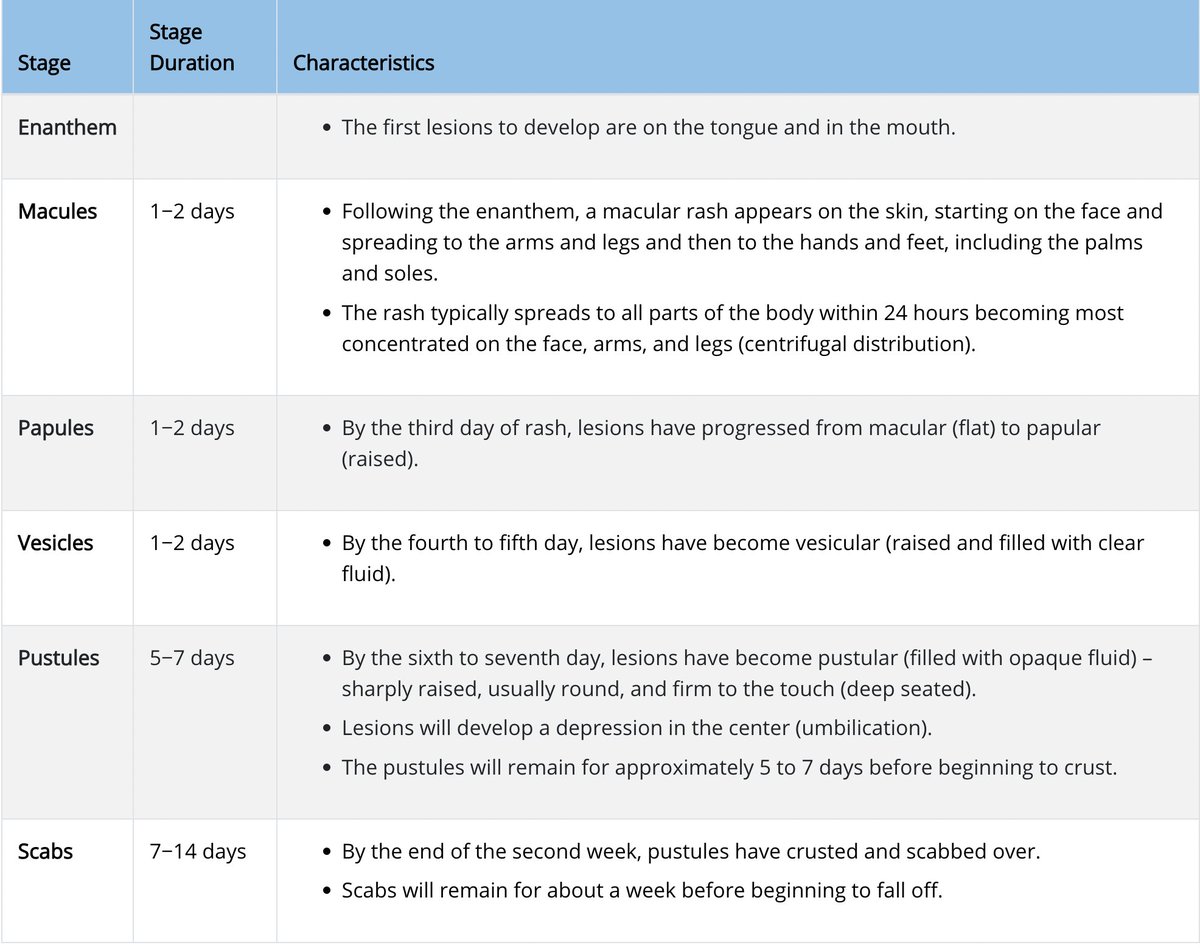
The @CDCgov reports that the dermatologic manifestations start in the mouth and on the tongue. Then progress to the skin after a certain amount of time.
Macules for 1-2 days
Papules for 1-2 days
Vesicles for 1-2 days
Pustules for 5-7 days
Crusted over for 7-14 days
4/
Macules for 1-2 days
Papules for 1-2 days
Vesicles for 1-2 days
Pustules for 5-7 days
Crusted over for 7-14 days
4/
Unlike other viral processes (like VZV) that start on the trunk and move out, MPX starts in the mouth/face and moves down the limbs.
Also, unlike VZV that has lesions in multiple stages, MPX progresses through stages together for each body part.
PC: @dermnetnz, @Medscape
5/

Also, unlike VZV that has lesions in multiple stages, MPX progresses through stages together for each body part.
PC: @dermnetnz, @Medscape
5/


I just wanted to point out this is the perfect example of why #dermatologic training can be so difficult. We train our residents to think horses when they hear hoofbeats, but we as derms have to know the zebras. This is where knowing the zebra can help you diagnose early!
6/
6/
And one final poll for my #dermtwitter nerds: Even though multiple primary morphologies are reported, what do you think is the "true primary morphology" for MPX?
7/
7/
I personally would vote vesicles, because I think the M/P phases are just pre-vesicular, and we always say that any vesicle turns into a pustule after a few days.
That said, I do think it's important to emphasize the macular and papular phases for the sake of early diagnosis!
8/
That said, I do think it's important to emphasize the macular and papular phases for the sake of early diagnosis!
8/
That's it! Since I haven't personally seen a patient, I wanted to stay in my lane and comment on morphology and clinical recognition. I'll leave the broader commentaries to other folks here on #medtwitter.
Stay safe out there!
9/9
Stay safe out there!
9/9
One more thing: the actual vesicle looks a bit herpetic. “Dewdrop on a rose petal” but the dew is pus, and the drop is bigger!
Another observation I’m not certain about (& would ❤️ other opinions)- looks like they don’t cluster like hsv/vzv; they stay relatively discrete!
10/10
Another observation I’m not certain about (& would ❤️ other opinions)- looks like they don’t cluster like hsv/vzv; they stay relatively discrete!
10/10
• • •
Missing some Tweet in this thread? You can try to
force a refresh













