In a new preprint led by @annasimsbiol, we ask:
Why Don’t These Viruses Want to be Friends?
A 🧵...
biorxiv.org/cgi/content/sh…
Why Don’t These Viruses Want to be Friends?
A 🧵...
biorxiv.org/cgi/content/sh…

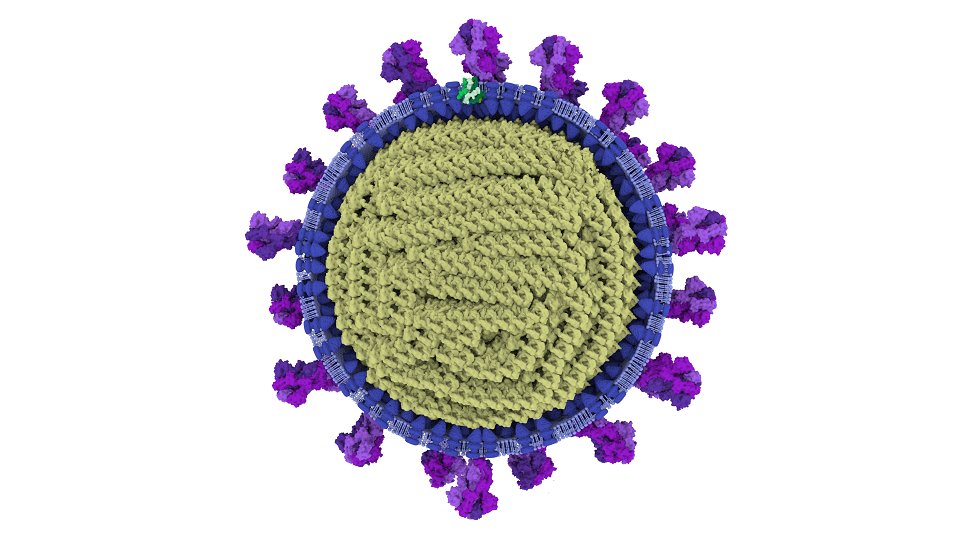
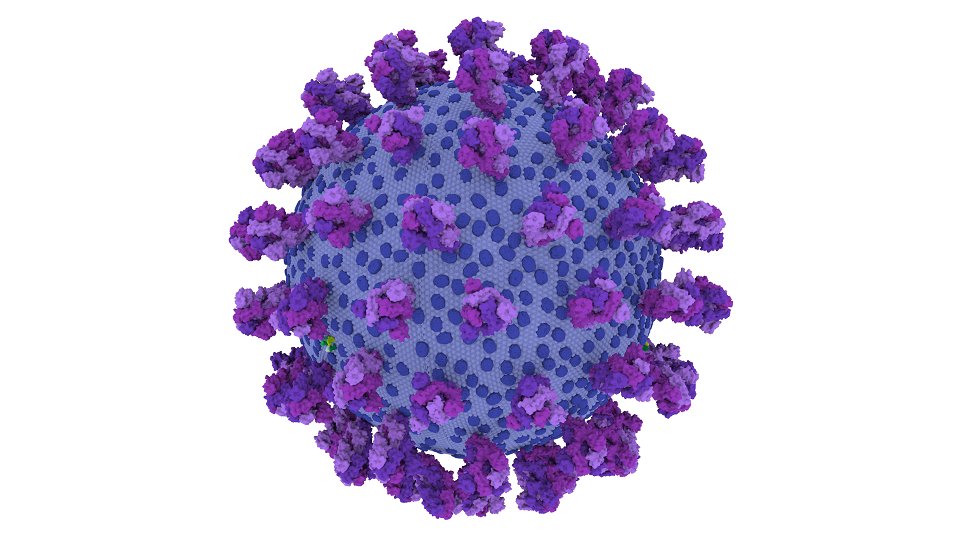
Coinfection is an important aspect of viral evolution. If two viruses can get into the same cell, they can undergo genetic exchange. A dramatic example of this is when different strains of influenza A virus (IAVs) use coinfection to generate novel pandemic strains 

However, many viruses actively push back against coinfection. In a variety of ways, they change an infected cell until it becomes resistant to infection by related viruses. This effect is known as superinfection exclusion (SIE) 

What does this mean for coinfection? In the lab we can set up experiments in which cells are coinfected simultaneously, but the chances of two unrelated viruses actually entering a host organism, and finding exactly the same cell, at exactly the same moment are… slim
Instead, we assume that, for viruses such as IAVs, unrelated viruses first establish separate infections inside a host, and then encounter each other when those infections spread through tissue. How would SIE control these spreading infections?
Following infections inside a living animal is not easy. Instead, we started with cells, using two IAVs that differed only in the colour of a fluorescent tag. SIE by IAV is rapid and early – there is a short window for coinfection, and then the door slams closed, fast 

Next, to observe spread we used everyone's favourite model of virus spread: the #PlaqueAssay. When different spreading viruses meet, or two plaques bump together, coinfection can only occur in a thin boundary of recently-infected cells. Beyond that point, SIE is fully effective 

But what about interactions within a single spreading region? To look at this we needed plaques that started with a mixture of the two viruses. As the mixed plaques spread, would coinfection be maintained, or would the plaques segregate into regions descended from a single virus? 

To set up mixed plaques we coinfected cells simultaneously, dissociated them with trypsin, diluted them, then reseeded them onto new cells so that each coinfected cell was a plaque forming unit. We found… 

… that they stayed well mixed as they spread. This wasn’t the result we expected, but it makes sense – each new cell in a growing plaque can receive plenty of both colours of virus before SIE kicks in 

This is all very well and good, but is it just a cell culture artefact? Plaque assays are not lungs, after all.
So we infected mice with both viruses…
So we infected mice with both viruses…

… and found that once lesions had grown there were clear boundaries between the two colours inside the same anatomical compartments. So it seems SIE can impose its patterns inside a host as well as in a dish 

What does this mean?
•Within a host IAV naturally partitions into a landscape of microdomains
•Within domains genetic exchange is maintained but between them it is inhibited
•Because it relies on kinetics, rather than a specific mechanism, this could apply for many viruses
•Within a host IAV naturally partitions into a landscape of microdomains
•Within domains genetic exchange is maintained but between them it is inhibited
•Because it relies on kinetics, rather than a specific mechanism, this could apply for many viruses

Things not in the paper but worth mentioning.
This project was triggered by two ideas:
(1) listening to #TWiV while lagging the loft, I heard about this cool paper and thought ‘I wonder if flu does that?’ (it probably doesn't, but...)
pubmed.ncbi.nlm.nih.gov/30318351/
This project was triggered by two ideas:
(1) listening to #TWiV while lagging the loft, I heard about this cool paper and thought ‘I wonder if flu does that?’ (it probably doesn't, but...)
pubmed.ncbi.nlm.nih.gov/30318351/
... and (2) after a seminar in which I carelessly claimed cells inside a host would get coinfected all the time, @Digs66768072 asked the best and most annoying question in science, which is of course
‘… but why do you think that’s true?’
(It was not true)
‘… but why do you think that’s true?’
(It was not true)
Many thanks here: to #LauraBurgessTornaletti, @snjasim, @chiara_pirillo, #RyanDevlin, @jack__stat, @Onlycloney, @jowojtus, @DrLizSloan, @lukethorley96, #ChrisBoutell and #EdRoberts, to the rest of team @CVRHutchinson…
• • •
Missing some Tweet in this thread? You can try to
force a refresh