Final session :: Lisanne Roesthuis and Annemijn Jonkman - Lung uss. What’s the thickness of diaphragm
Goal / make it comparable - 1. Patient position : supine or semi recumbent 2.probe selection : cardiac probe. 3. Measurements : thickening fraction 4. But if ventilated then it’s harder to separate pt v machine #LIVES2022 #ventilation #POCUS @ESICM
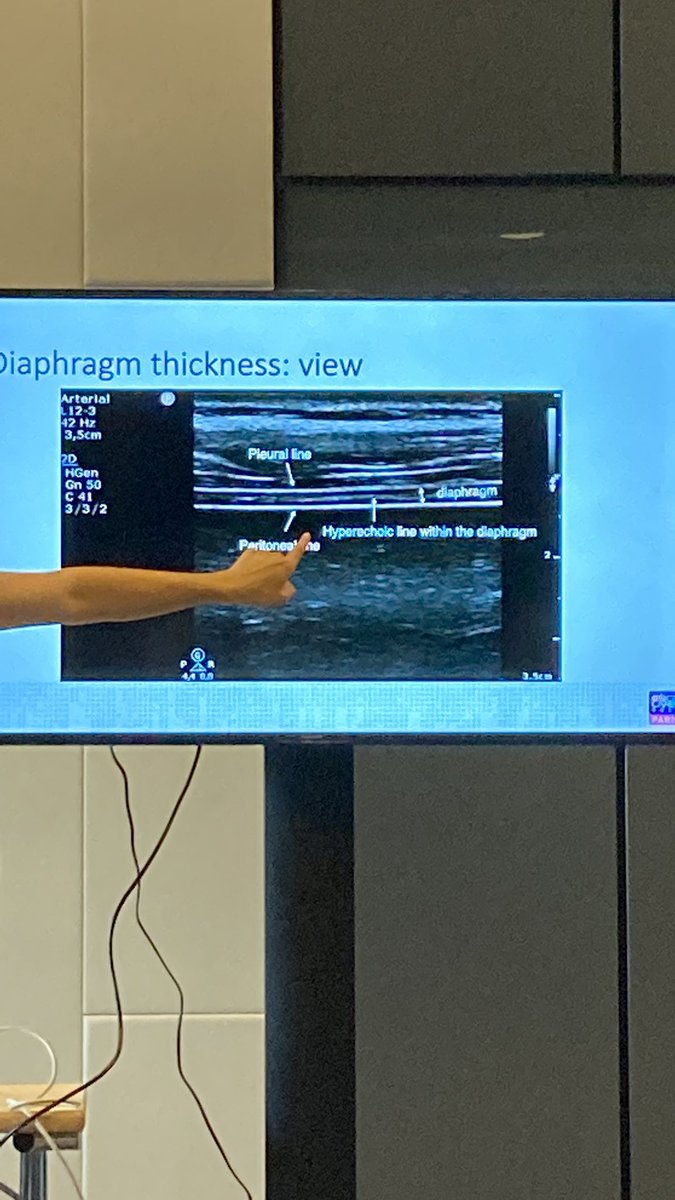
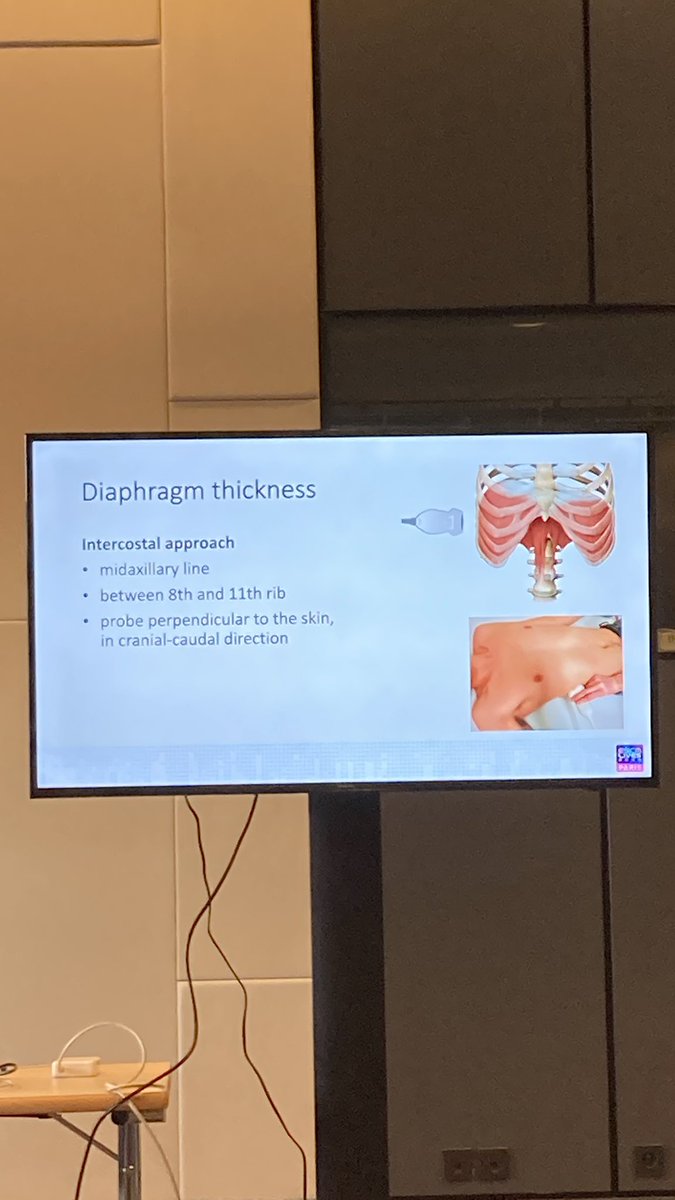
Measure in the zone of apposition. I.E., lung needs to be sliding in and out -> can be tricky to acquire. Intercostal approach. Mid. Axillary line. Perpendicular to skin. Audience : difficult to obtain views. But perhaps shorter learning curve than echo 👍🤞 
— having ascitic fluid or pleural fluid doesn’t change the measurements. Measure “end expiratory thickness” when there’s no activity. Measure for 3 breaths and average. Thickening fraction TFdi = (Tei-Tee)/Tee * 100%. #POCUS #LIVES2022 #ventilation
- “M” mode. Adjust sweep speed to 10mm/s to capture multiple breaths. End expiratory thickness affected by body position + gender. TFdimax < 20% ~ diaphragm weakness. pubmed.ncbi.nlm.nih.gov/26167730/ . If during assist target 15-30%-less than 15% may be over assist
However there’s new paper : potentially poor relation between TFdi and Delta P di. pubmed.ncbi.nlm.nih.gov/34788380/ so questions : TFdi does not = force generation. 2nd ?: does zone of apposition reflects the whole diaphragm ?
To me this is again like using Poes. It reflects central dorsal side more than ventral.
Next : Diaphragm Excursion. Use liver as acoustic window. Diaphragm moves caudally during inspiration I.E., towards probe. M line perpendicular to diaphragm at 10mm/a sweep speed . 
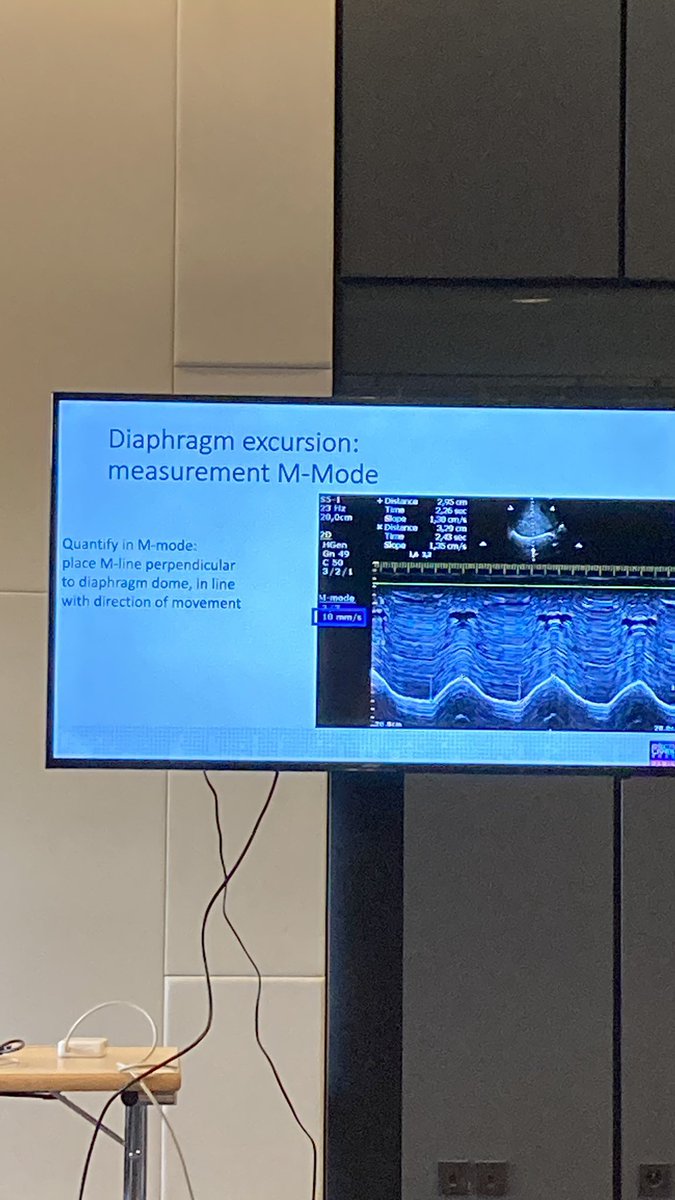
Main question : diaphragm moving caudally or paradoxically ? Diaphragm dysfunction : tidal excursion< 1cm and maximal breath <2.5 cm. Compare L and R. image acquisition of R is easier.
Take home message : uss of diaphragm is non invasive. Useful. Potentially other tools and uses too. E.g., respiratory muscles. See pubmed.ncbi.nlm.nih.gov/32386831/
Question from audience :: what do you with this ? Answer : difficult as need t be in the context of everything. For example Potential consideration for diaphragmatic pacing etc.
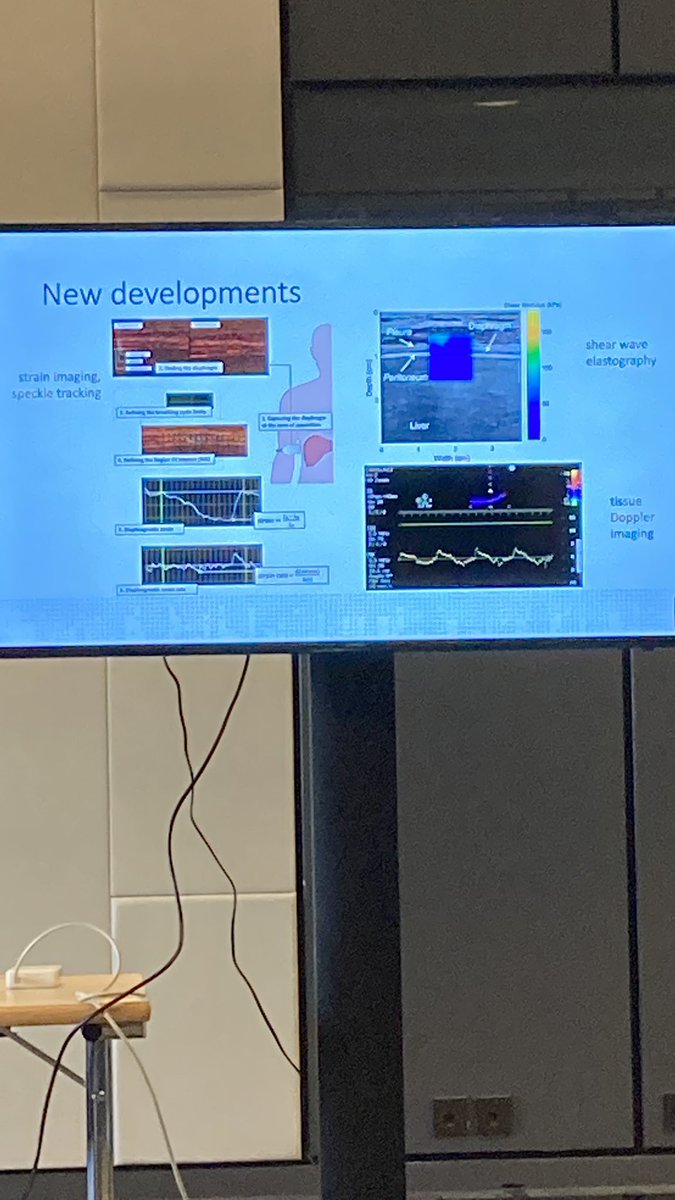
More complex measurements — usually trickle down technology already used in echo - Speckle tracking. But what’s signal to noise ratio. More to think.🤔All in all a very exciting area with potential applications and perhaps transfer learning with ?chest wall nerve blocks , echo 🤓 
• • •
Missing some Tweet in this thread? You can try to
force a refresh