1) Welcome to this #accredited #tweetorial on genetic testing in the evaluation of patients with cystic kidney disease. #Kidney #cysts are a frequent finding, ranging from simple cysts to suspected or confirmed #ADPKD.
Expert author @dguerrot of @CHURouen 🇫🇷 leads us!
Expert author @dguerrot of @CHURouen 🇫🇷 leads us!

2) This program is supported by an educational grant from Otsuka Pharmaceuticals & is intended for #HCPs. #Physicians #Physicianassociates #nurses #nursepractioners #pharmacists 🇺🇸🇨🇦🇪🇺🇬🇧 earn CE/#CME credit. Statement of accreditation & faculty disclosures ckd-ce.com/disclosures
3a) Fortuitous discovery of non-malignant kidney cysts is increasingly frequent with age, and often leads to #nephrology referral.
3b) In this setting, the main concern is accurate differential diagnosis between “simple” cysts without clinical significance and cysts associated with genetic polycystic disorders with renal and/or extrarenal consequences.
See 🔓 pubmed.ncbi.nlm.nih.gov/16941027/

See 🔓 pubmed.ncbi.nlm.nih.gov/16941027/


4a) So let’s start with the case of a 36♀️ patient.
Her personal medical history is unremarkable and she takes no medication. Because of transient abdominal pains, an ultrasound followed by an MRI were performed.
Her personal medical history is unremarkable and she takes no medication. Because of transient abdominal pains, an ultrasound followed by an MRI were performed.
4b) Intraductal papillary mucinous neoplasm of the pancreas was diagnosed and multiple small cysts were fortuitously observed in the cortex and the medulla of both #kidneys. The digestive surgeon calls you for advice… 



5) At this stage, what would you answer regarding the discovery of these kidney cysts ?
A/ ADPKD
B/ ARPKD
C/ Perform genetic testing
D/ Perform additional investigations
A/ ADPKD
B/ ARPKD
C/ Perform genetic testing
D/ Perform additional investigations
6) Multiple disorders can lead to the occurrence of #kidney #cysts, with very different prognostic and therapeutic implications, so the correct answer is D. The following questions are key for differential diagnosis: 

7) Family history was unremarkable. Lab results revealed:
🧪Normal kidney function (CKD-EPI eGFR 110 ml/min/1.73m2)
🧪Low plasma Mg (0.37 mmol/l)
🧪High plasma uric acid (390 µmol/l)
Does this ring a 🔔?
🧪Normal kidney function (CKD-EPI eGFR 110 ml/min/1.73m2)
🧪Low plasma Mg (0.37 mmol/l)
🧪High plasma uric acid (390 µmol/l)
Does this ring a 🔔?

8) Given the presence of multiple bilateral #cysts and characteristic #electrolyte disturbances, #genetic testing was performed. As you may have suspected this patient had a heterozygous deletion of #HNF1beta.
See pubmed.ncbi.nlm.nih.gov/25536396/.
See pubmed.ncbi.nlm.nih.gov/25536396/.
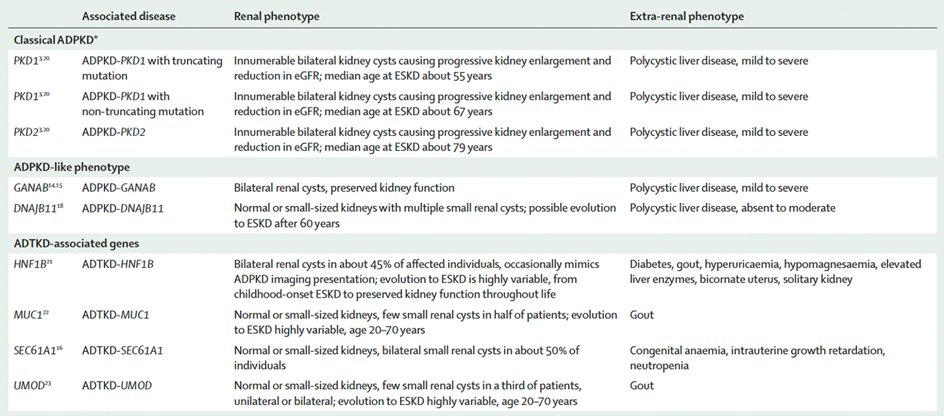
9) #HNF1B #nephropathy is classified as an autosomal dominant tubulointerstitial kidney disease (#ADTKD), along with #MUC_1 and #UMOD, and rarer causes including #SEC61A1 and #DNAJB11.
See pubmed.ncbi.nlm.nih.gov/30819518/ and pubmed.ncbi.nlm.nih.gov/31488840/.

See pubmed.ncbi.nlm.nih.gov/30819518/ and pubmed.ncbi.nlm.nih.gov/31488840/.

10) The clinical #phenotype associated with #HNF1B haploinsufficiency is variable, and extrarenal features, including #MODY diabetes and urogenital tract malformations, are frequently helpful to guide the diagnosis.
See pubmed.ncbi.nlm.nih.gov/31488840/
See pubmed.ncbi.nlm.nih.gov/31488840/

11) More generally, patients with autosomal dominant #tubulointerstitial kidney disease (#ADTKD) present with #kidney #cysts in approximately 50% of cases.
Look at the main features that can help consider ADTKD in the differential diagnosis of kidney cysts:
Look at the main features that can help consider ADTKD in the differential diagnosis of kidney cysts:

12) #ADTKD share common pathophysiological mechanisms, mainly dependent on endoplasmic reticulum stress within tubular epithelial cells
pubmed.ncbi.nlm.nih.gov/31488840/
pubmed.ncbi.nlm.nih.gov/31488840/

13) #DNAJB11 is an example of atypical #ADPKD-#ADTKD phenotype, with normal sized or atrophic kidneys & small cysts.
The tubulo-interstitial nephropathy evolves towards end-stage kidney disease #ESKD in 20% of cases (55-89 years, median age 75).
See 🔓 pubmed.ncbi.nlm.nih.gov/32631624/
The tubulo-interstitial nephropathy evolves towards end-stage kidney disease #ESKD in 20% of cases (55-89 years, median age 75).
See 🔓 pubmed.ncbi.nlm.nih.gov/32631624/

14) While the previous diagnoses are commonly missed since they are rather seldom in general practice, autosomal dominant polycystic kidney disease (#ADPKD) is a frequent hereditary cause of #kidneydisease, present in 1/1000 to 1/2500 individuals. 



15) In #ADPKD, cysts progressively ⬇️the number of functional nephrons ➡️chronic kidney disease (#CKD). In western countries ADPKD accounts for as much as 8 to 10% of the causes of end-stage kidney disease #ESKD #ESRD.
🔓 era-online.org/en/registry/pu…
🔓 academic.oup.com/ndt/article/29…

🔓 era-online.org/en/registry/pu…
🔓 academic.oup.com/ndt/article/29…


16) ADPKD predominantly affects the kidneys, with the progressive onset and growth of numerous cysts.
🔓 pubmed.ncbi.nlm.nih.gov/21079243/
🔓 pubmed.ncbi.nlm.nih.gov/21079243/

17) #ADPKD is also responsible for a large variety of extra-renal manifestations, particularly involving the liver, the digestive tract and the cardiovascular system, as described in this Table from 🔓academic.oup.com/ndt/article/29… 

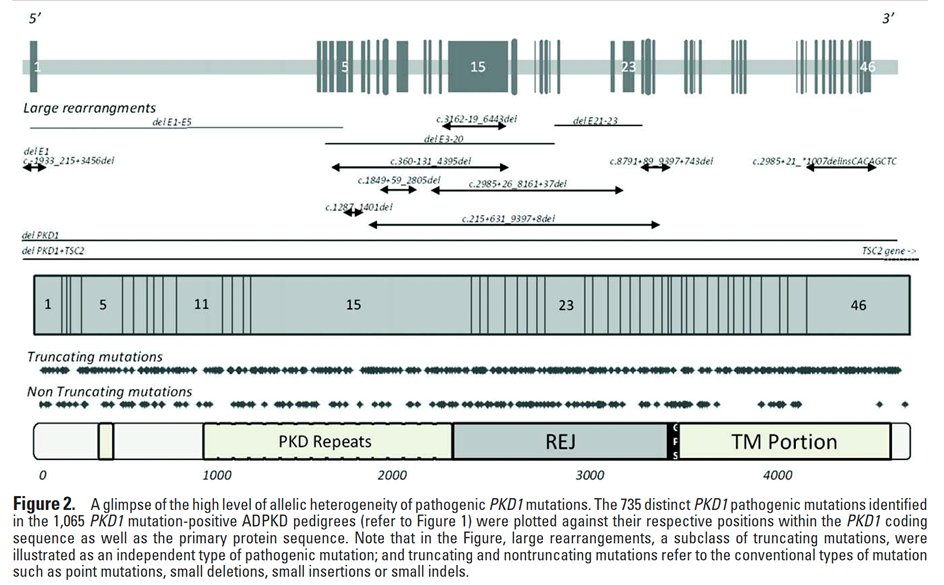
18) In approximately 80% of cases the genetic variations responsible for #ADPKD are located in #PKD1, encoding #polycystin 1. The molecular diagnosis of ADPKD is complicated by the presence of highly homologous sequences of PKD1.
See pubmed.ncbi.nlm.nih.gov/25263802/
See pubmed.ncbi.nlm.nih.gov/25263802/
19) Other genes less frequently involved in #ADPKD or ADPKD-like phenotypes include #PKD2 (encoding #polycystin 2, 15% cases), #GANAB, #DNAJB11, #ALG5, #ALG9, #IFT140, …
See pubmed.ncbi.nlm.nih.gov/30819518/
See pubmed.ncbi.nlm.nih.gov/30819518/

20) As shown in this large study from the #Genkyst cohort the types of mutations found in #PKD1 and #PKD2 are variable.
See pubmed.ncbi.nlm.nih.gov/22508176/

See pubmed.ncbi.nlm.nih.gov/22508176/


21) In kidney epithelial cells, #polycystins 1 and 2 constitute a complex that locates at the cell membrane, predominantly in the primary #cilium, where it regulates Ca2+ influx and cellular signaling, and is thought to contribute to the cellular adaptation to urine flow. 



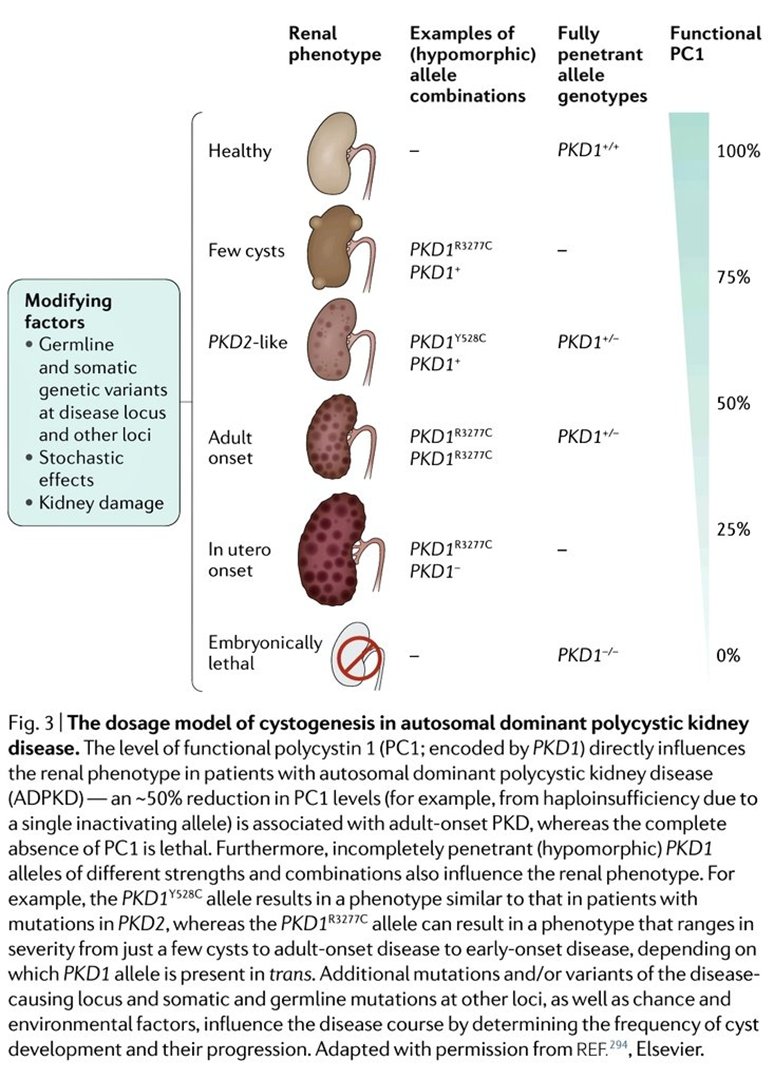
22) The severity of renal phenotype in #ADPKD is highly dependent on the gene involved, the type of genetic variation, & the potential association with additional variants, which all contribute to the level of expression of functional #polycystins.
See 🔓 pubmed.ncbi.nlm.nih.gov/30523303/
See 🔓 pubmed.ncbi.nlm.nih.gov/30523303/
23) The diagnostic value of genetic testing for #ADPKD is particularly important in suspected de novo mutations (negative family history) and in patients with atypical presentations, which are rare taken individually but are cumulatively common.
See 🔓 pubmed.ncbi.nlm.nih.gov/32690722/
See 🔓 pubmed.ncbi.nlm.nih.gov/32690722/

24a) Genetic analysis is indicated in severe renal phenotypes occurring in utero or in early childhood. It can reveal:
👉compound #heterozygosity (2 different mutations in #PKD1)
(cont)
👉compound #heterozygosity (2 different mutations in #PKD1)
(cont)
24b)
👉 #digenic disease (a mutation in #PKD1 associated with a mutation in another gene such as #COL4A1, #HNF1B or #PKD2)
👉 contiguous PKD1/TSC2 deletion
👉 #digenic disease (a mutation in #PKD1 associated with a mutation in another gene such as #COL4A1, #HNF1B or #PKD2)
👉 contiguous PKD1/TSC2 deletion
25) Absence of a ➕family history occurs in 10%-25% of pts w/#ADPKD.
Beyond potentially missing parental records, genetic analyses are useful here as ADPKD may be related to a de novo mutation, a germline or a somatic #mosaicism, or to combined hypomorphic PKD1 & PKD2 mutations.
Beyond potentially missing parental records, genetic analyses are useful here as ADPKD may be related to a de novo mutation, a germline or a somatic #mosaicism, or to combined hypomorphic PKD1 & PKD2 mutations.

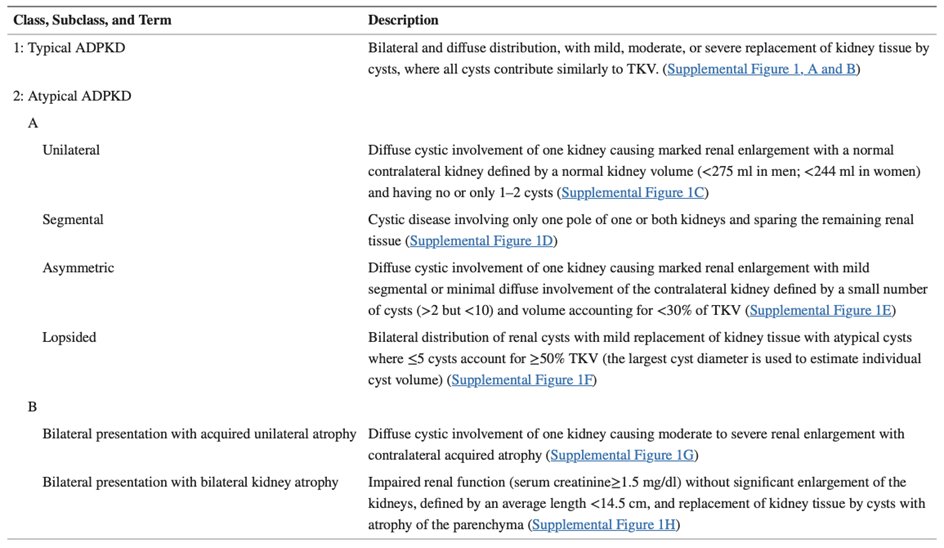
26) 5-10% of #ADPKD pts present w/atypical kidney imaging patterns (Mayo class 2). When FHx is negative, patients w/unilateral, segmental, asymmetric or lopsided cystic kidney dz are suspicious for #somatic #mosaicism.
See 🔓 ncbi.nlm.nih.gov/pmc/articles/P… & 🔓 pubmed.ncbi.nlm.nih.gov/28522688/

See 🔓 ncbi.nlm.nih.gov/pmc/articles/P… & 🔓 pubmed.ncbi.nlm.nih.gov/28522688/

27a) The genetic #mosaicism corresponds to the coexistence of several cellular genetic lineage in the same individual, because of the occurrence of a post zygotic mutation. A mutation may therefore be present in the kidney tissue but not identified . . .
27b) . . . in the DNA extracted from the leukocytes. If the mutation is present in the germline cells, there is a risk of transmission to the descendants of a classical, homogeneous form of #ADPKD.
See pubmed.ncbi.nlm.nih.gov/25424979/.
See pubmed.ncbi.nlm.nih.gov/25424979/.

28) In summary, in which patients with suspected or confirmed #ADPKD should genetic analyses be prioritized?
See 🔓 pubmed.ncbi.nlm.nih.gov/32690722/.
See 🔓 pubmed.ncbi.nlm.nih.gov/32690722/.

29) So let's take a breather here. Please RETURN TOMORROW for the remainder of this program and your link to 🆓CE/#CME!
👏 to @EAE_Elhassanr @DrDanMO @nephrohamzaoui @Carmendemigue12 @fjorios @georgehret @torra_roser @korinapena1 @edgarvlermamd @sophia_kidney @KidneyCathy
👏 to @EAE_Elhassanr @DrDanMO @nephrohamzaoui @Carmendemigue12 @fjorios @georgehret @torra_roser @korinapena1 @edgarvlermamd @sophia_kidney @KidneyCathy
30) WELCOME BACK! I am @dguerrot from @CHURouen 🇫🇷 , we are talking about the utility of #genetic analysis in #ADPKD, and YOU are earning 🆓CE/#CME! Follow @ckd_ce for expert-authored #accredited #tweetorials in the #nephrology space!
#FOAMed #NephTwitter @MedTweetorials
#FOAMed #NephTwitter @MedTweetorials
31) Beyond the diagnostic impact, #genetic analyses in #ADPKD hold important prognostic value for kidney function.
See 🔓 pubmed.ncbi.nlm.nih.gov/32634120/
See 🔓 pubmed.ncbi.nlm.nih.gov/32634120/

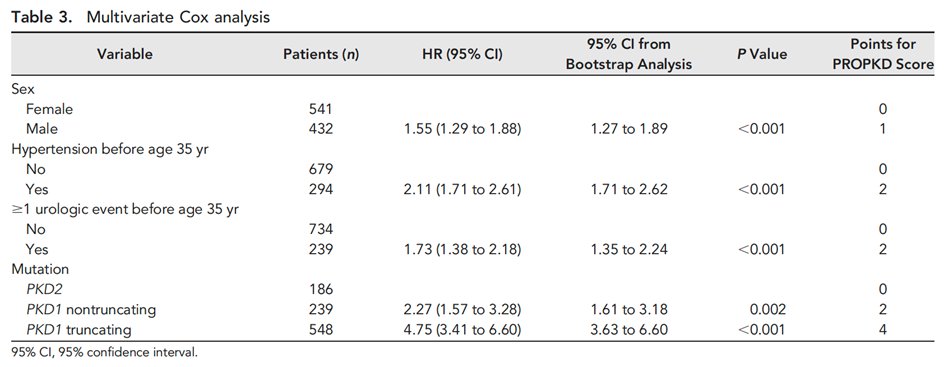
32) This important study from the #Genkyst cohort demonstrated that #PKD1 (vs PKD2) and the type of PKD1 mutation have a strong influence on renal survival. Patients with PKD1 truncating mutations reach #ESKD at a mean age of 55 years old.
🔓 pubmed.ncbi.nlm.nih.gov/23431072/
🔓 pubmed.ncbi.nlm.nih.gov/23431072/

33) The addition of genetic results to classical clinical variables (gender, early hypertension & early urologic events) improves prediction of renal prognosis in #ADPKD. This ➡️establishment of the #PROPKD score
See 🔓 pubmed.ncbi.nlm.nih.gov/26150605/ and 🔓 pubmed.ncbi.nlm.nih.gov/28992127/



See 🔓 pubmed.ncbi.nlm.nih.gov/26150605/ and 🔓 pubmed.ncbi.nlm.nih.gov/28992127/



34) There is a significant genotypic and phenotypic overlap between #ADPKD and autosomal dominant polycystic liver disease (#ADPLD).
See 🔓 pubmed.ncbi.nlm.nih.gov/29038287/
See 🔓 pubmed.ncbi.nlm.nih.gov/29038287/

35a) In patients with milder renal phenotype and predominant liver #cysts, mutations in #GANAB, encoding the Glucosidase IIα Subunit, should be considered.
See 🔓 pubmed.ncbi.nlm.nih.gov/27259053/
See 🔓 pubmed.ncbi.nlm.nih.gov/27259053/

35b) Cystogenesis in #GANAB-related disease is probably related to a defect in PC1 maturation, because GIIα is essential for the maturation and surface and ciliary localization of #PC1. 

36) #Tuberous_sclerosis complex (#TSC) is an autosomal dominant genetic disease affecting multiple organs with wide variability in presentation. See 🔓 pubmed.ncbi.nlm.nih.gov/34399110/ 

37a) Renal disease is the second leading cause of early death (27.5%) in individuals with #TSC. Five different kidney lesions occur in TSC:
1⃣ benign #angiomyolipoma (70% of affected individuals)
2⃣ epithelial cysts (20%-30%)
(cont)
1⃣ benign #angiomyolipoma (70% of affected individuals)
2⃣ epithelial cysts (20%-30%)
(cont)
37b)
3⃣ #oncocytoma (benign adenomatous #hamartoma) (<1%)
4⃣ malignant #angiomyolipoma (<1%)
5⃣ renal cell #carcinoma (<3%)
See 🔓 pubmed.ncbi.nlm.nih.gov/24053982/.
3⃣ #oncocytoma (benign adenomatous #hamartoma) (<1%)
4⃣ malignant #angiomyolipoma (<1%)
5⃣ renal cell #carcinoma (<3%)
See 🔓 pubmed.ncbi.nlm.nih.gov/24053982/.

38) The skin is affected in virtually 100% of individuals with #TSC. Skin lesions can be recognized and guide the etiological approach.
See pubmed.ncbi.nlm.nih.gov/24053982/
See pubmed.ncbi.nlm.nih.gov/24053982/

39) Which genetic diagnosis would you consider in a family with prenatal lethality in male fetuses, and only females affected by polycystic kidneys, with a history of miscarriage ?
A) Fumarate hydratase mutation
B) Cobalamin C deficiency
C) #OFD1 mutation
D) Lowe syndrome
A) Fumarate hydratase mutation
B) Cobalamin C deficiency
C) #OFD1 mutation
D) Lowe syndrome
40a) The correct answer is #OFD1, a X-linked dominant #ciliopathy where kidney cysts occur in ~40% of cases. See 🔓 pubmed.ncbi.nlm.nih.gov/35112477/. This is a malformative syndrome is almost constant in OFD1 with characteristic oral anomalies:
40b) cleft lip/cleft palate or both, bifid or multilobed tongue, small hamartomas, multiple & hypertrophied lingual & labial frenula, missing central/lateral incisors, malpositioned & supernumerary teeth, & high susceptibility to caries. May also see skin & extremity anomalies. 

41) Parapelvic cysts should be recognized as they can ➡️erroneous dx of #hydronephrosis.
They generally do not require intervention, & this name may be misleading, as parapelvic cysts do not belong to kidney parenchymal cystic diseases.
See 🔓 pubmed.ncbi.nlm.nih.gov/29636957/
They generally do not require intervention, & this name may be misleading, as parapelvic cysts do not belong to kidney parenchymal cystic diseases.
See 🔓 pubmed.ncbi.nlm.nih.gov/29636957/

43) Did you identify renal #lymphangiectasia ? Well done ! Don’t miss this specific finding of benign perirenal cystic appearance.
See pubmed.ncbi.nlm.nih.gov/25709103/.
See pubmed.ncbi.nlm.nih.gov/25709103/.
44) In summary, this is a great flowchart and differential diagnosis table by @ecorneclegall, which I recommend to follow for the diagnosis of #cystic #kidneydisease
From pubmed.ncbi.nlm.nih.gov/30819518/

From pubmed.ncbi.nlm.nih.gov/30819518/


45) And you have just earned 0.5h 🆓CE/#CME from @academiccme ! I am @dguerrot and you should go to ckd-ce.com/adpkd5/ to claim your certificate!
🏆🥇🥳🎆
Thank you for following this 🧵. Now follow this feed--there's more education to come!
🏆🥇🥳🎆
Thank you for following this 🧵. Now follow this feed--there's more education to come!

• • •
Missing some Tweet in this thread? You can try to
force a refresh